INTRODUCTION
End-stage kidney disease (ESKD) is a chronic disorder that has attention globally due to its high morbidity and mortality (Cousin Sobrinho et al., 2020). Malfunction of the kidney brings about multiple clinical complications, such as hyperphosphatemia, hyperkalemia, hyperuricemia, hyperparathyroidism, hyperglycemia, hypertension, hypocalcemia, uremia, metabolic acidosis, anemia, and fluid overload (de Jager et al., 2009). The treatment effectiveness of hemodialysis patients depends on the adherence to hemodialysis sessions, fluid-diet control, and medication adherence (Alkatheri et al., 2014). Medication adherence is the most complex issue among these three factors because hemodialysis patients might receive about 10–12 types of medication with different names, indications, doses, frequencies, and administration times (Manley et al., 2004). Poor understanding of prescribed medication can lead to medication nonadherence and bring more risk than benefit. Besides, the patient’s self-experience of adverse drug reactions can cause negative beliefs about prescribed medication resulting in medication nonadherence (Cummings et al., 1982; Jin et al., 2008; Wileman et al., 2015). A previous study showed that a patient with positive beliefs about medicine less engaged in intentional medication nonadherence (Náfrádi et al., 2016).
The rate of medication nonadherence among hemodialysis patients was ranked from 12.5% to 98.6% based on previous studies (Ghimire et al., 2015). Clinicians should be aware of patient-, disease-, and medication-related factors associated with medication nonadherence (Ghimire et al., 2015). However, the psychosocial and behavioral factors should be focused on as well to address the problem of medication nonadherence (Ghimire et al., 2017). Indeed, previous studies showed that belief about medication was an important predictor of medication adherence in hemodialysis patients (Drangsholt et al., 2019; Horne et al., 2001). Medication nonadherence among hemodialysis patients was potentially modifiable by using psychoeducational or cognitive-behavioral interventions (Ghimire et al., 2017).
Patients’ medication beliefs have been extensively assessed in multiple chronic illnesses by using the Beliefs about Medicine Questionnaire (BMQ), a validated tool developed by Horne et al. (1999). The BMQ model assesses the medication beliefs in two domains which are BMQ-Specific and BMQ-General. BMQ-Specific evaluates patients’ beliefs about prescribed medication for their personal use, whereas BMQ-General assesses general beliefs about medicine. The Necessity-Concerns differential determined from BMQ-Specific was extensively used to categorize the patients’ attitudes into four groups: accepting, ambivalent, indifferent, and skeptical (Horne et al., 1999; Liu et al., 2017; Sipos et al., 2021). In the context of the Necessity-Concerns Framework, perceptions of high necessity with low concerns about the potential adverse effects of medication were associated with high medication adherence (Horne et al., 2013; Jamous et al., 2014). A meta-analysis revealed that the Necessity-Concerns Framework could help clinicians identify patients’ perception about the medication necessity and understand the patients’ degree of worry about the potential side effects of the medication (Horne et al., 2013).
In Malaysia, the pharmacist-led medication therapy adherence clinic (MTAC) is well established in government hospital settings (Pharmaceutical Service Program, 2019). The MTAC aims to improve patient medication knowledge and adherence by providing systematic medication counseling (Pharmaceutical Service Program, 2019). However, the medication beliefs perspective has not been incorporated in medication counseling for hemodialysis patients in Malaysia due to the lack of local supportive data. Hence, this study aimed to assess the association between medication beliefs (by using the Necessity-Concerns Framework) and medication adherence among Malaysian hemodialysis patients. The study findings would guide the incorporation of the medication beliefs perspective in medication counseling for Malaysian hemodialysis patients.
MATERIALS AND METHODS
Study design, site, and duration
A multicenter, cross-sectional study was conducted between September 2019 and January 2020 in eight hemodialysis centers in Penang state, Malaysia. The centers were conveniently selected, including one government hospital hemodialysis center and seven nongovernment hemodialysis centers. The study was approved by the Medical Research Ethics Committee, Ministry of Health Malaysia (Ethics Approval No. NMRR-19-280-46289).
Study participants and sampling method
The sample was enrolled by using purposive sampling. Patients who fulfilled the inclusion criteria were sampled. The inclusion criteria were ESKD patients aged more than 18 years and undergoing hemodialysis for at least 6 months. The patients who were cognitively and physically unstable were excluded.
Sample size
The sample size was determined by using the formula for prevalence study. The sample size was determined by using an estimation of 30% prevalence of medication nonadherence among hemodialysis patients from a previous Malaysian study (Chan et al., 2012). The calculated required sample size was 323 patients. With an estimation of an 85% response rate, 380 patients needed to be recruited.
Study instruments
A data collection form was used in the study. The data collection form consisted of demographic data, a five-item medication adherence report scale (MARS-5), and the BMQ. Baseline information such as demographic data and current medication list was obtained from the patient’s medical record. Meanwhile, a patient’s social history, medication adherence, and beliefs about medicine were obtained from the patient’s structured interview. A pilot test was conducted to examine the feasibility of the MARS-5 and BMQ prior to the data collection.
Medication adherence report scale
MARS-5 (Horne and Weinman, 1999) was used to assess medication adherence. The approval to use MARS-5 was obtained from the copyright holder. The reliability test for MARS-5 in a previous study showed a Cronbach’s alpha of 0.67–0.89 for hypertension, asthma, and diabetes mellitus patients (Chan et al., 2020). MARS-5 included five statements of nonadherence behavior, which are “forgetting,” “changing of dosage,” “stopping,” “skipping,” and “using medication less than what is prescribed.” The answers are on a five-point Likert scale. The patients indicated the frequency (“always,” “often,” “sometimes,” “rarely,” or “never”) for each question with ascending score from “always” (1 point) to “never” (5 points). A higher score of MARS-5 indicates high levels of medication adherence, with a maximum score of 25 (Horne and Weinman, 1999). The English version of MARS-5 was translated to the Malay language by using the forward-backward translation procedure in the present study.
Beliefs about Medicine Questionnaire
The BMQ is a reliable, validated tool to assess beliefs about medicine in patients with chronic diseases (Horne et al., 1999). The permission to use both the English (Horne et al., 1999) and Malay (Supramaniam et al., 2019) versions of the BMQ in this study was obtained from the copyright holder. A total of 10 questions in the questionnaire are scored on a 5-point Likert scale (where 1 = strongly disagree, 2 = disagree, 3 = uncertain, 4 = agree, and 5 = strongly agree). The BMQ-Specific is divided into subscales of Necessity and Concerns. The total scores for the Specific-Necessity and Specific-Concerns subscale range from 5 to 25, with the midpoint of 15. A higher score reflects higher beliefs in necessity and more concern, respectively. Considering the reliability of the BMQ, a previous study showed the Cronbach’s alpha values for each scale in kidney disease patients were 0.55 for Specific-Necessity and 0.73 for Specific-Concerns (Horne et al., 1999). In Malaysia, the internal consistency of the BMQ among diabetes mellitus and hypertensive patients was 0.75 and 0.86, respectively (Supramaniam et al., 2019; Tan et al., 2018).
Data collection
A preannouncement of the study to the patients was performed a day before the data collection. Written informed consent was obtained from all the patients before study participation. The data were collected during a researcher (the first author) administered structured interview. The interview was performed by a single researcher (the first author) at the time before the starting of the hemodialysis session.
Data analysis
All the data were processed with IBM Statistical Package for the Social Sciences® version 27.0. Data were tested for normality by using the Kolmogorov–Smirnov method. Categorical data such as demographic data were presented as frequency and percentage. The medication adherence score (MARS-5) was presented as the mean score. The scores of items in the Specific-Necessity and Specific-Concerns were presented as a percentage. The dependent variable was medication adherence, and the independent variables were demographic data and BMQ score. The differences in the medication adherence based on the patients’ demographic data were analyzed by using the Mann–Whitney U test and the Kruskal–Wallis test, whereas the association of the BMQ-Specific items with medication adherence was analyzed by using single linear regression, followed by multiple linear regression.
The Necessity-Concerns differential was determined by subtracting the total mean score of Specific-Concerns from the total mean score of Specific-Necessity. The score was on a differential varied from the lowest score of −20 to the highest score of +20 (Horne and Weinman, 1999; Liu et al., 2017). The Necessity-Concerns Framework was split at the midscale to form the four attitude groups which are accepting (a high necessity with low concerns), ambivalent (a high necessity with high concerns), indifferent (a low necessity with low concerns), and skeptical (a low necessity with high concerns) (Horne and Weinman, 1999; Horne et al., 2001). The differences between the attitude groups based on the MARS-5 score were analyzed by using the Kruskal–Wallis test. In all steps of analysis, p ≤ 0.05 was considered statistically significant.
RESULTS
Demographic characteristics of patients
Out of 380 patients who fulfilled the inclusion criteria, 55 patients disagreed with consenting to participate in the study. Hence, 325 patients were recruited and completed the study, corresponding to a response rate of 85.5%. The required sample size was achieved. The mean age of the patients was 60.18 ± 21.54 years, with 57.6% less than 65 years old. Additionally, 54.8% of the patients were male, and 57.2% were Chinese. Most (68.3%) of the patients were married. Slightly more than half (55.1%) of the patients had an education level of secondary school, and the majority (86.8%) were employed. The patients mostly received hemodialysis with a duration of 10 years or less (87.1%) and received 6–10 types of prescribed medications (58.2%). The median number of daily medications received by the patients was 9 (95% CI: 8.0–11.0). Among the demographic variables, age and number of prescribed medications showed significant differences in the MARS-5 score (Table 1). The patients with age ≥65 years had a significantly higher MARS-5 mean score than the patients with younger ages (18–44 years old). In terms of the number of prescribed medications, the patients who were prescribed 5 or fewer medications showed lower MARS-5 mean scores as compared to patients who received 6–10 and 11 or more prescribed medications, respectively (Table 1).
Necessity-Concerns Framework analysis
Figures 1 and 2 show the descriptive analysis of hemodialysis patients’ responses to the BMQ Specific-Necessity and Specific-Concerns. Most of the patients (88.0%) believed that their medication prevents them from becoming worse, and 85.5% of them agreed that their current health depends on the prescribed medication (Fig. 1). Considering the Specific-Concerns analysis, the worry about long-term side effects of medication was the main concern among the patients (36.3%). Meanwhile, 29.5% of the patients were worried about becoming too dependent on their prescribed medication (Fig. 2).
This study found that most patients perceived high necessity beliefs about their prescribed medication with a mean score of 18.42 ± 2.30 and low concerns about medication side effects with a mean score of 13.16 ± 3.13. The Necessity-Concerns differential showed a positive value of 5.26 ± 3.91. By analyzing whether the patient scored above or below the scale midpoint for both scales, this study found that 67.1% of hemodialysis patients were accepting, 26.5% were ambivalent, 3.7% were indifferent, and 2.8% were skeptical towards prescribed medication. Figure 3 showed that the rate of medication adherence was highest among the patients with accepting attitudes (75.8%), followed by ambivalent (19.2%), skeptical (3%), and indifferent (2%) ones.
Differences in MARS-5 score among the attitudinal groups
The four attitudinal groups of patients showed a significant difference in medication adherence based on the MARS-5 score (Table 2). The accepting group scored the highest mean score of 23.65 ± 1.65, followed by the ambivalent group (22.98 ± 1.92), skeptical group (23.33 ± 1.94), and indifferent group (22.50 ± 2.91). Post hoc analysis showed a significant difference in adherence between the accepting and ambivalent groups of patients.
Association of Necessity-Concerns Framework with medication adherence
The multiple linear regression analysis showed that the overall medication adherence in hemodialysis patients was positively associated with the Specific-Necessity score but negatively associated with the Specific-Concerns score (Table 3). The association between each BMQ-Specific item and medication adherence was further analyzed (Table 4). The belief of getting very sick without medications was a significant predictor of medication adherence (adjusted regression coefficient = 0.344; 95% CI: 0.113–0.576). Meanwhile, the worry about becoming heavily dependent on medications has a significant negative association with medication adherence (adjusted regression coefficient = −0.264, 95% CI: −0.469–0.059).
DISCUSSION
The present study revealed that hemodialysis patients of varied ages had a significant difference in medication adherence. This study showed a different trend from a previous study by Theofilou (2013), which found that hemodialysis patients aged over 65 years were less likely to take their medications as prescribed. This is because elderly patients are more prone to forgetfulness of taking medication, making it easier for them to encounter drug side effects (Moreira et al., 2008). However, the present study discovered that older patients had higher medication adherence than the younger-aged group. This finding could be attributed to the daily monitoring of elderly hemodialysis patients’ medication-taking behavior by the caregivers.
 | Table 1. Demographic characteristics, social history, and difference in MARS-5 score of the hemodialysis patients. [Click here to view] |
This study revealed an interesting finding that patients who were prescribed more medications had better adherence. These patients might have experienced complications of ESKD which led to the extra medication treatment. The extra medication might serve as a reminder to the patients to adhere to their treatment in order to avoid further severe complications. Nevertheless, a previous study showed a different trend that high pill load in hemodialysis patients was substantially associated with medication nonadherence (Neri et al., 2011). Besides, a recent study found that chronic kidney disease patients who consumed more than five medications per day had lower adherence (Bai et al., 2022). The patients’ nonadherence was due to a lack of tolerance for the complex regimen’s negative effects and drug interactions (Chiu et al., 2009).
In this study, hemodialysis patients showed a high level of awareness regarding the benefits of their prescribed medications. The majority of patients believe their medication keeps them from becoming worse, according to the Specific-Necessity analysis. Patients also believed that their current health was dependent on the medications they were taking. These positive views were also discovered in a prior study done among Norwegian hemodialysis patients (Drangsholt et al., 2019). The patients might have experienced recovery from the ESKD complications after taking their prescribed medications. A rapid deterioration of clinical outcomes might occur if the patient defaults on the medication treatments (Horne et al., 2001).
 | Figure 1. Percentage of patients expressing belief the need of their medication as indicated by responding agree or strongly agree to the Specific-Necessity items in the BMQ. [Click here to view] |
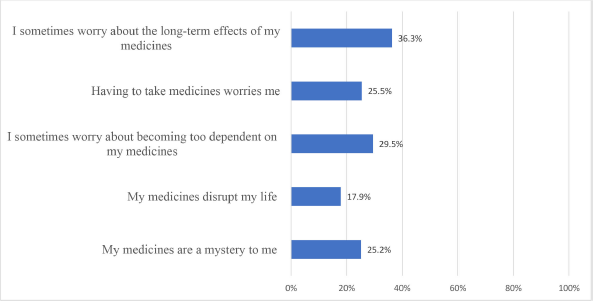 | Figure 2. Percentage of patients expressing concern the side effects of their medication as indicated by responding agree or strongly agree to the Specific-Concerns items in the BMQ. [Click here to view] |
The worries about long-term side effects and becoming too dependent on medications were the hemodialysis patients’ main concerns according to the Specific-Concerns analysis in this study. A study conducted in England found a similar finding that the dialysis patients’ erroneous beliefs about medication were always tempered with concern about long-term safety and medication dependence (Horne et al., 2001). Indeed, a more recent study showed that informing patients about known drug side effects and the countermeasures for dealing with them can help in enhancing the patients’ beliefs about long-term medication treatment (Bai et al., 2022). Thus, alleviating such concern among hemodialysis patients is one of the strategies for counseling intervention to improve their medication adherence.
The positive value of the Necessity-Concerns differential indicated that hemodialysis patients held beliefs that their medication brought about more benefits than side effects. This result reflects that the responding Malaysian hemodialysis patients have a good acceptance of their prescribed medication, which was consistent with previous studies involving patients with other chronic diseases (Gonzalez et al., 2007; Neame and Hammond, 2005; Wei et al., 2017). Additionally, this study found that the majority of hemodialysis patients had an accepting attitude with the highest medication adherence rate. However, the rate of medication adherence was lower in the ambivalent group of patients as their medication beliefs were tempered with worrying about the medication’s long-term adverse effects and medication dependence. A previous study showed that patients who are ambivalent about their medication might need proper medication counseling. In fact, healthcare providers need to always be alert to the patients’ history of side effects (Liu et al., 2017). In this study, only 3% of patients adhered to medications with a skeptical attitude. Patients with skepticism might not have good adherence until they experience the worsening symptoms of the disease (Liu et al., 2017). Meanwhile, the present study found that the patients with an indifferent attitude have the lowest adherence. This finding deviated from a study conducted among nondialysis ESKD patients, which reported that skeptical patients showed the lowest adherence score (Bai et al., 2022). The low medication adherence in patients with an indifferent attitude might be due to the poor understanding of their medication. Therefore, a good patient and healthcare provider relationship should be established to correct the misunderstanding of medication and reduce the negative beliefs about medication (Ghimire et al., 2017). Overall, the present study’s findings supported that the Necessity-Concerns Framework is a good predictor tool for medication adherence behavior in hemodialysis patients (Horne et al., 2013; Nie et al., 2019).
 | Figure 3. Rate of patients’ adherence according to the four attitudinal groups from the BMQ analysis. [Click here to view] |
 | Table 2. Differences in MARS-5 score among the attitudinal groups [Click here to view] |
The present study showed similar findings to studies from overseas that medication adherence in ESKD patients was positively associated with the Specific-Necessity score but negatively associated with the Specific-Concerns score (Bai et al., 2022; Horne et al., 2001). Medication adherence was significantly higher in patients with the belief that their condition would become worse without the prescribed medicines. This finding is valuable in the customization of medication counseling for hemodialysis patients. Counseling on the benefit of disease control by the medication would enhance hemodialysis patients’ adherence. Besides, the patients should be educated on the clinical complications of ESKD to further strengthen their adherence to the medication treatment. These complications include fatigue, fluid overload, electrolyte imbalance, and uncontrolled blood pressure (Saran et al., 2003). Meanwhile, medication adherence was found to be lower in patients worried about medication dependence. Patient counseling on the indication of each prescribed medication would address the misconception of medication dependence. When the patients clearly understand the indication, their confidence in taking their medications will improve.
 | Table 3. Association of the BMQ-Specific subscale with MARS-5 score in hemodialysis patients. [Click here to view] |
 | Table 4. Association of BMQ-Specific items with MARS-5 score in hemodialysis patients. [Click here to view] |
CONCLUSION
In conclusion, a positive belief in necessity with less concern about medication side effects was associated with medication adherence in hemodialysis patients. The Necessity-Concerns Framework is a useful tool to predict medication adherence behavior in hemodialysis patients. Targeted counseling should be customized for hemodialysis patients with negative beliefs about medications and potential nonadherence.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All the authors are eligible to be an author as per the international committee of medical journal editors (ICMJE) requirements/guidelines.
FUNDING
There is no funding to report.
CONFLICTS OF INTEREST
The authors report no financial or any other conflicts of interest in this work.
ETHICAL APPROVALS
The study was approved by the Medical Research Ethics Committee, Ministry of Health Malaysia (Ethics Approval No. NMRR-19-280-46289).
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
Alkatheri AM, Alyousif SM, Alshabanah N, Albekairy AM, Alharbi S, Alhejaili FF, Alsayyari AA, Qandil AM, Qandil AM. Medication adherence among adult patients on hemodialysis. Saudi J Kidney Dis Transpl, 2014; 25(4):762–8. CrossRef
Bai HH, Nie XJ, Chen XL, Liang NJ, Peng LR, Yao YQ. Beliefs about medication and their association with adherence in Chinese patients with non-dialysis chronic kidney disease stages 3-5. Medicine (Baltimore), 2022; 101(2):e28491. CrossRef
Chan AHY, Horne R, Hankins M, Chisari C. The medication adherence report scale: a measurement tool for eliciting patients’ reports of nonadherence. Br J Clin Pharmacol, 2020; 86(7):1281–8. CrossRef
Chan YM, Zalilah MS, Hii SZ. Determinants of compliance behaviours among patients undergoing hemodialysis in Malaysia. PLoS One, 2012; 7(8):e41362. CrossRef
Chiu YW, Teitelbaum I, Misra M, de Leon EM, Adzize T, Mehrotra R. Pill burden, adherence, hyperphosphatemia, and quality of life in maintenance dialysis patients. Clin J Am Soc Nephrol, 2009; 4(6):1089–96. CrossRef
Cousin Sobrinho EL, Duncan BB, Schmidt MI, GBD Chronic Kidney Disease Collaboration. Global, regional, and national burden of chronic kidney disease, 1990–2017: a systematic analysis for the Global Burden of Disease Study 2017. Lancet, 2020; 395(10225):709–33. CrossRef
Cummings KM, Becker MH, Kirscht JP, Levin NW. Psychosocial factors affecting adherence to medical regiments in a group of hemodialysis patients. Med Care, 1982; 20(6):567–80. CrossRef
de Jager DJ, Grootendorst DC, Jager KJ, van Dijk PC, Tomas LMJ, Ansell D, Collart F, Finne P, Heaf JG, De Meester J, Wetzels JFM, Rosendaal FR, Dekker F. Cardiovascular and noncardiovascular mortality among patients starting dialysis. JAMA, 2009; 302(16):1782–9. CrossRef
Drangsholt SH, Cappelen UW, von der Lippe N, Høieggen A, Os I, Brekke FB. Beliefs about medicines in dialysis patients and after renal transplantation. Hemodial Int, 2019; 23(1):117–25. CrossRef
Ghimire S, Castelino RL, Jose MD, Zaidi STR. Medication adherence perspectives in haemodialysis patients: a qualitative study. BMC Nephrol, 2017; 18(1):167. CrossRef
Ghimire S, Castelino RL, Lioufas NM, Peterson GM, Zaidi ST. Nonadherence to medication therapy in haemodialysis patients: a systematic review. PLoS One, 2015; 10(12):e0144119. CrossRef
Gonzalez JS, Penedo FJ, Llabre MM, Durán RE, Antoni MH, Schneiderman N, Horne R. Physical symptoms, beliefs about medications, negative mood, and long-term HIV medication adherence. Ann Behav Med, 2007; 34(1):46–55. CrossRef
Horne R, Chapman SC, Parham R, Freemantle N, Forbes A, Cooper V. Understanding patients’ adherence-related beliefs about medicines prescribed for long-term conditions: a meta-analytic review of the Necessity-Concerns Framework. PLoS One, 2013; 8(12):e80633. CrossRef
Horne R, Sumner S, Jubraj B, Weinman J, Frost S. Haemodialysis patients’ beliefs about treatment: implications for adherence to medication and fluid-diet restrictions. Int J Pharm Pract, 2001; 9(3):169–75. CrossRef
Horne R, Weinman J. Patients’ beliefs about prescribed medicines and their role in adherence to treatment in chronic physical illness. J Psychosom Res, 1999; 47(6):555–67. CrossRef
Horne R, Weinman J, Hankins M. The beliefs about medicines questionnaire: the development and evaluation of a new method for assessing the cognitive representation of medication. Psychol Health, 1999; 14(1):1–24. CrossRef
Jamous RM, Sweileh WM, El-Deen Abu Taha AS, Zyoud SH. Beliefs about medicines and self-reported adherence among patients with chronic illness: a study in Palestine. J Family Med Prim Care, 2014; 3(3):224–9. CrossRef
Jin J, Sklar GE, Min Sen Oh V, Chuen Li S. Factors affecting therapeutic compliance: a review from the patient’s perspective. Ther Clin Risk Manag, 2008; 4(1):269–86. CrossRef
Liu HX, Teng S, Lin XH, Shang YB, Wang L, Zhang J, Zang YJ. The application of the Necessity-Concerns Framework in investigating adherence and beliefs about immunosuppressive medication among Chinese liver transplant recipients. Chin Nurs Res, 2017; 4(1):14–7. CrossRef
Manley HJ, Garvin CG, Drayer DK, Reid GM, Bender WL, Neufeld TK, Hebbar S, Muther RS. Medication prescribing patterns in ambulatory haemodialysis patients: comparisons of USRDS to a large not-for-profit dialysis provider. Nephrol Dial Transplant, 2004; 19(7):1842–8. CrossRef
Moreira LB, Fernandes PF, Mota RS, Monte FS, Galvão RIM, Sousa DF, Martins AMC. Medication noncompliance in chronic kidney disease. J Nephrol, 2008; 21(3):354–62.
Náfrádi L, Galimberti E, Nakamoto K, Schulz PJ. Intentional and unintentional medication non-adherence in hypertension: the role of health literacy, empowerment and medication beliefs. J Public Health Res, 2016; 5(3):762. CrossRef
Neame R, Hammond A. Beliefs about medications: a questionnaire survey of people with rheumatoid arthritis. Rheumatology (Oxford), 2005; 44(6):762–7. CrossRef
Neri L, Martini A, Andreucci VE, Gallieni M, Rey LAR, Brancaccio D, MigliorDialisi Study Group. Regimen complexity and prescription adherence in dialysis patients. Am J Nephrol, 2011; 34(1):71–6. CrossRef
Nie B, Chapman SCE, Chen Z, Wang X, Wei L. Utilization of the beliefs about medicine questionnaire and prediction of medication adherence in China: a systematic review and meta-analysis. J Psychosom Res, 2019; 122:54–68. CrossRef
Pharmaceutical Service Program. Nephrology MTAC protocol. 2nd edition, Ministry of Health Malaysia, 2019. [Online] Available via https://www.pharmacy.gov.my/v2/en/documents/nephrology-mtac-protocol-second-edition-2019.html (Accessed 15 January 2020).
Saran R, Bragg-Gresham JL, Rayner HC, Goodkin DA, Keen ML, Van Dijk PC, Kurokawa K, Piera L, Saito A, Fukuhara S, Young EW, Held PJ, Port FK. Nonadherence in hemodialysis: associations with mortality, hospitalization, and practice patterns in the DOPPS. Kidney Int, 2003; 64(1):254–62. CrossRef
Sipos M, Farcas A, Prodan N, Mogosan C. Relationship between beliefs about medicines and adherence in elderly patients with cardiovascular and respiratory diseases: a cross-sectional study in Romania. Patient Educ Couns, 2021; 104(4):911–8. CrossRef
Supramaniam P, Aisyah A, Chong L. Reliability and validity of Beliefs on Medicine Questionnaire (BMQ) in diabetes mellitus patients: Malay translated version. Int J Sci Res, 2019; 9(2):66–73. CrossRef
Tan CS, Hassali MA, Neoh CF, Saleem F, Horne R. Cultural adaptation and inguistic validation of the Beliefs about Medicines Questionnaire in Malaysia. Value Health Reg Issues, 2018; 15:161–8. CrossRef
Theofilou P. Medication adherence in Greek hemodialysis patients: the contribution of depression and health cognitions. Int J Behav Med, 2013; 20(2):311–8. CrossRef
Wei L, Champman S, Li X, Li X, Li S, Chen R, Bo N, Chater A, Horne R. Beliefs about medicines and non-adherence in patients with stroke, diabetes mellitus and rheumatoid arthritis: a cross-sectional study in China. BMJ Open, 2017; 7(10):e017293. CrossRef
Wileman V, Farrington K, Wellsted D, Almond M, Davenport A, Chilcot J. Medication beliefs are associated with phosphate binder non-adherence in hyperphosphatemic haemodialysis patients. Br J Health Psychol, 2015; 20(3):563–78. CrossRef