INTRODUCTION
About 4.4% of the global population suffered from depressive disorder, whereas 3.6% suffered from anxiety in 2015. Significant variation is found in the global rate of depression from 3.6% in the Western Pacific Region to 5.4% in Africa (WHO, 2017). The incidence rate of depression has increased by 49.86% from 1990 to 2017 worldwide, despite the reported decrease in 18 countries. The highest prevalence rate of mental disorders is found in Finland, the Netherlands, France, and Ireland, whereas the lowest is in Romania, Bulgaria, and Poland (OECD/EU, 2018). The highest decline is established in Latvia (−30.99%), followed by Bosnia and Herzegovina (−25.75%) and Georgia (−23.98%) (Liu et al., 2020).
The overall costs due to mental disorders rose significantly across the 28 EU countries. The estimated expenditures range from 2% to 2.5% of gross domestic product in Romania, Bulgaria, and the Czech Republic to over 5% in Finland, Denmark, the Netherlands, and Belgium (OECD/EU, 2018).
The COVID-19 pandemic caused a sharp increase in the prevalence of anxiety and depression among the general adult population in China. The financial burden is one of the main factors related to both anxiety and depression (Li et al., 2020). A positive correlation is found between the impact of the COVID pandemic on economic results and effects on daily life, whereas this correlation is negative if there is social support (Cao et al., 2020). A systematic review and meta-analysis reported 15.97% prevalence of depression, 15.15% prevalence of anxiety, and 23.87% prevalence of insomnia related to COVID-19 among the affected populations (Cénat et al., 2020). In addition, deterioration in mental health since the pandemic is established (Choi et al., 2020). Observing posttraumatic stress disorder prevalence also reveals its higher psychological impact on patients infected with COVID-19 (Alshehri et al., 2020).
Defining the right outcomes and main patients’ needs when they seek treatment could help in the quick diagnosis and treatment of disease (Cuijpers, 2020). Factors such as medication side effects, patient’s gender, occupation, and education resulted in a low level of patient adherence (Marasine et al., 2020). A potential role of the pharmacist in depression treatment and adequately oriented pharmaceutical care could help in achieving good clinical results and disease control (Kamusheva et al., 2020), especially in such crisis situations as COVID -19 (Assiri et al., 2021).
There are doubts that the COVID-19 pandemic expansion in Bulgaria significantly influences population status and disease diagnostics, control, and treatment. Social and physical isolation leads to low activity, worsening patient condition, anxiety, and depressive disorder.
Depression is a chronic disease that requires strong control and treatment management. The achieved clinical results depend at a high rate on patients’ status and social environment. The goal of our study is to measure utilization of antidepressants in the outpatient treatment of depression and public spending on their reimbursement to establish if there are significant differences before and after pandemic expansion and establishment of the initial impact on depression treatment in Bulgaria.
MATERIALS AND METHODS
Design of the study
We performed a cross-sectional, retrospective, observational, macroeconomic analysis of National Health Insurance Fund (NHIF) expenditures on antidepressants included in the Positive Drug List (PDL) with Anatomical Therapeutic Chemical (ATC) codes N06AB and N06AX. In total, 10 international nonproprietary names (INNs) used for outpatient depression treatment were included in the analysis.
The utilization of antidepressants was retrospectively calculated and analyzed. The study covered only the medicines reimbursed by the NHIF in Bulgaria during the periods January–September 2019 and January–September 2020, which are nine months before and after the beginning of the COVID-19 pandemic.
The reimbursed costs were compared before and after the beginning of the COVID-19 pandemic for the periods January–September 2019 and January–September 2020.
All costs are presented in euro, based on the official exchange rate: 1 BGN = 0.51 euros.
Data sources
Data for the reimbursed expenditures, medicine utilization, and the number of reimbursed packages of all INNs was collected from the NHIF official register (NHIF, 2019, 2020). The number of inhabitants was selected from the National Statistical Institute (NSI) database (NSI, 2019, 2020). The total population was 6,951,482 people in 2019 and 6,924,882 people in 2020.
The reference price per DDD (the lowest reimbursed price) was extracted from Annex 1 of the PDL “Medicinal Products for Outpatient Treatment” published in the official register of the National Council on Prices and Reimbursement of Medicinal Products (NCPRMP, 2019, 2020).
Cost analysis
The total reimbursed expenditures, as well as reference price per DDD, were retrospectively gathered, summed via Excel 2010, and compared in absolute terms to evaluate their changes. The cost paid by the NHIF before (January–September 2019) and after (January–September 2020) the COVID pandemic in Bulgaria was calculated for each INN.
The changes in overall reimbursed cost per year were tested with the Mann–Whitney test. p values lower than 0.05 are considered statistically significant.
Medicine utilization analysis
Medicine utilization per INN was evaluated by the WHO formula for DDD/1,000 inhabitants/day (WHO Collaborating Centre for Drug Statistics Methodology Guidelines, 2017):
The changes in utilization were tested with the Mann–Whitney test. p values less than 0.05 are determined as statistically significant. Descriptive statistics are used to express the main variables measuring utilization in 2019 and 2020.
RESULTS
Cost analysis
The reference price per DDD remains almost the same during the observed period. Two of the compared INNs are found with decreasing values (agomelatine and trazodone) and two with increasing ones (mirtazapine and duloxetine) (Table 1).
The results reveal that costs paid by the NHIF in 2020 decreased or remained almost the same as those found in 2019. Only mirtazapine and vortioxetine are exceptions, where an increasing cost was found (Fig. 1).
The prepared test compares the reimbursed amount in 2019 and that in 2020 for all INNs included in the analysis. The final result reveals no statistically significant difference (p = 0.67).
Medicine utilization analysis
Medicine utilization measured in DDD/1,000 inhabitants/day is similar before and after the beginning of the COVID-19 pandemic (Fig. 2).
Overall antidepressant utilization decreased in 2020 compared to that in 2019 with 3.455 DDD /1,000 inhabitants/day. A slightly increasing consumption is found in six INNs, whereas decreasing is established in four. The highest utilization rate is found for escitalopram (both 2019 and 2020), followed by paroxetine and venlafaxine (Fig. 2).
To confirm a low rate of deviations found in medicine utilization, we have prepared descriptive statistics analysis via Excel 10. The established sample variance and low standard deviation value illustrate similarity in results and confirm that high differences in medicine consumption in 2019 and 2020 did not exist (Table 2).
The Mann–Whitney test reveals no statistically significant changes between overall utilization data in 2019 compared to that in 2020 (p = 0.968). Therefore, outpatient medicine utilization is almost the same in the research period with a very slight decreasing level in 2020.
The analysis of the results for the consumption and costs shows that the increasing level of utilization often leads to growing costs of the payment institution for outpatient treatment. In general, these changes are not significant after the beginning of the pandemic (Table 3).
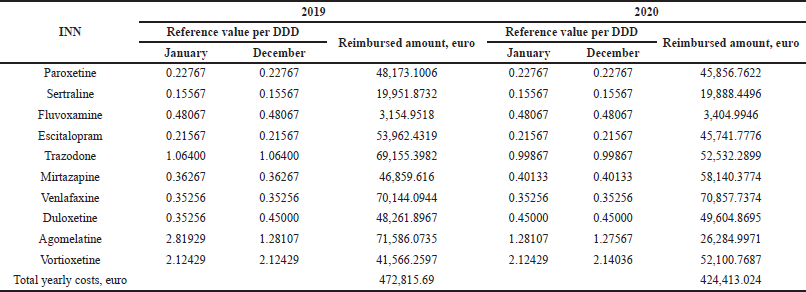 | Table 1. Reference value per DDD and reimbursed expenditure in 2019 and 2020. [Click here to view] |
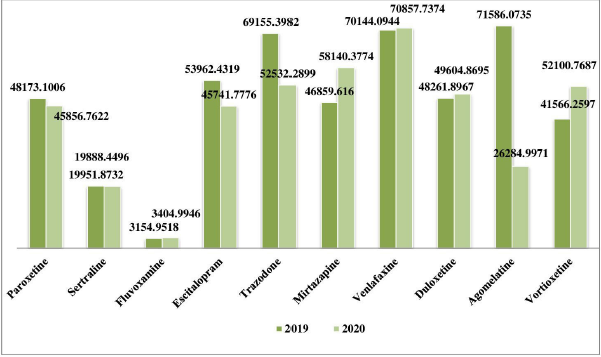 | Figure 1. Reimbursed value paid by NHIF for antidepressants. [Click here to view] |
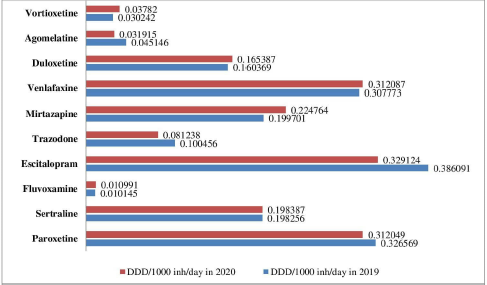 | Figure 2. Antidepressant utilization measured in DDD/1,000 inh/day in 2019 and 2020 [Click here to view] |
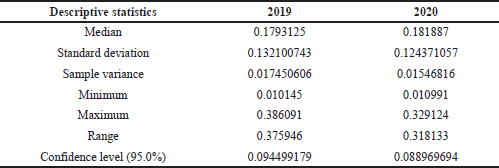 | Table 2. Descriptive statistics based on utilization data. [Click here to view] |
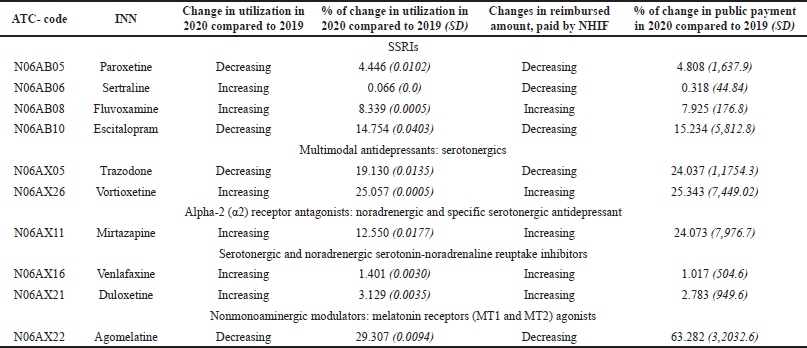 | Table 3. Changes in antidepressant utilization in ambulatory practice and reimbursed amount paid by the NHIF during the observed period. [Click here to view] |
DISCUSSION
Expansion of the COVID-19 pandemic imposed full quarantine and social and physical isolation of the population worldwide. The COVID-19 pandemic set new challenges in psychiatric practice and treatment of mentally ill patients with COVID-19 due to their vulnerability and sensitivity (Andrade et al., 2020).
A study in Saudi Arabia reported that a smaller proportion of individuals had symptoms like anxiety or depression, while a majority declared psychological distress during the COVID-19 pandemic (Joseph et al., 2021). Depression and anxiety are prevailing among healthcare providers despite the efforts supporting their psychological conditions (AlAteeq et al., 2020).
The symptomatic treatments of COVID-19 lead to frequent interactions between the most often used psychotropics (Javelot et al., 2020). More and more patients need additional antidepressants or psychotropics due to isolation or loneliness, which may affect further mental illness progression (Uvais, 2020).
During lockdown in Croatia, a questionnaire among 3,027 respondents reported that, in this period, both men and women felt more frequently afraid, discouraged, and sad. A cross-sectional study in Italy reported that 24.7% of patients felt depression, while 23.2% reported anxiety and 42.2% had sleep disturbances and among them 17.4% reported moderate/severe insomnia. Increasing age, an absence of work-related problems, and family reduced such a probability (Gualano et al., 2020).
The study uses the Yale-Brown Obsessive Compulsive Severity score before assessing the quarantine influence after 6 weeks since the beginning of the complete lockdown. It found a significant increase in obsession and compulsion severity and more elevated obsessive-compulsive disorder (OCD) symptom worsening during the quarantine (Davide et al., 2020). These results suggest that health authorities should promote healthy lifestyles to reduce the long-term negative effects of the quarantine (?ogaš et al., 2020).
In Bulgaria, full quarantine and isolation were implemented on March 13, 2020 (Order, 2020). Social isolation and loneliness have been found to predict premature mortality, depression, cardiovascular disease, and cognitive decline, and this had dramatic mental health impacts, bringing about increased anxiety and greater social isolation (Smith et al., 2020). As a result, a high number of patients were afraid to perform regular physician visits to avoid COVID-19 contaminations. The lack of electronic prescriptions finally could affect medicine utilization, especially medicines paid for by the NHIF. To avoid this confusion, the Minister of Health issued an order to allow pharmacists to dispense medicines without new prescriptions with only available patient prescription books as confirmation of appointed therapy.
The trend of antidepressant consumption in Italy between 2000 and 2011 reveals significant increase in selective serotonin reuptake inhibitors (SSRIs) and other antidepressant utilization and a decrease in that of tricyclic antidepressants (Gualano et al., 2014). In England, it was found that SSRIs were the most prescribed class, followed by citalopram, fluoxetine, and mirtazapine (Heald et al., 2020). A study that measured medicine utilization in Iran (in DDD/1,000 in hour/day as sales and prescription) reveals the highest SSRI consumption rate (Soleymani et al., 2018), as we found in Bulgaria.
In line with the recommendations as to the first-line treatment for depressive disorders, as in Bulgaria, SSRIs are prescribed most frequently in other countries. Hence, it is not a result of pandemic expansion and the final results are based on clinical practice recommendations and treatment approaches applied before 2020 (Gautam et al., 2017).
The highest differences in utilization are found in agomelatine with a 29% decreasing rate and vortioxetine with growth of about 25%. These findings could not be discussed from the pandemic point of view. The rising value of vortioxetine consumption is probably due to data discussed in literature promising higher efficacy in the treatment of major depressive disorder and tolerability, without cardiovascular or weight gain effects (Orsolini et al., 2017).
Our study found that this measure works effectively and adequately in Bulgaria, as medicine utilization is similar with no statistically significant difference before and after the pandemic. The small decline in antidepressants consumption could be the result of some patients’ discomfort or worries about visiting physicians’ offices and the necessity of special prescriptions for narcotics. A study measuring resilience, mood, and mental health outcomes during the first wave of the COVID-19 pandemic in Bulgaria reveals lower anxiety and depression. A significant rise is measured in negative mood compared to that before the pandemic (Psederska et al., 2021). These facts suppose a stable medicine utilization level and a lack of extreme growth due to the stable rate of concerned patients. Therefore, found deviations in utilization of some antidepressant are not directly connected with the COVID-19 pandemic expansion in Bulgaria.
A study in India confirms that strict control of medicine price and utilization is needed during the pandemic and only costs of personal protective equipment and analgesics increase in this period (Haque et al., 2021).
The stable reimbursed expenditure paid by the NHIF for antidepressants in this period also confirms steadiness in the level of medicine utilization, number of patients, and morbidity and supposes a low rate of newly diagnosed patients after pandemic expansion in Bulgaria. The similarity in reference price per DDD used as a basis for establishing the reimbursed amount predicted a stable level of public payment for outpatient depression treatment and adequate price control during pandemic expansion. Only the reference price per DDD of agomelatine has declined significantly, thus leading to substantial lowering of reimbursed payment (63%) and declining in utilization by 29%.
A retrospective and observational study measured antidepressant utilization during an economic crisis with a 12-month period that patients followed. During the observed period, antidepressant consumption rose by 35.2%, while expenditure decreased by 38.7% (Peiró and Meneu, 2011). Further studies are needed to establish the rising trend of antidepressant utilization after pandemic expansion and the following economic crisis in Bulgaria.
The limitation of our study is the short research period due to the lack of availability of official published data concerning the reimbursed amount of medicinal products. Our study is not designed to define the association between different patient groups, medicine utilization, and disease prevalence. There is a lack of an official register in Bulgaria illustrating treatment and medicine utilization of patients suffering from COVID-19. As a result, comparison between the general population and patients with SARS-Cov-2 is not possible.
Our study found a similar rate of medicine utilization before the pandemic and when it started, but further studies are needed to confirm this claim and observe the trends on a long-term basis.
CONCLUSION
The COVID-19 pandemic and social isolation lead to worsening of mental health and require health system reorganization to ensure the treatment of patients with chronic diseases. The measures implemented in Bulgaria at the beginning of the pandemic led to a stable level of medicine utilization and outpatient treatment of depression as well as a similar rate of NHIF expenditure compared with the relevant period in the previous year.
AUTHORS’ CONTRIBUTIONS
All authors made substantial contributions to the conception and design of the work, acquisition, analysis, and interpretation of data for the work, and drafting of the manuscript and revising it critically and approved the final version of the manuscript.
FUNDING
There is no funding to report.
CONFLICTS OF INTEREST
The authors report no financial or any other conflicts of interest in this work.
ETHICAL APPROVALS
This study does not involve experiments on animals or human subjects.
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
AlAteeq DA, Aljhani S, Althiyabi I, Majzoub S. Mental health among healthcare providers during coronavirus disease (COVID-19) outbreak in Saudi Arabia. J Infect Public Health, 2020; 13(10):1432–7. CrossRef
Alshehri FS, Alatawi Y, Alghamdi BS, Alhifany AA, Alharbi A. Prevalence of post-traumatic stress disorder during the COVID-19 pandemic in Saudi Arabia. Saudi Pharm J, 2020; 28(12):1666–73. CrossRef
Andrade G, Simões do Couto F, Câmara-Pestana L. Recomendações sobrea Utilização de Fármacos Psicotrópicos durante a Pandemia COVID-19 [Recommendations about the use of psychotropic medications during the COVID-19 pandemic]. Acta Med Port, 2020; 33(10):693–702. CrossRef
Assiri A, Iqbal MJ, Gramish J, Assiri A, Meraya A, Alhossan A, Khobrani M. Pharmacists’ satisfaction with their involvement in the management of COVID-19 patients in Saudi Arabia. Saudi Pharm J, 2021; 29:85–90. CrossRef
Cao W, Fang Z, Hou G, Han M, Xu X, Dong J, Zheng J. The psychological impact of the COVID-19 epidemic on college students in China. Psychiatry Res, 2020. [ONLINE]. Available via https://pubmed.ncbi.nlm.nih.gov/32229390/ CrossRef
Cénat JM, Blais-Rochette C, Kokou-Kpolou CK, Noorishad PG, Mukunzi JN, McIntee SE, Dalexis RD, Goulet MA, Labelle PR. Prevalence of symptoms of depression, anxiety, insomnia, posttraumatic stress disorder, and psychological distress among populations affected by the COVID-19 pandemic: a systematic review and meta-analysis. Psychiatry Res, 2020. [ONLINE]. Available via https://pubmed.ncbi.nlm.nih.gov/33285346/ CrossRef
Choi EPH, Hui BPH, Wan EY. Depression and anxiety in Hong Kong during COVID-19. Int J Environ Res Public Health, 2020. [ONLINE]. Available via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7277420/ CrossRef
Cuijpers P. Measuring success in the treatment of depression: what is most important to patients? Expert Rev Neurother, 2020; 20(2):123–5. CrossRef
Davide P, Andrea P, Martina O, Andrea E, Davide D, Mario A. The impact of the COVID-19 pandemic on patients with OCD: effects of contamination symptoms and remission state before the quarantine in a preliminary naturalistic study. Psychiatry Res, 2020. [ONLINE]. Available via https://pubmed.ncbi.nlm.nih.gov/32535508/ CrossRef
?ogaš Z, Luši? Kalcina L, Pavlinac Dodig I, Demirovi? S, Madirazza K, Vali? M, Pecoti? R. The effect of COVID-19 lockdown on lifestyle and mood in Croatian general population: a cross-sectional study. Croatian Med J, 2020; 61(4):309–18. CrossRef
Gautam S, Jain A, Gautam M, Vahia VN, Grover S. Clinical practice guidelines for the management of depression. Indian J Psychiatry, 2017; 59(Suppl 1):S34–50; http://doi.org/10.4103/0019-5545.196973 CrossRef
Gualano MR, Bert F, Mannocci A, La Torre G, Zeppegno P, Siliquini R. Consumption of antidepressants in Italy: recent trends and their significance for public health. Psychiatr Serv, 2014; 65(10):1226–31 CrossRef
Gualano MR, Lo Moro G, Voglino G, Bert F, Siliquini R. Effects of Covid-19 lockdown on mental health and sleep disturbances in Italy. Int J Environ Res Public Health, 2020. [ONLINE]. Available via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7369943/ CrossRef
Haque M, Kumar S, Charan J, Bhatt R, Islam S, Dutta S, Abhayanand JP, Sharma Y, Sefah I, Kurdi A, Wale J, Godman B. Utilisation, Availability and price changes of medicines and protection equipment for COVID-19 among selected regions in India: findings and implications. Front Pharmacol, 2021. [ONLINE]. Available via https://www.frontiersin.org/articles/10.3389/fphar.2020.582154/full CrossRef
Heald AH, Stedman M, Davies M, Livingston M, Taylor D, Gadsby R. Antidepressant prescribing in England: patterns and costs. Prim Care Companion CNS Disord, 2020; 22(2):19m02552. CrossRef
Javelot H, Llorca PM, Drapier D, Fakra E, Hingray C, Meyer G, Dizet S, Egron A, Straczek C, Roser M, Masson M, Gaillard R, Fossati P, Haffen E. Informations relatives aux psychotropeset à leurs adaptations éventuelles pour les patients souffrant de troubles psychiquesen France pendant l’épidémie à SARS-CoV-2 [Informations on psychotropics and their adaptations for patients suffering from mental disorders in France during the SARS-CoV-2 epidemic]. Encephale, 2020; 46(3S):S14–34. CrossRef
Joseph R, Alshayban D, Lucca J, Alshehry Y. The immediate psychological response of the general population in Saudi Arabia during COVID-19 pandemic: a cross-sectional study. J Infect Public Health, 2021; 14:1–8. CrossRef
Kamusheva M, Ignatova D, Golda A, Skowron A. The potential role of the pharmacist in supporting patients with depression—a literature-based point of view. Integr Pharm Res Pract, 2020; 9:49–63. CrossRef
Li J, Yang Z, Qiu H, Wang Y, Jian L, Ji J, Li K. Anxiety and depression among general population in China at the peak of the COVID-19 epidemic. World Psychiatry, 2020; 19(2):249–50. CrossRef
Liu Q, He H, Yang J, Feng X, Zhao F, Lyu J. Changes in the global burden of depression from 1990 to 2017: findings from the Global Burden of Disease study. J Psychiatr Res, 2020; 126:134–40. CrossRef
Marasine N, Sankhi S, Lamichhane R, Marasini NR, Dangi NB. Self-reported antidepressant drug side effects, medication adherence, and its associated factors among patients diagnosed with depression at the Psychiatric Hospital of Nepal. Depress Res Treat, 2020. [ONLINE]. Available via https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7593732/ CrossRef
NCPRMP. National Council on prices and reimbursement of medicinal products. [ONLINE]. Available at https://portal.ncpr.bg/registers/pages/register/archive.xhtml
NHIF. Reports for the number of patients and the reimbursement amount during 2019-2020. [ONLINE]. Available via https://www.nhif.bg/page/218
NSI. National Statistical Institute of Bulgaria. Population by districts, place of residence and gender. [ONLINE]. Available at https://www.nsi.bg/bg/content/2975/
OECD/EU. Health at a Glance: Europe 2018: State of Health in the EU Cycle, OECD Publishing, Paris, France, 2018. [ONLINE]; http://doi.org/10.1787/health_glance_eur-2018-en CrossRef
Order RD -01-124/ 13.03.2020. [ONLINE]. Available via https://www.mh.government.bg/media/filer_public/2020/03/13/rd-01-124-vuvejdane-protiepidemichni-merki.pdf
Orsolini L, Tomasetti C, Valchera A, Iasevoli F, Buonaguro EF, Fornaro M, Fiengo ALC, Martinotti G, Vellante F, Matarazzo I, Vecchiotti R, Perna G, Di Nicola M, Carano A, Di Bartolomeis A, De Giannantonio M, De Berardis D. Current and future perspectives on the major depressive disorder: focus on the new multimodal antidepressant vortioxetine. CNS Neurol Disord Drug Targets, 2017; 16(1):65–92; http://doi.org/10.2174/1871527315666161025140111 CrossRef
Peiró S, Meneu R. Economic crisis and healthcare system epicrisis. Aten Primaria, 2011; 43:115–6. CrossRef
Psederska E, Vasilev G, DeAngelis B, Bozgunov K, Nedelchev D, Vassileva J, al’Absi, M. Resilience, mood, and mental health outcomes during the first wave of the COVID-19 pandemic in Bulgaria. PsyArXiv 2021. [ONLINE]. Available via https://psyarxiv.com/8nraq/ CrossRef
Smith BJ, Lim MH. How the COVID-19 pandemic is focusing attention on loneliness and social isolation. Public Health Res Pract, 2020. [ONLINE]. Available via https://pubmed.ncbi.nlm.nih.gov/32601651/ CrossRef
Soleymani F, Taheri F, Roughead E, Nikfar S, Abdollahi M. Pattern of antidepressant utilization and cost in Iran from 2006 to 2013 in comparison with other countries. J Epidemiol Glob Health, 2018; 8(3–4):213–9; http://doi.org/10.2991/j.jegh.2018.06.101 CrossRef
Uvais NA. Psychological Impact of the COVID-19 Pandemic Among the Elderly: A Case Series From India. Prim Care Companion CNS Disord, 2020. [ONLINE]. Available via https://www.psychiatrist.com/pcc/covid-19/psychological-impact-of-covid-on-the-elderly/ CrossRef
WHO Collaborating Centre for Drug Statistics Methodology. Collaborating Centre for Drug Statistics Methodology guidelines for ATC classification and DDD assignment 2018. World Health Organization, Oslo, Norway, 2017. [ONLINE]. Available via https: https://www.whocc.no/atc_ddd_index_and_guidelines/guidelines/
World Health Organization. Depression and other common mental disorders: global health estimates. World Health Organization, Geneva, Switzerland, 2017. [ONLINE]. Available via https://www.who.int/mental_health/management/depression/prevalence_global_health_estimates/en/