INTRODUCTION
As per the population census report of 2011, nearly 104 million aged people resided in India, of which 53 million and 51 million are female and male, respectively. The United Nations Population Fund and HelpAge India report that these numbers are expected to grow to 173 million by 2026, and more than two-thirds of the Indian aged population are residing in rural areas (senior citizens’ status in India). Compared to adults, older people are at an enhanced risk of mortality and morbidity due to chronic diseases. Pharmacokinetic and pharmacodynamic changes in the aged make them more prone to hospitalization. As per the National Council of Applied Economic Research 2016 report, the prevalence of hypertension in the Indian ageing population has significantly increased from 6.6% (2004–2005) to 11.5% (2011-2012) (Adiseshiah M. Ageing in India: the health issues, 2018).
“Hypertension is defined as persistent elevation of arterial blood pressure (BP), and uncontrolled hypertension is a clinical condition where BP ≥140/90 mmHg, which carries a high morbidity and mortality risk, including heart failure, coronary heart disease, stroke, and renal insufficiency” (Chobanian et al., 2003; WHO, Hypertension, America, 2019).
Adherence is defined by the WHO as “the extent to which a person’s medication-taking behavior, following a diet, and/or executing lifestyle changes corresponds with agreed recommendations from a health care provider” (WHO, Adherence to long-term therapies: evidence for action, chronic diseases and health promotion, Switzerland, 2003). In general, the medication adherence of a patient can vary from 0% to 100%, and larger values represent better medication adherence by the patient. “Several factors are known to affect adherence: low socioeconomic status (SES), class of drug prescribed, number of pills per day, side effects of medication, patient’s inadequate understanding of the disease, age, gender, severity of disease and importance of the treatment” (Hashmi et al., 2007).
“Satisfaction is the perception of an individual’s experience compared with his or her expectations. For patients, it is related to the extent to which general healthcare needs and condition-specific needs are met” (Guldvog, 1999). “Patients’ satisfaction with their doctors is a key element in the efficiency and usage of health services and varies depending on patient characteristics. Each patient has expectations when meeting a doctor, and the difference between these expectations and what he obtains represents the perception of satisfaction” (Kuteyi et al., 2010). “Adherence to treatment, provision of continuous care, clinical management of the illness, and patients’ adjustment are very closely related to satisfaction with physician-patient interaction” (Loblaw et al., 1999).
According to previous research, hypertensive patients are considered adherent if they take at least 80% of their medications (Nair et al., 2011). Many studies have shown that, despite the availability of effective medications, controlling high BP in the ageing population is a major challenge for doctors. Nonadherence to antihypertensive medications is a major risk factor that can lead to uncontrolled BP, disease progression, increased healthcare costs, and even death (Cárdenas-Valladolid et al., 2010; Pasina et al., 2014; Wang et al., 2002). Nonadherence can also be influenced by dexterity issues, declining cognitive abilities, and poor healthcare provider–patient communication. As a result, the ageing population is more likely to experience medication mismanagement, adverse drug events, and poor health outcomes (Al-Ruthia et al., 2017). With this background, our study aimed at assessing medication adherence along with treatment satisfaction in aged hypertensive patients visiting a secondary care public hospital. Furthermore, our study also evaluated the relationship between treatment satisfaction and medication adherence in aged hypertensive patients.
MATERIALS AND METHODS
Study design and setting
A prospective observational convenient sample study was conducted between June 2017 and April/May 2018 at the Govt. District Headquarters Hospital, Ooty, which is a 480-bed secondary care public hospital catering to the healthcare needs of the general public in and around The Nilgiris district.
Inclusion and exclusion criteria
The study included hypertensive patients of either sex aged >60 years old visiting the outpatient department and hospital pharmacy. The study excluded noncooperative patients and hypertensive patients treated as inpatients.
Ethical clearance
The study was approved by the Institution Review Board, JSS College of Pharmacy, Ooty, Tamil Nadu (IRB approval number JSSCP/DPP/IRB/11/2017-18 Dated: 03-02-2018).
Study procedure
Hypertensive patients visiting the hospital pharmacy and outpatient department of the study site were reviewed on a daily basis. Patients meeting the study criteria were explained briefly about the research study. Those patients willing to participate in the study gave informed consent to participate, and then the data were collected through interviews. The data related to demographic characteristics, antihypertensive medication treatment, and prescription filling details were first collected. Furthermore, the patients were subjected to the Morisky Medication Adherence Scale (MMAS) and the Medication Interview Satisfaction Scale (MISS-21) to assess their medication adherence and treatment satisfaction, respectively. Wherever required, assistance was given by a graduate pharmacist to complete the information on the data collection form.
Study instruments
Data collection form
The data collection form included sections like demographic data, BP, social habits, diagnosis, family history, past medical history, past medication history, current therapy, etc.
Kuppuswamy’s SES scale
“The modified Kuppuswamy scale was used to measure the SES of patients. The scale is based on a composite score considering the education and occupation of the head of the family along with their monthly income, which yields a score of 3–29. The scale classifies the study populations into high, middle, and low SES ” (Singh et al., 2017).
The Morisky Medication Adherence Scale (MMAS)
“The MMAS was used to measure a participant’s adherence to medication. The MMAS is a validated self-reporting questionnaire consisting of eight questions. The questions address the patient’s medication-taking behavior but not medication adherence determinants; it requires a dichotomous response (yes/no) to 7 out of 8 questions, with a 5-point Likert scale for the last question. The total score ranges from 0 to 8, with scores of <6, 6 to <8, and 8 reflecting low, medium, and high adherence, respectively” (Morisky et al., 2008).
Medication Interview Satisfaction Scale (MISS-21)
“Patients’ treatment satisfaction was assessed with the aid of MISS-21, which was first developed for British general practice. The scale consists of 21 questions. The patient is asked to indicate their level of agreement on a 7-point Likert scale: very strongly disagree (1), strongly disagree (2), disagree (3), uncertain (4), agree (5), strongly agree (6), and very strongly agree (7). The scale is structured in four dimensions, namely ‘Distress relief subscale’ (6 items), ‘Communication comfort subscale’ (4 items), ‘Rapport subscale’ (8 items), and ‘Compliance intent subscale’ (3 items). Responses from all the questions are combined. Higher scores represent a higher level of satisfaction” (Meakin and Weinman, 2002).
Statistical analysis
Data were recorded on a predesigned proforma and managed on MS Excel. The entries were double checked for any possible keyboard errors. Data was analyzed using the Statistical Package for the Social Sciences version 20.0 (Systat Software, Chicago, II., USA). Bivariate analysis [Pearson’s Chi-square, odds ratio (OR), and 95% confidence interval (CI)] was executed to identify the predictors for nonadherence. Pearson’s correlation was executed to study the correlation between Morisky medication adherence scores along with SES and the number of medications received. “p”-value < 0.05 was considered statistically significant.
RESULTS
A total of 202 aged patients meeting the study criteria were recruited for the study. Of these, the majority were female (n = 102). The demographic characteristics of the study population are presented in Table 1. Age range of the study population was found to be 60–77 years. However, 60–65 years age group comprised majority (n = 120) of the study population. Majority of the patients were within the range of 130–140 mmHg systolic BP (n = 90) and 91–100 mmHg diastolic BP (n = 97). Only, 13.86% of the study population was found to have smoking habit and 15.84% of the study population was found to be alcoholic. About two-thirds of the study population had a normal body mass index (n = 157). Most of the patients in the present study were married and found to follow mixed/nonvegetarian diet. As per the modified Kuppuswamy scale 2017, most of the patients belonged to “lower class” and “upper lower class” with regard to the SES.
Detailed information about the various drugs prescribed in the study population is presented in Table 2. The most Commonly prescribed drugs for comorbid conditions in the study population was found to be calcium channel blockers, followed by angiotensin-converting enzyme inhibitors and beta blockers. The most prescribed antihypertensive medication was found to be Amlodipine and about 69 patients were treated with two or more antihypertensive drugs. Along with antihypertensives, proton pump inhibitors, multivitamins, calcium supplements, and Atorvastatin were the most commonly prescribed medicines for comorbid conditions in the study population.
The level of medication adherence was assessed using the MMAS. As per the scores, 38.61% (n = 78) of the patients were found to have high adherence to their medications. 19.3% (n = 39) and 42.07% (n = 85) of the patients were found to have medium adherence and low adherence, respectively. For the purpose of executing statistical analysis, patients apart from the high adherence group were combined together, and this was taken up for the calculation of the prevalence of nonadherence and further bivariate analysis. Elevated BP, polypharmacy, and nonvegetarian/mixed diet were the influential predictors for nonadherence as identified by bivariate analysis (p < 0.05). Other variables did not have statistical significance. The prevalence of nonadherence and its bivariate analysis results are presented in Table 3. Treatment satisfaction was assessed using MISS-21. As per the scores, majority of the patients were found to be highly satisfied with their treatment. All the domains showed similar patterns of satisfaction. The descriptive statistics of the MISS-21 are given in Table 4. MMAS scores and number of drugs prescribed were subjected to Pearson’s correlation; a weak positive correlation was noted [Correlation coefficient, (r)-0.392, coefficient of determination, (R2)-0.153]. Morisky scale scores and SES were subjected to Pearson’s correlation; a weak positive correlation was noted [Correlation coefficient, (r)-0.046, coefficient of determination, (R2)-0.002]
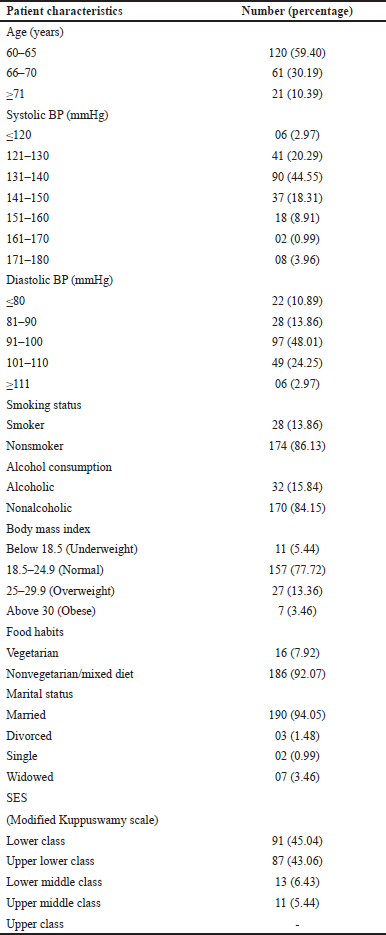 | Table 1. Demographic characteristics of the study population. [Click here to view] |
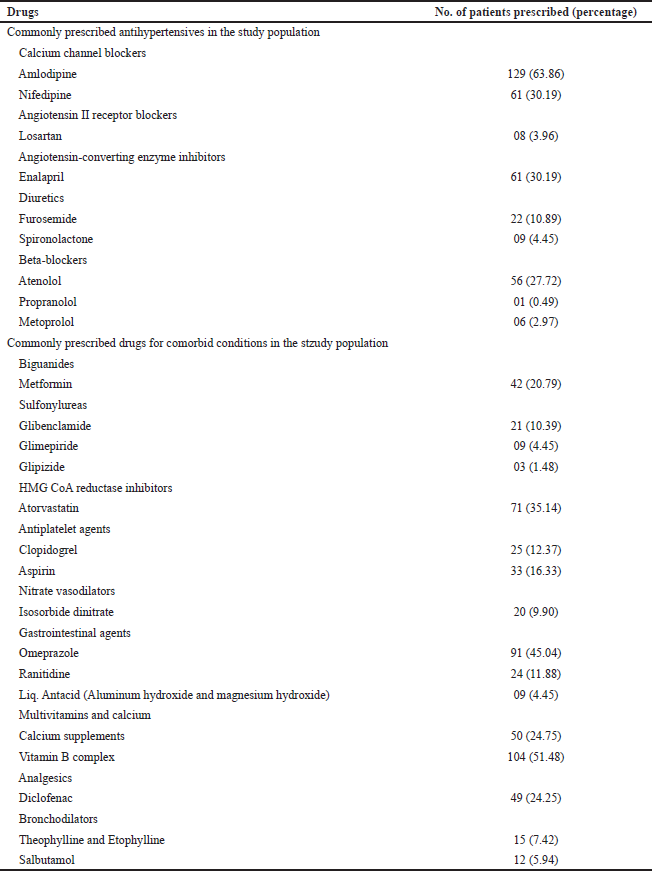 | Table 2. Commonly prescribed drugs in the study population. [Click here to view] |
DISCUSSION
Population ageing is taking place throughout the world, and hypertension is a common disease. One major reason for this trend is the patterns of changes in BP and increasing hypertension prevalence with age (in about 1 billion people worldwide) (Kearney et al., 2005). A total of 202 aged patients participated in the present study, and the number of male and female patients was almost equal. Many studies on the aged population published in developed countries are conducted by recruiting patients aged ≥65 years. Our study recruited patients aged ≥60years. This is justified because the normal age for retirement and the margin for senior citizenship in India is 60 years (Maintenance and Welfare of Parents & Senior Citizens Act, 2007). In addition, research studies from India have already been published with an age cut-off of 60 years and above (Harugeri et al., 2010; Vishwas et al., 2012).
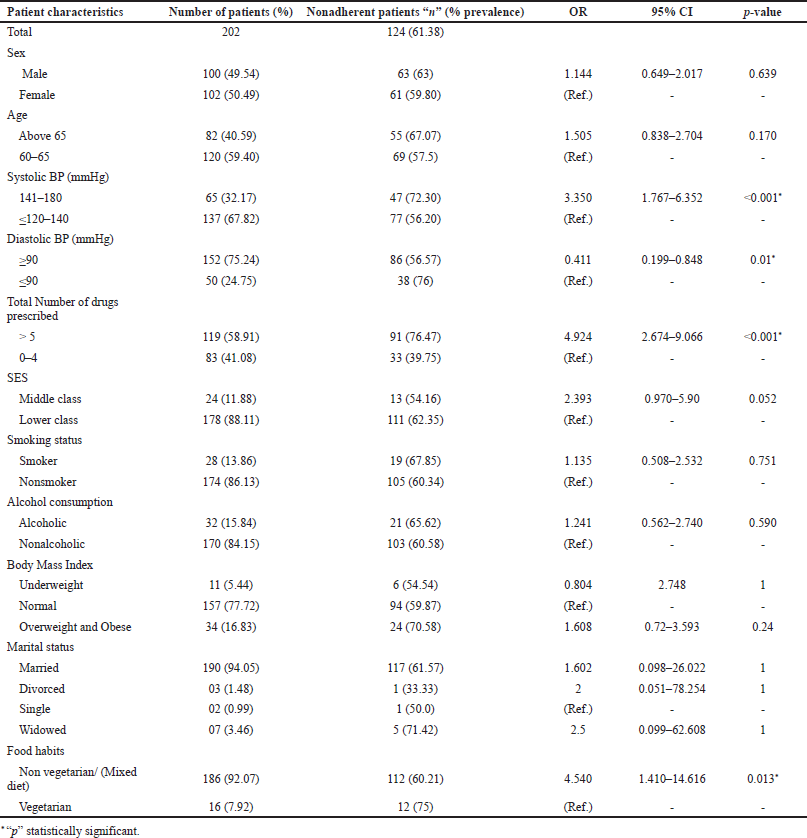 | Table 3. Prevalence and predictors for nonadherence in the study population using bivariate analysis. [Click here to view] |
In this study, majority of the patients were prescribed with calcium channel blockers (Amlodipine, dose range of 2.5–10 mg; Nifedipine, dose range of 10–30 mg), Enalapril (dose range of 2.5–40 mg), and Atenolol (dose range of 5–50 mg). This practice is justified because, as per the eigth Joint National Committee recommendations, nonblack adults should be initiated with either any one of the following drugs as their first choice of treatment [thiazide diuretic, calcium channel blocker-CCBs, angiotensin-converting enzyme inhibitors (ACEIs) or angiotensin receptor blockers (ARBs)] (James et al., 2014). These agents are preferred because evidence from outcome data has demonstrated cardiovascular risk reduction benefits with these classes. Patients with comorbidities like diabetes mellitus should be prescribed ACEIs or ARBs. However, our hospital was adhering to the recommendations of the guidelines.
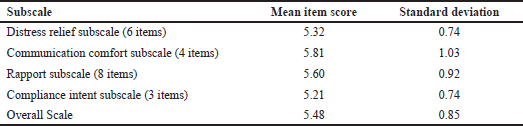 | Table 4. Descriptive statistics of MISS-21. [Click here to view] |
A total of 124 patients out of 202 patients had low-to-moderate adherence problems as per the MMAS (Morisky et al., 2008). Hence, these patients were considered nonadherent, and the prevalence of nonadherence in the present study was found to be 61.38%. In a community-based study from South India, the prevalence of nonadherence was found to be 45.4% (Venkatesan et al., 2018). In a cross-sectional study on aged patients from Korea, the prevalence of low adherence was found to be 52.5% (Jin et al., 2016). Our study was conducted at a public hospital, where the health literacy of the patients visiting the hospital is expected to be lower when compared to patients visiting a private hospital. In Ooty, the majority of the patients are from agricultural and rural backgrounds. Hence, the level of health awareness is relatively lower when compared to patients visiting a private hospital. This could be the reason for us to observe the high prevalence of nonadherence in our study population.
Upon applying the bivariate analysis, elevated BP, nonvegetarian or mixed diet, and polypharmacy were identified as influential predictors for nonadherence (p < 0.05). Poor medication adherence is a major issue for hypertension treatment. Even though it is considered one of the major causes of treatment failure, our study also assessed the relationship between patient medication adherence and treatment satisfaction in patients who are taking antihypertensive medications. Studies have shown that the reasons for medication nonadherence are knowledge and beliefs about medication, polypharmacy, adverse drug reactions, age, and sociodemographic factors (Yap et al., 2016; Yokoyama et al., 2014). Researchers from Japan and the United States of America in their meta-analysis showed that removing meat from the diet can result in a significant reduction in systolic and diastolic BP. The study also concluded that vegetarian food can be considered a nonpharmacological treatment for hypertension (Alsabbagh et al., 2014). Interventions targeting the limiting of nonvegetarian food and salt restriction should be focused on educating hypertensive patients to avoid unnecessary complications like hypertensive emergencies. Polypharmacy has been frequently considered as one major medication-related issue among older adults with comorbidities. This finding also correlates with the study by Pasina et al. (2014). The number of patients who were taking fewer drugs was more adherent in comparison with those taking ≥5 drugs. We also observed a weak positive correlation between MMAS scores and the number of drugs prescribed. As the MMAS scores increase, the nonadherence pattern also increases. This finding also supports the notion that polypharmacy can act as a factor to precipitate nonadherence behavior in the aged population.
We also observed a weak positive correlation between the patients’ SES and MMAS scores. This finding suggests that the lower SES patients were found to have more adherence behavior to their medications when compared to the middle-class population. This may be an incidental finding, because a meta-analysis conducted in Canada reported that there is no association between low SES and nonadherence to antihypertensive medications (Wolf et al., 1978).
We used the MISS-21 instrument even though it was developed for use in British general practice, due to the absence of a standard indigenous instrument to assess the level of satisfaction in patients with chronic diseases. Another reason for choosing MISS-21 is that it is derived from the original 29-item MISS developed by Wolf et al., (1978) which is one of the most cited research instruments in assessing patient satisfaction toward healthcare (Wolf et al., 1978). MISS-21 has demonstrated good validity and internal consistency (reported values of Cronbach’s alpha between 0.67 and 0.92) (Meakin and Weinman, 2002).
By conducting a personal interview with the aged patients during data collection, we observed that a lot of patients had good trust in the physicians of the hospital. This is the reason we observed good levels of treatment satisfaction in our study population. Good scores were noted in all the four domains of MISS, suggesting good levels of patient satisfaction, namely distress relief, communication comfort, compliance intent, and rapport. Studies have reported that emotional support and a sense of trust in the doctors noticeably affect the patient’s satisfaction, leading to better treatment outcomes (Guldvog, 1999; Kinnersley et al., 1996).
The results of the present study have to be carefully interpreted and a few points have to be considered limitations because the study was conducted at a public hospital and not a private hospital. Here, the patients were not charged for the medical consultations. They were also issued medications free of charge. In our study, we observed patients from lower and middle SES levels, and no patients from upper socioeconomic levels were observed in our study.
The findings of the present study were completely based on patients’ responses to the interviewer. We did not confirm the adherence pattern of the patients by performing other alternative methods like the pill count method, serum level drug estimations, etc. Future studies should incorporate both subjective and objective confirmation of the adherence behavior of the patients. Large multicentric studies will be very helpful in assessing the exact prevalence of nonadherence in aged hypertensive patients.
CONCLUSION
Multiple factors, such as a patient’s mental status, health literacy, comorbidities, and drug-related problems, influence the medication adherence behavior of aged patients. In our study, it was observed that elevated BP, polypharmacy, and nonvegetarian diet affected the medication adherence of our study population. In spite of reporting good satisfaction levels, majority of the patients still remained nonadherent to their medications. As a special population, aged patients need to be specially addressed in hospitals regarding the advantages of treatment adherence. Aged hypertensive patients should be counseled that they need to take the drugs lifelong. There is an increased responsibility on all healthcare professionals especially when dealing aged patients with chronic diseases. Considering the fact that majority of the aged people reside in rural areas, the primary healthcare system in rural India needs to be strengthened to achieve better health outcomes.
ACKNOWLEDGMENT
The authors express their gratitude to JSS College of Pharmacy, Ooty, and JSS Academy of Higher Education and Research, Mysuru, for providing various facilities used during the project. The authors also thank the staff and healthcare professionals of the Govt. District Headquarters Hospital, Ooty, for supporting the project.
CONFLICTS OF INTEREST
The authors report no financial or any other conflicts of interest in this work.
ETHICAL APPROVALS
The study was approved by the Institution Review Board, JSS College of Pharmacy, Ooty, Tamil Nadu (IRB approval number JSSCP/DPP/IRB/11/2017-18 Dated: 03-02-2018).
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
FUNDING
The authors declare that they have no funding support for this study.
AUTHORS’ CONTRIBUTIONS
All authors contributed to the study and conception of design. Dr. Ponnusankar S and Dr. Balasubramaniam V reviewed and commented on the first and subsequent drafts of the manuscript. They were also involved in data analysis/interpretation and supervision. Mr. Vishwas HN, Ms. Anjali K, and Mr. Manoj Kumar S contributed to data acquisition, data analysis/interpretation, and statistical analysis.
REFERENCES
Adiseshiah M. Ageing in India: the health issues, 2018 Available via https://www.ncaer.org/uploads/photo-gallery/files/1478675655NCAER-Health.pdf
Al-Ruthia YS, Hong SH, Graff C, Kocak M, Solomon D, Nolly R. Examining the relationship between antihypertensive medication satisfaction and adherence in older patients. Res Social Adm Pharm, 2017; 13(3):602–13. CrossRef
Alsabbagh MW, Lemstra M, Eurich D, Lix LM, Wilson TW, Watson E, Blackburn DF. Socioeconomic status and nonadherence to antihypertensive drugs: a systematic review and meta-analysis. Value Health, 2014; 17(2):288–96. CrossRef
Cárdenas-Valladolid J, Martín-Madrazo C, Salinero-Fort MA, de-Santa Pau EC, Abánades-Herranz JC, de Burgos-Lunar C. Prevalence of adherence to treatment in homebound elderly people in primary health care. Drugs Aging, 2010; 27(8):641–51. CrossRef
Chobanian AV, Bakris GL, Black HR, Cushman WC, Green LA, Izzo Jr JL, et al. The seventh report of the joint national committee on prevention, detection, evaluation, and treatment of high blood pressure: the JNC 7 report. JAMA, 2003; 289(19):2560-71 CrossRef
Guldvog BJ. Can patient satisfaction improve health among patients with angina pectoris? Int J Qual Health Care, 1999; 11(3):233–40. CrossRef
Harugeri A, Joseph J, Parthasarathi G, Ramesh M, Guido S. Potentially inappropriate medication use in elderly patients: a study of prevalence and predictors in two teaching hospitals. J Postgrad Med, 2010; 56(3):186–91. CrossRef
Hashmi SK, Afridi MB, Abbas K, Sajwani RA, Saleheen D, Frossard PM, Ishaq M, Ambreen A, Ahmad U. Factors associated with adherence to anti-hypertensive treatment in Pakistan. PLoS One, 2007; 2(3):280. CrossRef
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC. Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the Eighth Joint National Committee (JNC 8). JAMA, 2014; 311(5):507–20. CrossRef
Jin H, Kim Y, Rhie SJ. Factors affecting medication adherence in elderly people. Patient Prefer Adher, 2016; 10:2117. CrossRef
Kearney PM, Whelton M, Reynolds K, Muntner P, Whelton PK, He J. Global burden of hypertension: analysis of worldwide data. Lancet, 2005; 365(9455):217–23. CrossRef
Kinnersley P, Stott N, Peters T, Harvey I, Hackett P. A comparison of methods for measuring patient satisfaction with consultations in primary care. Fam Pract, 1996; 13(1):41–51. CrossRef
Kuteyi EA, Bello IS, Olaleye TM, Ayeni IO, Amedi MI. Determinants of patient satisfaction with physician interaction: a cross-sectional survey at the Obafemi Awolowo University Health Centre, Ile-Ife. Nigeria. S Afr Fam Pract, 2010; 52(6):557–62. CrossRef
Loblaw DA, Bezjak A, Bunston T. Development and testing of a visit-specific patient satisfaction questionnaire: the Princess Margaret hospital satisfaction with doctor questionnaire. J Clin Oncol. 1999; 17(6):1931–8. CrossRef
Maintenance and Welfare of Parents and Senior Citizens Act. Ministry of Social Justice and Empowerment. Government of India, 2007 Available via https://socialjustice.nic.in/writereaddata/UploadFile/Annexure-X635996104030434742.pdf
Meakin R, Weinman J. The Medical Interview Satisfaction Scale (MISS-21) adapted for British General Practice. Fam Pract, 2002; 19(3):257–63. CrossRef
Morisky DE, Ang A, Krousel-Wood M, Ward HJ. Predictive validity of a medication adherence measure in an outpatient setting. J Clin Hypertens (Greenwich), 2008; 10(5):48–54. CrossRef
Nair KV, Belletti DA, Doyle JJ, Allen RR, McQueen RB, Saseen JJ, Vande Griend J, Patel JV, McQueen A, Jan S. Understanding barriers to medication adherence in the hypertensive population by evaluating responses to a telephone survey, patient preference and adherence. Patient Prefer Adherence, 2011; 5: 195–206. CrossRef
Pasina L, Brucato AL, Falcone C, Cucchi E, Bresciani A, Sottocorno M, Taddei GC, Casati M, Franchi C, Djade CD, Nobili A. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging, 2014; 31(4):283–9. CrossRef
Senior Citizens - status in India, 2018. Available via https://vikaspedia.in/social-welfare/senior-citizens-welfare/senior-citizens-status-in-india
Singh T, Sharma S. and Nagesh S. Socio-economic status scales updated for 2017. Int J Res Med Sci, 2017; 5(7):3264–7. CrossRef
Venkatesan M, Dongre AR, Ganapathy K. A community-based study on diabetes medication non-adherence and its risk factors in rural Tamil Nadu. Indian J Community Med, 2018; 43(2):72–6.
Vishwas HN, Harugeri A, Parthasarathi G, Ramesh M. Potentially inappropriate medication use in Indian elderly: comparison of beers’ criteria and screening tool of older persons’ potentially inappropriate prescriptions. Geriatr Gerontol Int, 2012; 12(3):506–14. CrossRef
Wang PS, Bohn RL, Knight E, Glynn RJ, Mogun H, Avorn J. Noncompliance with antihypertensive medications: the impact of depressive symptoms and psychosocial factors. J Gen Intern Med, 2002; 17(7):504–11. CrossRef
WHO. Adherence to long-term therapies: evidence for action, chronic diseases and health promotion. WHO, Geneva, Switzerland, 2003.
WHO. Hypertension, America. WHO, Geneva, Switzerland, 2019.
Wolf MH, Putnam SM, James SA, Stiles WB. The medical interview satisfaction scale: development of a scale to measure patient perceptions of physician behaviour. J Behav Med, 1978; 1(4):391–401. CrossRef
Yap AF, Thirumoorthy T, Kwan YH. Medication adherence in the elderly. J Clin Gerontol Geriatr, 2016; 7(2):64–7. CrossRef
Yokoyama Y, Nishimura K, Barnard ND, Takegami M, Watanabe M, Sekikawa A, Okamura T, Miyamoto Y. Vegetarian diets and blood pressure: a meta-analysis. JAMA Intern Med, 2014; 174(4):577–87. CrossRef