INTRODUCTION
It is observed and clearly evident that the pharmacy profession has an important role in the frontline healthcare response to the coronavirus disease of 2019 (COVID-19) pandemic across all settings (Paudyal et al., 2020). As clinical pharmacists are involved in “direct patient care,” they are at a similar high risk during this pandemic as physicians, nurses, and other healthcare providers (Bauman, 2020). It is great to notice that physicians and nurses received many appropriate and well-deserved tributes in the media for their heroic efforts in caring for patients with COVID-19 (Erstad, 2021). A number of clinical pharmacists were involved as caring and competent practitioners in the daily care of these patients; however, they were often overlooked by the other heroes on the front line and have received less attention (Barlow et al., 2020; Bauman, 2020; Erstad, 2021).
Clinical pharmacists were proactive and fulfilled an essential service during the COVID-19 pandemic by working in the frontline along with other healthcare providers to ensure the best possible outcomes for the patients they served (Bauman, 2020; Ferguson et al., 2020; Visacri et al., 2021). While they have taken a range of service adaptations and adoption of novel roles, they were invisible heroes (Bauman, 2020; Paudyal et al., 2020). One study, however, showed a positive perception of the general population about pharmacists in different sectors and the services they provided during the pandemic (Alhamad et al., 2021). A wide range of skills and knowledge were taken up for effective crisis, which included clinical expertise, education, data analysis, health informatics infrastructure, and inventory management in times of surging medication use and manufacturer shortages (Ferguson et al., 2020).
The aim of this review is to summarize the literature related to the challenges faced by clinical pharmacists and the opportunities that evolved while providing general and specialized services during COVID-19 pandemic.
LITERATURE SEARCH
A literature search in PubMed was conducted to evaluate relevant studies published in English language. Only articles that discussed the roles performed, challenges, and opportunities experienced specifically by clinical pharmacists during COVID-19 pandemic were reviewed. If a paper discussed pharmacists from different sectors, only the part that stated the roles of clinical pharmacists was reviewed.
Challenges and opportunities for clinical pharmacists
General clinical pharmacists
As pharmacists in other sectors were impacted by COVID-19 pandemic, clinical pharmacists had their share of the burden (Table 1). One of the challenges encountered by clinical pharmacists included shifting roles and reassignment. For example, general clinical pharmacists were mobilized to critical care units or to the main hospital pharmacy to cover the shortage and assist with general hospital pharmacy operations (Cheong, 2020; Damuzzo et al., 2021; Johnston et al., 2020). Another major challenge was the interruptions of routine clinical services by withdrawing the clinical pharmacists from inpatient wards to reduce the risk of infection, as well as suspending ambulatory care services in outpatient clinics (Cheong, 2020; Paudyal et al., 2020).
As the literature on COVID-19 pharmacotherapy was rapidly changing with the controversy on using hydroxychloroquine, lopinavir/ritonavir, tocilizumab, and other agents, clinical pharmacists were faced with an increased demand on consultations regarding safety and efficacy of COVID-19 therapy both during and after hours or during teleconferences with other healthcare providers. As such, having to remain alert to every update on the management based on the hurriedly emerging literature and keeping up with its pace while carefully appraising and interpreting the evidence was a necessity (Al-Quteimat Om Msc et al., 2021; Cheong, 2020; Paudyal et al., 2020; Ying et al., 2021). Contributing to this literature was also part of the increased workload as clinical pharmacists participated in some of the published and ongoing clinical trials on COVID-19 (Danelich et al., 2021; Meng et al., 2020; Paudyal et al., 2020). What may have made the burnout more challenging in many cases is that it came on top of an already present high burnout prior to the pandemic (Johnston et al., 2020; Manohar et al., 2021).
Despite these challenges, numerous opportunities have elicited the critical role of clinical pharmacists in pandemics and public healthcare emergencies (Table 2). Some major examples in the inpatient setting included the utilization of advanced technology to provide remote counseling to healthcare providers (telehealth services), remote therapeutic drug monitoring (TDM) (telemonitoing) of hospitalized patients, and virtual rounding (Aburas et al., 2020; Allison et al., 2021; Arain et al., 2021; Aruru et al., 2021; Bhat and Kehasse, 2020; Danelich et al., 2021; Herzik et al., 2021; Li et al., 2021; Marchese et al., 2021; Meng et al., 2020; Muflih et al., 2021; Song et al., 2021; Surapat et al., 2021; Thomas et al., 2021; Wieruszewski et al., 2021; Zheng et al., 2021; Zhou et al., 2021). One hospital described a technology named Connect Care Pro, which was utilized during the pandemic (Kjerengtroen et al., 2020). The technology comprises a high-definition television, camera, and a two-way audio speaker. These devices were installed in hospitalized patients’ rooms, where it allowed healthcare providers, including clinical pharmacists, to access the rooms remotely to communicate with patients and access drug infusion rates on intravenous (IV) infusion pumps. This technology was also connected to the electronic medication record, which helped the pharmacists providing direct care via evaluating the list of drugs the patients are receiving.
Clinical pharmacists were also involved in institutional emergency preparedness planning and training (Merks et al., 2021; Waldron et al., 2021). During the tough time of the pandemic, a provision of 24/7 service was necessary to ensure an uninterrupted service. Changes in work schedules of clinical pharmacists in order to provide 24/7 consultation services while decreasing work burnout and limit exposure to sick patients was also one of the strategies developed by clinical pharmacists, where a pharmacist would alternate between 2 weeks of on-site services and 2 weeks of off-site services (Moye et al., 2021). Other institutions also developed other pharmacy staffing plans to cope with the hospital’s needs during the pandemic to ensure continuous provisions of services (Arain et al., 2021; de Val et al., 2021; Yerram et al., 2021). To minimize duplication of efforts and avoid coverage gaps, clinical pharmacists were also assigned clear roles and responsibilities. Regardless of their specialty, clinical pharmacy specialists were repurposed to assist with clinical pharmacy coverage of COVID-19 admitted patients in addition to their standard job responsibilities. Such uninterrupted service was also achieved by involving clinical pharmacy residents, general or specialized, to be on-call or to alternate with clinical pharmacy staff in covering evening or night shifts (Faine et al., 2020).
In addition, patients with acute respiratory distress syndrome who were placed on extracorporeal membrane oxygenation (ECMO) had issues with drug distribution for drugs that are highly lipophilic or have high protein binding tendency due to the possibility of adsorption to the ECMO circuit leading to subtherapeutic plasma concentration (Cheng et al., 2018). Therefore, clinical pharmacists had an essential role in monitoring patients receiving such drugs for response and possibility of dose adjustment (Surapat et al., 2021). Same applied to drugs removed by hemadsorption, which is an adjunctive therapeutic procedure used in COVID-19 patients experiencing cytokine storm (Surapat et al., 2021). For some difficult to acquire medications that showed some benefit in the management of severe COVID-19 cases like tocilizumab, anakinra, and baricitinib, clinical pharmacists reviewed patients’ laboratories, such as ferritin and C-reactive protein in persistently febrile patients to determine eligibility for therapy and then referral to the respective service (critical care, immunology, or rheumatology) (Ferguson et al., 2020; Gross et al., 2020). In order to limit the unnecessary exposure of nursing staff to COVID-19 inpatients, clinical pharmacists innovated a strategy to administer inhaled medications using IV extension sets; hence, pumps could be placed outside the patients’ room, where medications can be timed (Gross et al., 2020).
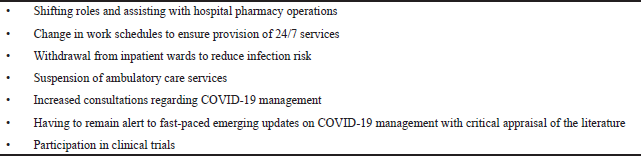 | Table 1. Summary of challenges encountered by clinical pharmacists during COVID-19 pandemic. [Click here to view] |
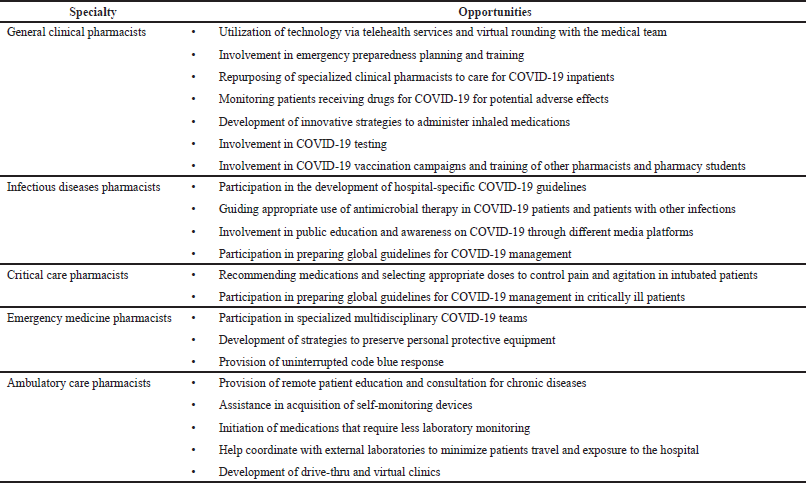 | Table 2. Opportunities arose for clinical pharmacists of various specialties during COVID-19 pandemic. [Click here to view] |
As COVID-19 was associated with coagulopathy and increased risk for venous thromboembolism, clinical pharmacists were on board to provide counseling on the use of anticoagulants, as well as dose adjustment and TDM (such as INR in patients prescribed warfarin and anti-Xa activity in obese and renally impaired patients) (Surapat et al., 2021). Furthermore, clinical pharmacists continuously monitored adverse drug reactions and drug–drug interactions and assessed eligible patients to receive anticoagulants, especially with drugs being trialed for COVID-19 (Arain et al., 2021; Gourieux et al., 2021; Perez et al., 2021; Skalafouris et al., 2021; Surapat et al., 2021; Ying et al., 2021). For example, checking QTc interval at baseline and later in patients treated with hydroxychloroquine, as well as checking for drug–drug interactions with the protease inhibitors (lopinavir/ritonavir) although these drugs are no longer recommended for COVID-19 management.
Pharmacists were also involved in testing for COVID-19 early in the pandemic where licensed pharmacists in several countries were authorized to order and conduct tests for SARS-CoV-2 (Jordan et al., 2021; U.S. Department of Health & Human Services, 2020). Furthermore, with the evolvement of COVID-19 vaccines, pharmacists played a vital role in the vaccination campaigns. Those who were certified immunizers trained their fellow pharmacists and pharmacy trainees on the proper administration techniques, post-vaccination counseling, monitoring, and reporting of adverse reactions, as well as management of severe allergic reactions (Andrade et al., 2021; Jordan et al., 2021; Merks et al., 2021; Patel et al., 2021; Srirangan et al., 2021).
All these examples and others resulted in the recognition of the paramount role a clinical pharmacist plays as a member of the multidisciplinary team during the pandemic.
Specialized clinical pharmacists
Several important roles were also revealed during this crisis for specialized clinical pharmacists, such as infectious diseases and critical care pharmacists (Table 2). Many hospitals created COVID-19 multidisciplinary teams that included infectious diseases pharmacists as essential team members to provide guidance on therapy based on the updated literature (Bhat et al., 2020; Chahine, 2020; Danelich et al., 2021; Hussain et al., 2020; Song et al., 2021). Infectious diseases pharmacists were also a part of committees that developed hospital-specific COVID-19 guidelines, which were communicated to the chairs of different departments (such as medicine and critical care) to be included in their daily briefings and educational sessions (Arain et al., 2021; Aruru et al., 2021; Ferguson et al., 2020). Such pharmacists also had a huge impact in directing the appropriate use of antibiotics and antivirals in COVID-19 patients and patients with other infections (Al-Quteimat Om Msc et al., 2021; Ashiru-Oredope et al., 2021; Goff et al., 2020). They also continued to provide antimicrobial stewardship services via virtual rounds and encouraging testing for procalcitonin to help distinguish between viral and bacterial infections; hence, selecting the appropriate antimicrobial therapy accordingly (Ashiru-Oredope et al., 2021; Thong et al., 2021). Additionally, many infectious diseases pharmacists were involved in public education and awareness on COVID-19 through different media platforms, such as TVs, radio, and social media (Aruru et al., 2021; Ying et al., 2021).
Likewise, critical care pharmacists remained invaluable team members caring for critically ill COVID-19 patients and coordinated between the intensive care unit (ICU) and the hospital pharmacy (Ferguson et al., 2020; Lemtiri et al., 2020; Wang et al., 2021). In the ICU, critical care pharmacists worked with physicians and nurses in recommending medications and selecting the right doses to control intubated patients’ pain and agitation (Traynor, 2020). They also helped with dose adjustment depending on patients’ responses, laboratory results, body weight, renal or hepatic impairment, as well as the need for renal replacement therapy, such as hemodialysis or continuous renal replacement therapy (Gurnani et al., 2021; Surapat et al., 2021; Traynor, 2020). One retrospective study identified 470 interventions done by pharmacists to critically ill patients within less than 3 months during the pandemic (Alwhaibi et al., 2021). Most of these interventions pertained to suggesting alternatives to drugs on shortage. Other interventions involved correction of dosing regimens, drug class duplicates, and provision of drug information services.
An evolving role for emergency medicine pharmacists became prominent during the pandemic, where in one institution (University of Iowa Hospitals and Clinics, Iowa City, IA) they served on a team named “COVID-19 airway team” (Faine et al., 2020). This team encompassed other healthcare members, including an anesthesiologist or emergency medicine physician, a senior medical resident, a registered nurse, and a respiratory therapist. In this team, emergency medicine pharmacists provided the following services: Development of intubation medication kit (neuromuscular blocking agents, sedatives, analgesics, and vasopressors), facilitation of rapid delivery of intubation medications, evaluation of patient’s medical history and vital signs to ensure appropriate dosing, preparation of these medications, and documentation of interventions and recommendations made during the intubation process. In another institution (Mayo Clinic, Rochester, MN), emergency medicine pharmacists developed strategies to preserve personal protective equipment and limit exposure to COVID-19 in patients placed in isolation. They anticipated the needs of patients as much as possible, delivering medications in the most finalized dosage forms, priming the IV lines, and programming the pump infusion prior to medication delivery to the room (Wieruszewski et al., 2021). Uninterrupted code blue response was provided by two clinical pharmacists in one institution, where the responding pharmacists participated by preparing the medications and providing counseling to the providers who were inside the patient room via mobile phone (Danelich et al., 2021).
In the outpatient setting, clinical pharmacists, particularly pharmacists specialized in ambulatory care, pharmacotherapy, and cardiology, provided remote patient education and consultation for chronic diseases (Badr et al., 2021; Bhat et al., 2020; Bhat and Kehasse, 2020; Chahine, 2020; Do et al., 2021; Elnaem et al., 2021; Marchese et al., 2021; Moreau, 2021; Surapat et al., 2021; Thorakkattil et al., 2021). They also assisted in acquiring self-monitoring devices, and initiated medications that require less laboratory monitoring to keep the patients at home or if monitoring was needed, they helped coordinating with external laboratories to minimize patients travel and exposure to the hospital (Bhat and Kehasse, 2020; Surapat et al., 2021). One key service that was modified during the pandemic was anticoagulation monitoring and adjustment of warfarin therapy. Some institutions developed a drive-thru curbside clinics for counseling and monitoring of patients on warfarin (Moreau, 2021; Truong et al., 2021). Another institution developed virtual clinic that was shown to be effective as face-to-face consultation (Al Ammari et al., 2021). Other institutions evaluated patients for transitioning from warfarin therapy to direct oral anticoagulants that do not require frequent monitoring, thus limiting patients’ visits. The results of a study that implemented this strategy showed that this short-term switch did not impact the efficacy or safety of chronic management of warfarin therapy (Cope et al., 2021). In patients with diabetes, 11 studies showed positive clinical outcomes following telepharmacy services provided by ambulatory care pharmacists, where telephone calls were the mostly used technology followed by electronic messages (Iftinan et al., 2021). Most of the services included providing patient counseling and monitoring medication adherence. A study from a transplant clinic evaluated the services provided by ambulatory transplant pharmacists during the pandemic (Park et al., 2021). Within a seven-month period, 385 virtual clinic visits were conducted with lung transplant recipients with more than 890 interventions made, most of which were related to medications errors and involved patient education. Notably, more than 55% of these interventions demonstrated value of clinical pharmacy services.
Moreover, several national and international pharmacy societies and organizations invited clinical pharmacists, especially those specialized in infectious diseases, to participate in the development of guidelines or protocols on COVID-19 management and monitoring for their fellow pharmacists and other pharmacy employees (Goff et al., 2020; Li et al., 2021). On a more global basis, clinical pharmacists were also included in taskforces of national and international COVID-19 guidelines, namely, the Infectious Diseases Society of America Guidelines on the treatment and management of patients with COVID-19, the Surviving Sepsis Campaign: guidelines on the management of critically ill adults with COVID-19, and the US National Institute of Health COVID-19 treatment guidelines (Alhazzani et al., 2020; Bhimraj et al., 2020; National Institute of Health, 2020).
FUTURE DIRECTIONS AND RECOMMENDATIONS
As demonstrated from the vast majority of the discussed studies, pharmacists had invaluable roles as members of the healthcare team. As many lessons have been learned from this pandemic, many of the changes in practice made and developed could be utilized at times of crises, whether they are health or natural, such as the development of work schedules to provide uninterrupted 24/7 service and the provision of telehealth services to inpatients and outpatients. Such big roles played by clinical pharmacists should be emphasized, especially in areas where clinical pharmacists might be underutilized (Assiri et al., 2021). We also suggest that clinical pharmacy training and education during the undergraduate pharmacy programs should include a part on emergency preparedness and planning in times of disasters. As there is a plethora of papers that discussed the contribution of pharmacists from all sectors (clinical, hospital, community, etc) during COVID-19 pandemic, this training and education could include a summary of this literature.
As life returns to normal, face-to-face clinic visits are returning, as well. One study reported significant decrease in no shows and cancellations (Thomas et al., 2021). While many patients benefited from telepharmacy services provided by ambulatory care pharmacists, one study found that medication-related problems were significantly more identified during face-to-face encounter with patients than during virtual clinic visits when the number of medication-related problems was compared between the pre-pandemic time and during the pandemic (McNamara et al., 2021). However, this was less significant only with patients who were not diabetic. The major reason behind this difference was the lack of access to technology or training by many of the patients making virtual clinic visits a difficult task. As such, it is suggested that one or more of the follow up visits be made virtually to train the patient or their caregiver on the use of technology and provide a detailed manual as such technology may be needed in the case of any crisis that may hinder access to direct healthcare. This is also helpful to make patients who may not feel comfortable about telehealth visits get used to it as one study showed that such uncomfortable feeling was one of the limitations of virtual clinic visits during the pandemic (Segal et al., 2020).
CONCLUSION
It is pretty evident from the published literature that clinical pharmacists responded to the needs of the society during this unprecedented time to their best limits. Equally interesting are the new roles or activities they adopted in response to the situation, many of which may need to be continued after the end of the pandemic. The pandemic has brought to light the need for clinical pharmacists to be more prepared for such emergency situations and unprecedented times like other healthcare professionals. Along with all the positive findings observed with clinical pharmacy services during this time, there seems to be a lack of deserved recognition and importance from the media, administrations, and other sources. This calls for the need of clinical pharmacists to be even more proactive and press on the concerned parties to ensure that they receive the accolades that they deserve. However, this will not deter clinical pharmacists from carrying on with their relentless and substantial services with the ultimate aim of patient care for optimal outcomes.
AUTHOR CONTRIBUTIONS
JJ and AKT conducted the literature search and evaluation of articles for inclusion, whereas AKT extracted the information and summarized the findings.
The manuscript has been read and approved by both authors. Both authors are eligible to be an author as per the International Committee of Medical Journal Editors (ICMJE) guidelines.
FUNDING
There is no funding to report.
ETHICAL APPROVAL
This study does not involve experiments on animals or human subjects.
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
Aburas W, Alshammari TM. Pharmacists’ roles in emergency and disasters: COVID-19 as an example. Saudi Pharm J, 2020; 28(12):1797–816; doi:10.1016/j.jsps.2020.11.006 CrossRef
Al-Quteimat Om Msc B, Amer Am R.Ph M. SARS-CoV-2 outbreak: how can pharmacists help? Res Social Adm Pharm, 2021; 17(2):480–2; doi:10.1016/j.sapharm.2020.03.018 CrossRef
Al Ammari M, AlThiab K, AlJohani M, Sultana K, Maklhafi N, AlOnazi H, Maringa A. Tele-pharmacy anticoagulation clinic during COVID-19 pandemic: patient outcomes. Front Pharmacol, 2021; 12:652482; doi:10.3389/fphar.2021.652482 CrossRef
Alhamad H, Abu-Farha R, Albahar F, Jaber D. Public perceptions about pharmacists’ role in prescribing, providing education and delivering medications during COVID-19 pandemic era. Int J Clin Pract, 2021; 75(4):e13890. doi:10.1111/ijcp.13890 CrossRef
Alhazzani W, Moller MH, Arabi YM, Loeb M, Gong MN, Fan E, Oczkowski S, Levy MM, Derde L, Dzierba A, Du B, Aboodi M, Wunsch H, Cecconi M, Koh Y, Chertow DS, Maitland K, Alshamsi F, Belley-Cote E, Greco M, Laundy M, Morgan JS, Kesecioglu J, McGeer A, Mermel L, Mammen MJ, Alexander PE, Arrington A, Centofanti JE, Citerio G, Baw B, Memish ZA, Hammond N, Hayden FG, Evans L, Rhodes A. Surviving sepsis campaign: guidelines on the management of critically ill adults with coronavirus disease 2019 (COVID-19). Intensive Care Med, 2020; 46(5):854–87; doi:10.1007/s00134-020-06022-5 CrossRef
Allison A, Shahan J, Goodner J, Smith L, Sweet C. Providing essential clinical pharmacy services during a pandemic: virtual video rounding and precepting. Am J Health Syst Pharm, 2021; 78(17):1556–8; doi:10.1093/ajhp/zxab208 CrossRef
Alwhaibi RA, Alrwaished A, Binobydaan SM, Alawwad S, Wajid S, Bablghaith S, Alghadeer S, Al Arifi MN. Role of pharmacist during COVID-19 pandemic: a retrospective study focused on critically ill COVID-19 patients. Saudi Pharm J, 2021; 29(9):1050–5; doi:10.1016/j.jsps.2021.07.010 CrossRef
Andrade J, Slaby M, DeAngelis J, Connors J, Truong J, Ciaramella C, DiGregorio R. Implementation of a pharmacist-led COVID-19 vaccination clinic at a community teaching hospital. Am J Health Syst Pharm, 2021; 78(12):1038–42; doi:10.1093/ajhp/zxab135 CrossRef
Arain S, Thalapparambath R, Al Ghamdi FH. COVID-19 pandemic: response plan by the Johns Hopkins Aramco Healthcare inpatient pharmacy department. Res Social Adm Pharm, 2021; 17(1):2009–11; doi:10.1016/j.sapharm.2020.05.016 CrossRef
Aruru M, Truong HA, Clark S. Pharmacy emergency preparedness and response (PEPR): a proposed framework for expanding pharmacy professionals’ roles and contributions to emergency preparedness and response during the COVID-19 pandemic and beyond. Res Social Adm Pharm, 2021; 17(1):1967–77; doi:10.1016/j.sapharm.2020.04.002 CrossRef
Ashiru-Oredope D, Kerr F, Hughes S, Urch J, Lanzman M, Yau T, Cockburn A, Patel R, Sheikh A, Gormley C, Chavda A, Vaghela T, Phillips C, Reid N, Brady A. Assessing the impact of COVID-19 on antimicrobial stewardship activities/programs in the United Kingdom. Antibiotics (Basel), 2021; 10(2):110; doi:10.3390/antibiotics10020110 CrossRef
Assiri A, Iqbal MJ, Gramish J, Assiri A, Meraya A, Alhossan A, Khobrani M. Pharmacists’ satisfaction with their involvement in the management of COVID-19 patients in Saudi Arabia. Saudi Pharm J, 2021; 29(1):85–90; doi:10.1016/j.jsps.2020.12.009 CrossRef
Badr AF, Ismail GA, Alghuraybi RH, Lahza RZ. Expanding pharmacist’s educational role using virtual and Social media portals before and during COVID-19 outbreak. Saudi Pharm J, [Online ahead of print], 2021; 29(6):533–8. CrossRef
Barlow B, Barlow A, Newsome AS. Comment on Gross and MacDougall “Roles of the clinical pharmacist during the COVID-19 pandemic”. J Am Coll Clin Pharm, 2020. doi:10.1002/jac5.1253
Bauman JL. Hero clinical pharmacists and the COVID-19 pandemic: overworked and overlooked. J Am Coll Clin Pharm, 2020; doi:10.1002/jac5.1246 CrossRef
Bhat S, Farraye FA, Moss AC. Impact of clinical pharmacists in inflammatory bowel disease centers during the COVID-19 pandemic. Am J Gastroenterol, 2020; 115(9):1532–3; doi:10.14309/ajg.0000000000000787 CrossRef
Bhat S, Kehasse A. Additional clinical pharmacists roles during COVID-19. J Am Coll Clin Pharm, 2020; doi:10.1002/jac5.1243
Bhimraj A, Morgan RL, Shumaker AH, Lavergne V, Baden L, Cheng VC, Edwards KM, Gandhi R, Muller WJ, O’Horo JC, Shoham S, Murad MH, Mustafa RA, Sultan S, Falck-Ytter Y. Infectious Diseases Society of America guidelines on the treatment and management of patients with COVID-19. Clin Infect Dis, 2020; doi:10.1093/cid/ciaa478 CrossRef
Chahine EB. The role of pharmacists in the fight against COVID-19. Sr Care Pharm, 2020; 35(7):286–91; doi:10.4140/TCP.n.2020.286 CrossRef
Cheng V, Abdul-Aziz MH, Roberts JA, Shekar K. Optimising drug dosing in patients receiving extracorporeal membrane oxygenation. J Thorac Dis, 2018; 10(Suppl 5):S629–41; doi:10.21037/jtd.2017.09.154 CrossRef
Cheong MWL. ‘To be or not to be in the ward’: the impact of COVID-19 on the role of hospital-based clinical pharmacists—a qualitative study. J Am Coll Clin Pharm, 2020; doi:10.1002/jac5.1315 CrossRef
Cope R, Fischetti B, Eladghm N, Elaskandrany M, Karam N. Outpatient management of chronic warfarin therapy at a pharmacist-run anticoagulation clinic during the COVID-19 pandemic. J Thromb Thrombolysis, 2021; doi:10.1007/s11239-021-02410-w CrossRef
Damuzzo V, Bertin R, Mengato D, Chiumente M, Rivano M, Palozzo AC. Hospital pharmacy response to COVID-19 pandemic in Italy: what we learned from the first outbreak wave. J Pharm Pract, 2021; 8971900211023643; doi:10.1177/08971900211023643 CrossRef
Danelich IM, Thomson L, Alberto J, Bonanni S, Buckler R, Foley J, Phillips S, Rall B, Thoma B, Merli G, Wordell, C. Adaptation of clinical pharmacy services to meet patient care needs during the COVID-19 pandemic. J Am Coll Clin Pharm, 2021; 4(3):364–71; doi:10.1002/jac5.1392 CrossRef
de Val J, Sohal G, Sarwar A, Ahmed H, Singh I, Coleman JJ. Investigating the challenges and opportunities for medicines management in an NHS field hospital during the COVID-19 pandemic. Eur J Hosp Pharm, 2021; 28(1):10–15; doi:10.1136/ejhpharm-2020-002364 CrossRef
Do T, Luon S, Boothe K, Stutsky M, Renauer M. Advancing ambulatory pharmacy practice through a crisis: Objectives and strategies used in an ambulatory care action team’s response to the COVID-19 pandemic. Am J Health Syst Pharm, 2021; 78(8):720–5; doi:10.1093/ajhp/zxab063 CrossRef
Elnaem MH, Cheema E. Caring for patients with diabetes during COVID-19 pandemic: Important considerations for pharmacists. Res Social Adm Pharm, 2021; 17(1):1938–41; doi:10.1016/j.sapharm.2020.05.030 CrossRef
Erstad BL. Caring for the COVID patient: a clinical pharmacist’s perspective. Ann Pharmacother, 2021; 55(3):413–4; doi:10.1177/1060028020954224 CrossRef
Faine BA, Carroll E, Decleene J, Zepeski A. Airway management team for patients with COVID-19: a new role for emergency medicine pharmacists. Am J Health Syst Pharm, 2020; 77(14):1102–3; doi:10.1093/ajhp/zxaa129 CrossRef
Ferguson NC, Quinn NJ, Khalique S, Sinnett M, Eisen L, Goriacko P. Clinical pharmacists: an invaluable part of the coronavirus disease 2019 frontline response. Crit Care Explor, 2020; 2(10):e0243; doi:10.1097/CCE.0000000000000243 CrossRef
Goff DA, Ashiru-Oredope D, Cairns KA, Eljaaly K, Gauthier TP, Langford BJ, Mahmoud SF, Messina AP, Michael UC, Saad T, Schellack, N. Global contributions of pharmacists during the COVID-19 pandemic. J Am Coll Clin Pharm, 2020; doi:10.1002/jac5.1329
Gourieux B, Reisz F, Belmas AS, Danion F, Fourtage M, Nai T, Reiter-Schatz A, Ruch Y, Walther J, Nivoix Y, Michel B. Prescribing practices of lopinavir/ritonavir, hydroxychloroquine and azithromycin during the COVID-19 epidemic crisis and pharmaceutical interventions in a French teaching hospital. Eur J Hosp Pharm, 2021; 28(5):242–7; doi:10.1136/ejhpharm-2020-002449 CrossRef
Gross A, MacDougall C. Roles of the clinical pharmacist during the COVID-19 pandemic. J Am Coll Clin Pharm, 2020; 3(3):564–6; doi:https://doi.org/10.1002/jac5.1231 CrossRef
Gurnani PK, Peksa GD, Panos NG, DeMott JM. Under the microscope: a look into the role of critical care pharmacists during the COVID-19 pandemic. J Pharm Pract, 2021; 8971900211013991; doi:10.1177/08971900211013991 CrossRef
Herzik KA, Bethishou L. The impact of COVID-19 on pharmacy transitions of care services. Res Social Adm Pharm, 2021; 17(1):1908–12; doi:10.1016/j.sapharm.2020.10.017 CrossRef
Hussain K, Ambreen G, Muzammil M, Raza SS, Ali U. Pharmacy services during COVID-19 pandemic: experience from a tertiary care teaching hospital in Pakistan. J Pharm Policy Pract, 2020; 13(1):74; doi:10.1186/s40545-020-00277-5 CrossRef
Iftinan GN, Wathoni N, Lestari K. Telepharmacy: a potential alternative approach for diabetic patients during the COVID-19 pandemic. J Multidiscip Healthc, 2021; 14:2261–73; doi:10.2147/JMDH.S325645 CrossRef
Johnston K, O’Reilly CL, Cooper G, Mitchell I. The burden of COVID-19 on pharmacists. J Am Pharm Assoc (2003), 2020; doi:10.1016/j.japh.2020.10.013 CrossRef
Jordan D, Guiu-Segura JM, Sousa-Pinto G, Wang LN. How COVID-19 has impacted the role of pharmacists around the world. Farm Hosp, 2021; 45(2):89–95; doi:10.7399/fh.11652
Kjerengtroen S, Wilde SM, Fontaine GV, Forbush KM, Van Gorder CM, Wohlt P. COVID-19 preparedness: Clinical pharmacy services remote staffing in a quaternary, level I trauma and comprehensive stroke center. Am J Health Syst Pharm, 2020; 77(15):1250–6; doi:10.1093/ajhp/zxaa132 CrossRef
Lemtiri J, Matusik E, Cousein E, Lambiotte F, Elbeki N. The role of the critical care pharmacist during the COVID-19 pandemic. Ann Pharm Fr, 2020; 78(6):464–8; doi:10.1016/j.pharma.2020.09.001 CrossRef
Li H, Zheng S, Liu F, Liu W, Zhao R. Fighting against COVID-19: Innovative strategies for clinical pharmacists. Res Social Adm Pharm, 2021; 17(1):1813–8; doi:10.1016/j.sapharm.2020.04.003 CrossRef
Manohar KN, Parashar N, Kumar CRS, Verma V, Rao S, Sekhar Y, Vijay Kumar K, Amalselvam A, Hemkumar TR, Prem Kumar BN, Sridhar K, Pradeep Kumar S, Sangeeta K, Shivam, Kumar C, Judith. Prevalence and severity of secondary traumatic stress and optimism in Indian health care professionals during COVID-19 lockdown. PLoS One, 2021; 16(9):e0257429; doi:10.1371/journal.pone.0257429 CrossRef
Marchese M, Heintzman A, Pasetka M, Charbonneau F, DeAngelis C, Peragine C. Development of a process map for the delivery of virtual clinical pharmacy services at Odette Cancer Centre during the COVID-19 pandemic. J Oncol Pharm Pract, 2021; 27(3):650–7; doi:10.1177/1078155221991202 CrossRef
McNamara A, Zhao M, Lee SY. Evaluating the primary care clinical pharmacist visit transition to telehealth during the COVID-19 pandemic by comparing medication related problems from telehealth visits and in-person visits. J Am Coll Clin Pharm, 2021; 4(8):914–23; doi:10.1002/jac5.1487 CrossRef
Meng L, Huang J, Qiu F, Sun S. Roles of the Chinese clinical pharmacist during the COVID-19 pandemic. J Am Coll Clin Pharm, 2020; doi:10.1002/jac5.1274
Merks P, Jakubowska M, Drelich E, Swieczkowski D, Bogusz J, Bilmin K, Sola KF, May A, Majchrowska A, Koziol M, Pawlikowski J, Jaguszewski M, Vaillancourt R. The legal extension of the role of pharmacists in light of the COVID-19 global pandemic. Res Social Adm Pharm, 2021; 17(1):1807–12; doi:10.1016/j.sapharm.2020.05.033 CrossRef
Moreau C. The pharmacist as part of the primary care team during the COVID-19 pandemic. J Am Board Fam Med, 2021; 34(Suppl):S21–5; doi:10.3122/jabfm.2021.S1.200180 CrossRef
Moye RA, Mason K, Flatt A, Faircloth B, Livermore J, Brown B, Furr A, Starnes C, Yates JR, Hurt R. Emergency preparation and mitigation for COVID-19 response in an integrated pharmacy practice model. Am J Health Syst Pharm, 2021; 78(8):705–11; doi:10.1093/ajhp/zxab015 CrossRef
Muflih SM, Al-Azzam S, Abuhammad S, Jaradat SK, Karasneh R, Shawaqfeh MS. Pharmacists’ experience, competence and perception of telepharmacy technology in response to COVID-19. Int J Clin Pract, 2021; 75(7):e14209; doi:10.1111/ijcp.14209 CrossRef
National Institute of Health. COVID-19 treatment guidelines. The National Institutes of Health, Bethesda, MD, 2020. Available via https://covid19treatmentguidelines.nih.gov/
Park L, Kim JH, Waldman G, Marks CR, Clark JE. Impact analysis of virtual ambulatory transplant pharmacists during COVID-19. J Am Coll Clin Pharm, 2021; 4(8):978–87; doi:10.1002/jac5.1488 CrossRef
Patel C, Dalton L, Dey A, Macartney K, Beard F. Letter: impact of the COVID-19 pandemic on pharmacist-administered vaccination services. Res Social Adm Pharm, 2021; 17(1):2040–1; doi:10.1016/j.sapharm.2020.08.021 CrossRef
Paudyal V, Cadogan C, Fialova D, Henman MC, Hazen A, Okuyan B, Lutters M, Stewart D. Provision of clinical pharmacy services during the COVID-19 pandemic: experiences of pharmacists from 16 European countries. Res Social Adm Pharm, 2020; 17(8):1507–17; doi:10.1016/j.sapharm.2020.11.017 CrossRef
Perez M, Masse M, Deldicque A, Beuscart JB, De Groote P, Desbordes J, Fry S, Musy E, Odou P, Puisieux F, Lambert M, Scherpereel A, Decaudin B. Analysis of clinical pharmacist interventions in the COVID-19 units of a French university hospital. Eur J Hosp Pharm, 2022; 29(e1):e30–5; doi:10.1136/ejhpharm-2020-002542 CrossRef
Segal EM, Alwan L, Pitney C, Taketa C, Indorf, A., Held, L., Lee KS, Son M, Chi M, Diamantides E, Gosser, R. Establishing clinical pharmacist telehealth services during the COVID-19 pandemic. Am J Health Syst Pharm, 2020; 77(17):1403–8; doi:10.1093/ajhp/zxaa184 CrossRef
Skalafouris C, Samer C, Stirnemann J, Grosgurin O, Eggimann F, Grauser D, Reny JL, Bonnabry P, Guignard, B. Electronic monitoring of potential adverse drug events related to lopinavir/ritonavir and hydroxychloroquine during the first wave of COVID-19. Eur J Hosp Pharm, 2021; doi:10.1136/ejhpharm-2020-002667 CrossRef
Song Z, Hu Y, Zheng S, Yang L, Zhao R. Hospital pharmacists’ pharmaceutical care for hospitalized patients with COVID-19: recommendations and guidance from clinical experience. Res Social Adm Pharm, 2021; 17(1):2027–31; doi:10.1016/j.sapharm.2020.03.027 CrossRef
Srirangan K, Lavenue A. Helping Quebec pharmacists seize the vaccination service opportunity: the pharmacy best practice workshops. Pharmacy (Basel), 2021; 9(1); doi:10.3390/pharmacy9010051 CrossRef
Surapat B, Sungkanuparph S, Kirdlarp S, Lekpittaya N, Chunnguleum K. Role of clinical pharmacists in telemonitoring for patients with Coronavirus Disease 2019 (COVID-19). J Clin Pharm Ther, 2021; 46(1):236–9; doi:10.1111/jcpt.13293 CrossRef
Thomas AM, Baker JW, Hoffmann TJ, Lamb K. Clinical pharmacy specialists providing consistent comprehensive medication management with increased efficiency through telemedicine during the COVID19 pandemic. J Am Coll Clin Pharm, 2021; 4(8):934–8; doi:10.1002/jac5.1494 CrossRef
Thong KS, Selvaratanam M, Tan CP, Cheah MF, Oh HL, Lee PM, Chew CC, Chang CT, Lee JCY. Pharmacy preparedness in handling COVID-19 pandemic: a sharing experience from a Malaysian tertiary hospital. J Pharm Policy Pract, 2021; 14(1):61; doi:10.1186/s40545-021-00343-6 CrossRef
Thorakkattil SA, Nemr HS, Al-Ghamdi FH, Jabbour RJ, Al-Qaaneh AM. Structural and operational redesigning of patient-centered ambulatory care pharmacy services and its effectiveness during the COVID-19 pandemic. Res Social Adm Pharm, 2021; 17(1):1838–44; doi:10.1016/j.sapharm.2020.06.017 CrossRef
Traynor K. ICU pharmacist describes challenges in COVID-19 care. Am J Health Syst Pharm, 2020; 77(15):1183–4; doi:10.1093/ajhp/zxaa220 CrossRef
Truong L, Whitfield K, Nickerson-Troy J, Francoforte K. Drive-thru anticoagulation clinic: Can we supersize your care today? J Am Pharm Assoc (2003), 2021; 61(2):e65–7; doi:10.1016/j.japh.2020.10.016 CrossRef
U.S. Department of Health & Human Services. Guidance for Licensed Pharmacists, COVID-19 Testing, and Immunity under the PREP Act. U.S. Department of Health & Human Services, Washington, DC, 2020.
Visacri MB, Figueiredo IV, Lima TM. Role of pharmacist during the COVID-19 pandemic: a scoping review. Res Social Adm Pharm, 2021; 17(1):1799–806; doi:10.1016/j.sapharm.2020.07.003 CrossRef
Waldron KM, Schenkat DH, Rao KV, Campbell U. Application of emergency preparedness principles to a pharmacy department’s approach to a “black swan” event: the COVID-19 pandemic. Am J Health Syst Pharm, 2021; 78(7):552–5; doi:10.1093/ajhp/zxab004 CrossRef
Wang R, Kong L, Xu Q, Yang P, Wang X, Chen N, Li L, Jiang S, Lu X. On-ward participation of clinical pharmacists in a Chinese intensive care unit for patients with COVID-19: a retrospective, observational study. Res Social Adm Pharm, 2021; 17(1):1853–8; doi:10.1016/j.sapharm.2020.06.005 CrossRef
Wieruszewski ED, Mattson AE, Manuel FC, Brown CS. Optimizing emergency medicine pharmacists’ practice during the COVID-19 pandemic. J Pharm Pract, 2021; 8971900211004838; doi:10.1177/08971900211004838 CrossRef
Yerram P, Thackray J, Modelevsky LR, Land JD, Reiss SN, Spatz KH, Levoir AC, Pak TK, Dao PH, Buege MJ, Derespiris LM, Lau C, Orozco JS, Boparai M, Koranteng LA, Reichert KE, Yan SQ, Daukshus NP, Mathew S, Buie LW, Tizon RF, Freeswick S, Liu D, Harnicar S. Outpatient clinical pharmacy practice in the face of COVID-19 at a cancer center in New York City. J Oncol Pharm Pract, 2021; 27(2):389–94; doi:10.1177/1078155220987625 CrossRef
Ying W, Qian Y, Kun Z. Drugs supply and pharmaceutical care management practices at a designated hospital during the COVID-19 epidemic. Res Social Adm Pharm, 2021; 17(1):1978–83; doi:10.1016/j.sapharm.2020.04.001 CrossRef
Zheng SQ, Yang L, Zhou PX, Li HB, Liu F, Zhao RS. Recommendations and guidance for providing pharmaceutical care services during COVID-19 pandemic: a China perspective. Res Social Adm Pharm, 2021; 17(1):1819–24; doi:10.1016/j.sapharm.2020.03.012 CrossRef
Zhou C, Pavlakos R, Clark M, Jue VI, Clinard VB. Pharmacy telehealth services: perspectives from an academic medical center. J Pharm Pract, 2021; 8971900211030652; doi:10.1177/08971900211030652 CrossRef