INTRODUCTION
In India, fish being the most common seafood is the root cause of several types of seafood poisoning. Most of the seafood poisoning is not reported and the ones which are reported are due to the extreme severity and complications that have occurred. Recent figures estimate that 1%–6% of foodborne illnesses are due to seafood (James, 2006). Poisonous fishes are subdivided into Ichthyosarcotoxic fish, which have toxins in their flesh, Ichthyohemotoxic fish, have toxic blood, and Ichthyo-toxic fish, which have toxins primarily in their gonads (Pillay, 2013). Contaminated fish contain natural toxins and may cause illnesses if consumed. Majority of the toxins are produced by phytoplankton, a form of naturally occurring marine algae. These algae accumulate in the fish that are nontoxic and become poisonous fish if they feed on the algae or if they eat the other fish that have already consumed the poisonous algae. It is important to note that the historical occurrences of natural toxin and its distribution vary with time. Hence, it is important to create awareness among the people (World Health Organization, 2002). Formaldehyde has been classified in 2004 as a Group 1 carcinogen by the International Agency for Cancer Research and it is a very reactive chemical under the family aldehyde, where the liquid form is formalin and the gaseous form is formaldehyde, which is colorless, irritant, poisonous, pungent, and inflammable. Formaldehyde can be added as a preservative to foods and vegetables, and also can be used as a disinfectant (Noordiana et al., 2011). The toxic profiles of the fish in human beings are enlisted in Table 1. The various literature studies related to fish poisoning is shown in Figure 1. The main objective of this review is to highlight the various types of fish poisoning and its management.
TYPES OF FISH POISONING
Most of the fish toxicity is divided into five forms, including scombroid poisoning, ciguatera poisoning, tetrodotoxin poisoning, mercury poisoning, and shellfish poisoning.
Scombroid poisoning
Scombroid poisoning was first reported in 1799 in Britain (Morrow et al., 1991), also known as histamine fish poisoning, belongs to the family Scombridae. The others of this family include tuna, bonito, mackerel, needlefish, amberjack, wahoo, saurie, kingfish, albacore, blue fish, dolphin, mahi mahi, herring, swordfish, and Bombay duck. Food poisoning in humans is caused by the consumption of contaminated scombroid fish, with early symptoms occurring within 5–10 minutes and progressing to severe symptoms within 1–2 hours. When histamine toxin is present in the flesh of the fish, it is called Ichthyosarcotoxicosis (Scombroid). Fresh fish from the sea generally have no toxins; however, due to improper refrigeration, bacterial count increases in the flesh of the fish, and this leads to an endogenous breakdown of histidine to histamine resulting in toxin production, which does not get destroyed in cooking (Lerke et al., 1978; Pillay, 2013; Taylor and Eitenmiller, 1986). Histamine-mediated symptoms are erythema of the face, urticarial (hives), pruritis (itchy skin), dermal flushing, diaphoresis (sweating), burning feeling in the mouth, dizziness, and abdominal cramps. The most common clinical manifestations of scombroid poisoning are vomiting and diarrhea. Tachycardia, bradycardia, hypotension, and respiratory distress develop rarely. Scombroid fish is considered to be potentially harmful if the amount of histamine exceeds more than 5 mg/100 g of fish. A new study shows that mackerel and herring fish that were stored in ice for 9 days were found to contain <5 mg% histamine (Bartholomew et al., 1987; Murray et al., 1982). The capillary electrophoretic assay is the recommended method to estimate histamine level in the fish. Its severity is classified as mild, moderate, and severe. At the early stages of treatment, activated charcoal is useful; successful first-line treatment is cimetidine; in supportive management, oxygen, IV fluids, adrenaline, and nebulized bronchodilators are used (Lerke et al., 1978). The methods that can be used to reduce the risk of poisoning are avoiding the use of a longline method of fishing, maintenance of refrigeration during marketing and distribution, and maintaining a temperature of <32°F or <0°C (Food and Drug Administration, 1995).
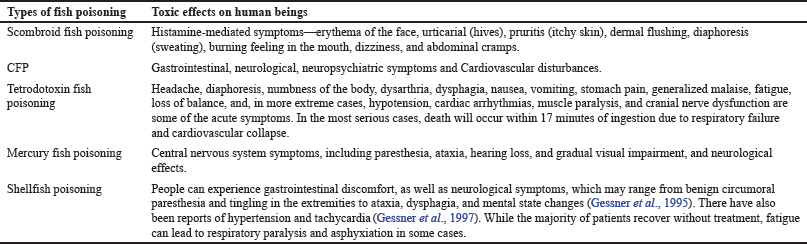 | Table 1. Toxic profile of fish in humans. [Click here to view] |
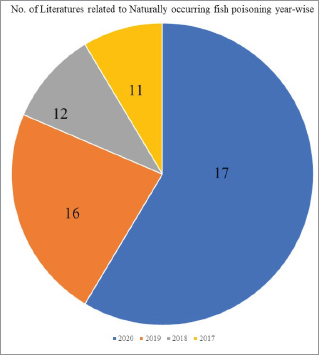 | Figure 1. Number of literature studies related to naturally occurring fish poisoning year-wise. [Click here to view] |
Ciguatera poisoning
Ciguatera fish poisoning (CFP) is often underdiagnosed and underreported, affecting 50,000–200,000 people annually (Dickey and Plakas, 2010). Currently, India is more prone to CFP. On October 3rd, 2016, an outbreak of ciguatera was reported in Mangalore for the first time, where more than 100 people got infected after consuming fish (Outbreak News Today, 2013). Ciguatera toxin is derived from the Gambierdiscus genus of benthic dinoflagellates. Its growth is associated with the microalgae of the coral reefs in tropical and subtropical climates. This family includes barracuda, sea bass, parrotfish, red snapper, grouper, amberjack, kingfish, emperor fish, and surgeonfish. In cell membrane, voltage-gated sodium channels are activated by ciguatera toxin which leads to an increase in sodium ion permeability and depolarization in nerve cell, and their incubation period is 2–6 hours. This depolarization of nerve cells is thought to be the cause of the neurological symptoms linked to CFP. This poison is characterized by gastrointestinal, neurological, and neuropsychiatric symptoms and cardiovascular disturbances. Sweating, stomach cramps, numbness in the mouth, tongue, and throat, metallic taste, chills, headache, diarrhea, and convulsions are some of the symptoms. Enzyme-linked immune sorbent assay, high-performance liquid chromatography (HPLC), and rapid dipstick immunobead assays are used to confirm the presence of ciguatera toxins (Friedman et al., 2008; Pillay, 2013). Deoxyribonucleic acid barcoding is an essential tool to control ciguatera toxin poisoning and to improve monitoring of fish trade and safety (Schoelinck et al., 2014). The mainstay treatment is IV mannitol, which is an effective antidote. The prescribed dosage is 0.5–1 g/kg of 20% solution given over 30–45 minutes. Decontamination with activated charcoal and catharsis within 2 hours of ingestion can be helpful. Atropine is used to treat bradycardia and hypotension. Antihistamines and analgesics can be given symptomatically. Dopamine and calcium gluconate are given in case of circulatory shock. Tocainide, meiletine, and amitriptyline are the drugs that are used to resolve neurological symptoms. Foods to be avoided are alcohol, chicken, caffeine, nuts, and pork for 3–6 months or until ciguatera symptoms are resolved (Friedman et al., 2008; Lewis, 2000; Pillay, 2013). Tourists are at the greatest risk when they are not accompanied by an experienced local guide as CFP may cause morbidity among travelers. Avoiding the consumption of the viscera of reef fish which is more than 1.35 kg is considered beneficial (Lewis et al., 1996; Ting and Brown, 2001).
Tetrodotoxin poisoning
In 1909, pufferfish was viewed as the most delicious food in Japan. Dr. Yoshizum Tahara found tetrodotoxin substances in pufferfish (Suehiro, 1994). The tetrodotoxic family is Tetraodontidae. Pufferfish, like balloon fish (Fig. 2a), globefish (Fig. 2b), blowfish, and toadfish, is a species that comes under this family. In Japan, “FUGU” is the common name for pufferfish. These fishes are 1,200 times more potent than cyanide (India Today, 2017). Tetrodotoxin, which is primarily found in the ovary and liver of pufferfish, is a very active neurotoxin that is found in a variety of marine (Rodríguez et al., 2012) and terrestrial species (Kim et al., 1975). Tetrodotoxin is stored all over the body, but the analogue 6-epi-tetrodotoxin of the red-spotted Notophthalmus viridescens, which have been evaluated by a post-column fluorescent-HPLC system, has been detected in skin and liver extracts (Yotsu-Yamashita et al., 2012). Tetrodotoxin in pufferfish is not naturally synthesized, but is produced with bacteria and enters the food chain (Noguch and Arakawa, 2008). Tetrodotoxin is bound with voltage-gated sodium channels. It blocks nerve and muscle conduction and the flow of sodium ions through the channel and prevents the action potential generation and propagation. It increases sodium and potassium permeability associated with nerve excitation (Lee and Ruben, 2008). Symptoms in patients develop within 30 minutes and the incubation period is 6–24 hours (Yang et al., 1996). Headache, diaphoresis, numbness of the body, dysarthria, dysphagia, nausea, vomiting, stomach pain, generalized malaise, fatigue, loss of balance, and, in more extreme cases, hypotension, cardiac arrhythmias, muscle paralysis, and cranial nerve dysfunction are some of the acute symptoms. In the most serious cases, death will occur within 17 minutes of ingestion due to respiratory failure and cardiovascular collapse (William and Shepherd, 2001). Diagnosis is carried out by mouse bioassay, fluorescent spectrometry, HPLC, liquid chromatography-mass spectrometry, and immunoassay method. There is no specific antidote to treat tetrodotoxin poisoning. Decontamination by activated charcoal is useful. To regain motor strength, IV edrophonium (10 mg) or IM neostigmine (0.5 mg) may be effective. Artificial ventilation is required. Because the toxin has a low molecular weight, is water-soluble, and is not significantly bound to protein; also, hemodialysis may be effective (Pillay, 2013). Due to global warming, the water temperature rises and, therefore, tetrodotoxin contamination of fish occurs. This point must be carefully considered from the standpoint of food hygiene and future management.
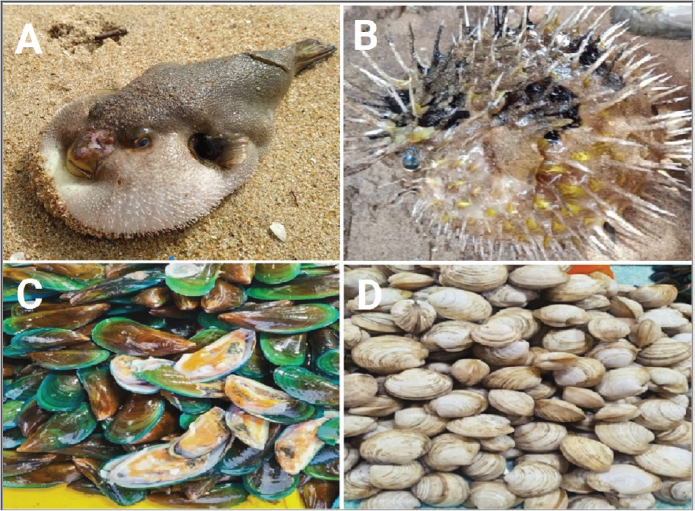 | Figure 2. (a) Balloon Fish, (b) Globe Fish, (c) Oysters, (d) Cockles. [Click here to view] |
Mercury fish poisoning
The health risks of mercury fish poisoning are well known, and the outbreak of Minamata disease in Japan in 1956 brought it to the attention of the entire world. In this case, methyl mercury was released into the nearby shore as a byproduct of acetaldehyde production in a fertilizer factory, polluting the marine environment. Approximately 5,000 people died or suffered illnesses from seafood from the same region. In Iraq, Iran, and Tanzania, mercury poisoning was reported later. As a result, the significance of mercury as an environmental toxin has been highlighted, as evidenced by the Minamata Convention on Mercury’s conclusion. As the metal migrates and circulates globally, international cooperation has become increasingly important in addressing the mercury problem (Ye et al., 2016). In India, high mercury content is found in fishes of Kodaikanal Lake and Periyakulam ponds due to leakage from the contaminated thermometer factory (Kodaikanal Mercury Poisoning, 2017). Mercury alters intracellular calcium balance and membrane potential, disturbing or inhibiting enzyme action, inducing oxidative stress, and inhibiting protein synthesis. Consumption of fish containing high levels of organic mercury, such as tuna, can result in methyl mercury poisoning and a variety of abnormal central nervous system symptoms, including paresthesia, ataxia, hearing loss, and gradual visual impairment. Total blood cell count, electrolyte assays, and renal and hepatic function measures are among the laboratory tests used to determine mercury intoxication The evaluations will also be carried out using electrocardiography, pulmonary function testing, cardiovascular surveillance, electroneuromyography, and neuropsychological tests. Chelation therapy is the most common medical treatment for reducing metal toxicity. Long-term treatment may be required to manage the effects of mercury poisoning, such as neurological effects (Al-Saleh et al., 2016).
Shellfish poisoning
Shellfish poisoning is classified into three types: paralytic shellfish poisoning, neurotoxic shellfish poisoning, and amnestic shellfish poisoning.
Paralytic shellfish poisoning
Paralytic shellfish poisoning is a foodborne disease that typically occurs after saxitoxin-contaminated shellfish are consumed. During toxic algae blooms, dinoflagellates of the genera Alexandrium feed on molluscan bivalves and other shellfish, concentrating the toxin and making it unsafe to consume (Etheridge, 2010). After consuming shellfish contaminated with toxic levels of saxitoxin, symptoms will appear within an hour. Patients can experience gastrointestinal discomfort as well as neurological symptoms, which may range from benign circumoral paresthesia and tingling in the extremities to ataxia, dysphagia, and mental state changes (Gessner et al., 1995). The majority of patients describe a sensation of “floating” or dissociation. There have also been reports of hypertension and tachycardia (Gessner et al., 1997). While the majority of patients recover without treatment, fatigue can lead to respiratory paralysis and asphyxiation in some cases. There are currently no antidotes for saxitoxin, but supportive management is the primary objective of treatment (Etheridge, 2010). Poisoning by shellfish is common and most cases are either of the gastrointestinal type due to bacterial or viral contamination or the hypersensitivity type (Etheridge, 2010; Gessner et al., 1995). Electromyography confirms that the toxin inhibits neuromuscular transmission in the motor axon and muscle membrane. At a molecular level, saxitoxin (like tetrodotoxin, another marine poison) blocks sodium channels in excitable membranes, preventing the propagation of impulses (Etheridge, 2010). The clinical manifestations of paralytic shellfish poisoning are distinct, beginning with numbness of the lips, tongue, and fingertips within minutes of ingestion of the poisoned shellfish, and progressing to numbness of the legs, arms, and neck, as well as general muscular disorder. Other symptoms commonly reported include a sense of lightness (as if floating on air), dizziness, weakness, drowsiness, incoherence, and headache. Throughout their illness, the majority of patients remain calm and conscious. Respiratory distress and muscular paralysis are the final stages of the disorder and can occur anytime within 2–12 hours after ingestion (Schantz, 1971). If the patient is found immediately after eating the poisoned shellfish, the toxin should be removed by gastric emesis or gastric lavage, followed by activated charcoal treatment, which should be used liberally to block further absorption of the poison (Pillay, 2013; Rand et al., 1977).
Neurotoxic shellfish poisoning (NSP)
The consumption of molluscan shellfish, such as oysters (Fig. 2c), cockles (Fig. 2d), whelks, and clams, contaminated with brevetoxins causes neurotoxic shellfish poisoning; these are a group of more than 10 natural neurotoxins produced by the marine Dinoflagellate and Karenia brevis, also known as Gymnodinium breve and Ptychodiscus brevis (Daugbjerg et al., 2000). The diagnosis of NSP is based upon the clinical presentation, along with a carefully elicited history that includes recent consumption of molluscan shellfish. The clinical manifestations begin within few minutes to 18 hours after the consumption of contaminated shellfish. A meantime of onset of 3–4 hours has been reported in the few documented outbreaks (Morris et al., 1991). NSP causes a range of signs and symptoms, both neurological and gastrointestinal. Mostly multiple symptoms have been reported. Mild to moderate symptoms are nausea, vomiting, and diarrhea, although these may not be the chief presenting complaints. NSP most frequently produces numbness and tingling in the lips, mouth, and face, as well as numbness and tingling in the extremities. Slurred speech, headache, pupil dilation, and overall fatigue are also commonly reported. Throat and chest heaviness have also been reported. Few individuals have had respiratory discomfort and distress, with a handful of cases requiring ventilatory support. The characteristic cluster of both gastrointestinal and neurological symptoms occurs approximately at the same time, with the neurological symptoms lasting longer than the gastrointestinal discomfort (Wu and Narahashi, 1998). Treatment for NSP involves mainly supportive care. Fluid replacement, observation of respiratory functions, and the administration of sedatives and pain mitigation are the main management techniques as there is no specific antidote available for brevetoxins. Gastrointestinal decontamination with activated charcoal for patients presenting within the first 4 hours post-ingestion has been recommended, but there is no clinical evidence supporting a significantly better or lessened course of illness. Given the similar toxin structure between brevetoxin and ciguatoxin, mannitol (the recommended treatment in ciguatera poisoning) may be useful in early treatment (Blythe et al., 2000; Friedman et al., 2008).
Amnestic shellfish poisoning
Domoic acid is a key factor with amnesic shellfish poisoning involved in isodomoic acid D, isodomoic acid E, and isodomoic acid F (Fig. 3). All of these are plankton products. It acts as a glutamate receptor agonist and has a high affinity for quisqualate glutamate receptors. The glutamate receptor opens Na+ ion channels in the postsynaptic membrane, causing it to depolarize. This increases Ca ion permeability, which eventually leads to cell death (Mattei et al., 1999). The DA toxicity process takes place primarily in mitochondria, where uncoupling of oxidative phosphorylation occurs, resulting in cell swelling and, eventually, lysis due to decreased membrane permeability. DA showed no mutagenic action on the pulmonary fibroblast hamster V79 cells, apart from neurotoxic and gastro toxic activity (Hampson et al., 1992). Within 24 hours, symptoms such as nausea, vomiting, headache, diarrhea, or abdominal cramps are observed, or at least one of the following neurological symptoms or signs occur, causing confusion, memory loss, disorientation, or other serious neurologic signs such as seizures, coma, or death (Rogers and Boyes, 1989). DA exposures lead to a strong c-fos induction in the brain, a reduced cardiac impact, and no kidney or liver effect. The induction of c-fos in the brain has been traced to two main areas: the brain stem and the limbic system. Vomiting and memory loss are the results of these brain effects (Todd, 1993). Mouse bioassay and HPLC are methods to find out the amnestic shellfish poisoning. Treatment includes administration of activated charcoal. Phenobarbital and diazepam is given to treat convulsion. Antiemetics like metoclopramide can be given for nausea and vomiting. I.V hydration with lactated ringer or normal saline is effective (Peng et al., 1994; Pillay, 2013). Avoiding contaminated shellfish, also known as “red tides” or “brown tides,” as they carry high risk viral and bacterial infection, is one of the methods of prevention.
 | Figure 3. Amnestic fish poisoning containing domoic acid. [Click here to view] |
Prevention from formalin preservatives
Formalin is a preservative that is used to keep fish safe from pathogens. Formalin or formaldehyde is used as a preservative, during the storage and transportation of fishes. This compound also aids in the preservation of seafood by reacting with protein and causing muscle toughness (Bianchi et al., 2007; Olney, 1990). Formalin is effectively used to kill parasites on gills, skin, and fins. Formalin is an aquatic chemotherapeutic that is approved in the United States and Canada. Under the Canada Feed Act, formaldehyde is registered as a feed ingredient (Sotelo et al., 1995). However, due to its association with oncogenesis, formalin use in aquaculture has not been approved in Australia, Europe, or Japan. Various methods have been described for the detection of formaldehyde in fish and other food products, such as spectrophotometric methods and chromatographic methods, which include gas chromatography-mass spectrometry, liquid chromatographic methods, enzyme-based methods, and other sensor-based techniques. Apart from the available instrument-based methodologies, some commercial kits are also available which provide qualitative information on the presence/absence of formaldehyde in fish; however, most of them are patented or commercialized and the exact mechanism by which they work is unknown. To detect whether the fishes that are consumed are layered with formalin or not, the Central Institute of Fisheries Technology, Kochi, has come up with a test kit, which will hit the markets in a month. These kits have 25 strips and each strip would cost Rs. 3 (Schnick et al., 1997).
CONCLUSION
Most people are unaware and not cautious about seafood poisoning. Therefore, it has become essential to improve the understanding and to create awareness among the society regarding aquatic toxicity. Physicians have to be educated to identify fish poisoning and manage the same. To further explore these results, more specific data on effects, exposure, and ecological factors are required. Additional ecological data on changes in the distribution of suitable habitat for dinoflagellates as a result of sea surface temperature warming, coral blanking, and storm destruction, as well as their overlap, are required.
ACKNOWLEDGMENTS
The authors acknowledge the Department of Pharmacy Practice, JSS College of Pharmacy, Ooty, for their support.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All the authors are eligible to be an author as per the international committee of medical journal editors (ICMJE) requirements/guidelines.
CONFLICT OF INTEREST
The authors of this paper have no conflicts of interest to declare.
FUNDING
There are no funding organizations that supported this review.
LIST OF ABBREVIATIONS
NSPNeurotoxic shellfish poisoning
REFERENCES
Al-Saleh I, Nester M, Abduljabbar M, Al-Rouqi R, Eltabache C, Al-Rajudi T, Elkhatib R. Mercury (Hg) exposure and its effects on Saudi breastfed infant’s neurodevelopment. Int J Hyg Environ Health, 2016; 219(1):129–41. CrossRef
Bartholomew BA, Berry PR, Rodhouse JC, Gilbert RJ, Murray CK. Scombrotoxic fish poisoning in Britain: features of over 250 suspected incidents from 1976 to 1986. Epidemiol Infect, 1987; 99(3):775–82. CrossRef
Bianchi F, Careri M, Musci M, Mangia A. Fish and food safety: determination of formaldehyde in 12 fish species by SPME extraction and GC–MS analysis. Food Chem, 2007; 100(3):1049–53. CrossRef
Blythe DG, Hack E, Washington G, Fleming LE. The medical management of seafood poisoning. In Foodborne disease handbook, New York, NY, 2000, vol 4, pp 311–9.
Daugbjerg N, Hansen G, Larsen J, Moestrup Ø. Phylogeny of some of the major genera of dinoflagellates based on ultrastructure and partial LSU rDNA sequence data, including the erection of three new genera of unarmoured dinoflagellates. Phycologia, 2000; 39(4):302–17. CrossRef
Dickey RW, Plakas SM. Ciguatera: a public health perspective. Toxicon, 2010; 56(2):123–36. CrossRef
Etheridge SM. Paralytic shellfish poisoning: seafood safety and human health perspectives. Toxicon, 2010; 56(2):108–22. CrossRef
Food and Drug Administration. Procedures for the safe and sanitary processing and importing of fish and fishery products. Fed Regist, 1995; 60:65096–202.
Friedman MA, Fleming LE, Fernandez M, Bienfang P, Schrank K, Dickey R, Bottein MY, Backer L, Ayyar R, Weisman R, Watkins S. Ciguatera fish poisoning: treatment, prevention and management. Mar Drugs, 2008; 6(3):456–79. CrossRef
Gessner BD, Bell P, Doucette GJ, Moczydlowski E, Poli MA, Van Dolah F, Hall S. Hypertension and identification of toxin in human urine and serum following a cluster of mussel-associated paralytic shellfish poisoning outbreaks. Toxicon, 1997; 35(5):711–22. CrossRef
Gessner BD, Middaugh JP. Paralytic shellfish poisoning in Alaska: a 20-year retrospective analysis. Am J Epidemiol, 1995; 141(8):766–70. CrossRef
Hampson DR, Huang XP, Wells JW, Walter JA, Wright JL. Interaction of domoic acid and several derivatives with kainic acid and AMPA binding sites in rat brain. Eur J Pharmacol, 1992; 218(1):1–8. CrossRef
India Today. This fish is 1200 times more poisonous than cyanide, and it’s a delicacy in Japan. 2017. Available via https://www.indiatoday.in/food-drink/food/story/fugu-japan-poisonous-fish-cyanide-pufferfish-delicacy-lifefd-958193-2017-01-31 (Accessed 5 April 2020)
James D. Color atlas of human poisoning and envenoming. CRC Press, Boca Raton, FL, 2006. CrossRef
Kim YH, Brown GB, Mosher FA. Tetrodotoxin: occurrence in atelopid frogs of Costa Rica. Science. 1975; 189(4197):151–2. CrossRef
Kodaikanal Mercury Poisoning. High mercury levels in fish from Kodai lake, Periakulam Ponds; IIT-Hyderabad Study Cautions Fish Consumers. 2017. Available via http://kodaimercury.org/high-mercury-levels-fish-kodai-lake-periakulam-ponds-iit-hyderabad-study-cautions-fish-consumers-2/ (Accessed 8 April 2020).
Lee CH, Ruben PC. Interaction between voltage-gated sodium channels and the neurotoxin, tetrodotoxin. Channels, 2008; 2(6):407–12. CrossRef
Lerke PA, Werner SB, Taylor SL, Guthertz LS. Scombroid poisoning: report of an outbreak. Wes J Med, 1978; 129(5):381.
Lewis R, King G. Williamson JA, Fanner PJ, Burnett JW, Rifkin JF. Ciguatera fish poisoning. University of New South Wales Press, Sydney, Australia, 1996.
Lewis RJ. Ciguatera management. SPC Live Reef Fish Inf Bull, 2000; 7:11–3.
Mattei C, Molgo J, Legrand AM, Benoit E. Ciguatoxins and brevetoxins: dissection of the neurobiological actions. J Soc Biol, 1999; 193(3):329–44. CrossRef
Morris PD, Campbell DS, Taylor TJ, Freeman JI. Clinical and epidemiological features of neurotoxic shellfish poisoning in North Carolina. Am J Public Health, 1991; 81(4):471–4. CrossRef
Morrow JD, Margolies GR, Rowland J, Roberts LJ. Evidence that histamine is the causative toxin of scombroid-fish poisoning. N Engl J Med, 1991; 324(11):716–20. CrossRef
Murray CK, Hobbs G, Gilbert RJ. Scombrotoxin and scombrotoxin-like poisoning from canned fish. Epidemiol Infect, 1982; 88(2):215–20. CrossRef
Noguch T, Arakawa O. Tetrodotoxin–distribution and accumulation in aquatic organisms, and cases of human intoxication. Mar Drugs, 2008; 6(2):220–42. CrossRef
Noordiana N, Fatimah AB, Farhana YC. Formaldehyde content and quality characteristics of selected fish and seafood from wet markets. Int Food Res J, 2011; 18(1):125–36.
Olney JW. Excitotoxicity: an overview. Can Dis Wkly Rep, 1990; 16:47–57.
Outbreak News Today. India reports first ciguatera poisoning outbreak, more than 100 affected. 2013. Available via http://outbreaknewstoday.com/india-reports-first-ciguatera-poisoning-outbreak-more-than-100-affected-42568/ (Accessed 21 March 2020)
Peng YG, Taylor TB, Finch RE, Switzer RC, Ramsdell JS. Neuroexcitatory and neurotoxic actions of the amnesic shellfish poison domoic acid. Neuroreport, 1994; 5(8):981–5. CrossRef
Pillay V. Modern medical toxicology. 4th edition, Jaypee Brothers Pvt. Ltd., New Delhi, India, 2013, p 535.
Rand PW, Lawrence FH, Pirone Jr LA, Lavigne JR, LaCombe E. The application of charcoal hemoperfusion to paralytic shellfish poisoning. J Maine Med Assoc, 1977; 68(5):147.
Rodríguez P, Alfonso A, Otero P, Katikou P, Georgantelis D, Botana LM. Liquid chromatography–mass spectrometry method to detect tetrodotoxin and its analogues in the puffer fish Lagocephalus sceleratus (Gmelin, 1789) from European waters. Food Chem, 2012; 132(2):1103–11. CrossRef
Rogers CG, Boyes BG. Evaluation of the genotoxicity of domoic acid in a hepatocyte-mediated assay with V79 Chinese hamster lung cells. Mutat Res, 1989; 226(3):191–5. CrossRef
Schantz EJ. The dinoflagellate poisons. In: Kadis S, Ceigler A, Ajl SJ, Acad PR (ed.). Microbial toxins. Algal and Protein Toxins, New York, NY, 1971, vol 7, pp 3:26–8. CrossRef
Schnick RA, Alderman DJ, Armstrong R, Gouvello RL. Worldwide aquaculture drug and vaccine registration progress. Proceeding of the Workshop at the EAFP 8th International Conference on Disease of Fish and Shellfish, (ICDFS’97), Edinburgh, Scotland, 1997, pp 14–9.
Schoelinck C, Hinsinger DD, Detta? A, Cruaud C, Justine JL. A phylogenetic re-analysis of groupers with applications for ciguatera fish poisoning. PLoS One, 2014; 9:8. CrossRef
Sotelo CG, Pineiro C, Perez-Martin RI. Denaturation of fish proteins during frozen storage: role of formaldehyde. Z Lebensm Unters Forsch, 1995; 200(1):14. CrossRef
Suehiro M. Historical review on chemical and medical studies of globefish toxin before World War II. Yakushigaku Zasshi, 1994; 29(3):428–34.
Taylor SL, Eitenmiller RR. Histamine food poisoning: toxicology and clinical aspects. Crit Rev Toxicol. 1986; 17(2):91–128. CrossRef
Ting JY, Brown AF. Ciguatera poisoning: a global issue with common management problems. Eur J Emerg Med, 2001; 8(4):295–300. CrossRef
Todd EC. Domoic acid and amnesic shellfish poisoning-a review. J Food Prot, 1993; 56(1):69–83. CrossRef
William SH, Shepherd S. Scombroid, ciguatera, and other seafood intoxications. Clin Toxicol, 2001; 1st Edition:959–68.
World Health Organization. Formaldehyde. Food and drug administration. Concise international chemical assessment, document 40. World Health Organization, Geneva, Switzerland, 2002.
Wu CH, Narahashi T. Mechanism of action of novel marine neurotoxins on ion channels. Annu Rev Pharmacol Toxicol, 1988; 28(1):141–61. CrossRef
Yang CC, Liao SC, Deng JF. Tetrodotoxin poisoning in Taiwan: an analysis of poison center data. Vet Hum Toxicol, 1996; 38(4):282–6.
Ye BJ, Kim BG, Jeon MJ, Kim SY, Kim HC, Jang TW, Chae HJ, Choi WJ, Ha MN, Hong YS. Evaluation of mercury exposure level, clinical diagnosis and treatment for mercury intoxication. Ann Occup Environ Med, 2016; 28(1):1–8. CrossRef
Yotsu-Yamashita M, Gilhen J, Russell RW, Krysko KL, Melaun C, Kurz A, Kauferstein S, Kordis D, Mebs D. Variability of tetrodotoxin and of its analogues in the red-spotted newt, Notophthalmus viridescens (Amphibia: Urodela: Salamandridae). Toxicon, 2012; 59(2):257–64. CrossRef