INTRODUCTION
Falls are a major public health problem among older people (OP). The World Health Organization defined falls as “an event which results in a person coming to rest inadvertently on the ground or floor or other lower-level” (Falls, 2021). Risk factors of falls in OP include increasing age, balance and gait impairment, cognitive decline, multimorbidity, and environmental factors (Ambrose et al., 2013; Fuller, 2000; Pfortmueller et al., 2014). Previous studies reported that the prevalence of falls among OP was approximately 30% in England, Brazil, and Indonesia (Gale et al., 2018; Siqueira et al., 2011; Susilowati et al., 2020). In Malaysia, 24.3%–32.8% of OP residing in nursing homes (Ghazi et al., 2017; Hami et al., 2019; Kioh and Rashid, 2018) and 14.1%–19.7% community-dwelling OP had fallen (Alex et al., 2018; Hami et al., 2019; Ibrahim et al., 2017; Sahril et al., 2020). Fall-related injuries such as fractures, hematoma, and severe laceration are the main consequences of falls that can result in disability, activity limitation, and dependency (Berg and Cassells, 1992).
Fall-risk-increasing drugs (FRIDs) such as psychotropics, benzodiazepines (BZD), antipsychotics, and antihypertensives have been associated with falls (Huang et al., 2012; Seppala et al., 2018). FRIDs may increase the risk of falling (ROF) due to their side effects on the central nervous system or by causing orthostatic hypotension (Milos et al., 2014). Despite the association between FRIDs and falls, the drugs are commonly used by OP who are at ROF (Beunza-Sola et al., 2018; Chen et al., 2012; Liew et al., 2019; Marvin et al., 2017; Mazlan et al., 2021; Sjöberg et al., 2010). Studies conducted in England, Spain, and Sweden reported that 65%–93% of OP who needed medical attention due to falls were using FRIDs (Beunza-Sola et al., 2018; Marvin et al., 2017; Sjöberg et al., 2010). A survey in Malaysia showed that 73.7% out of 72 OP residing in residential aged care facilities used FRIDs, with more than half of the FRID users (54.2%) already identified to be at ROF (Mazlan et al., 2021).
Previous studies showed that the awareness among OP of the association of FRIDs and falls may be lacking, and they commonly overestimate the benefits of medications and underestimate the potential harms (Bell et al., 2017; Laing et al., 2011). In a qualitative study among Norwegian OP aged >65 years who used FRIDs, none of them were familiar with the term FRIDs, and they did not perceive medications as a prominent risk factor for falls. In another survey in Canada among OP aged ≥60 years, only about 45% and 24% of them were aware that hypnotics and anxiolytics, respectively, may increase their ROF (Wien et al., 2006). Due to the low awareness of OP about the influence of medications on increasing the ROF, it is recommended that healthcare providers (HCPs) regularly educate OP to make sure they recognize the side effects of FRIDs such as dizziness and unsteadiness (Bell et al., 2017).
Professional bodies such as the European Geriatric Medicine Society (EuGMS) Task and Finish group on FRIDs recognized the low awareness of FRIDs among OP as an important problem that warrants intervention from HCPs (Seppala et al., 2019). The EuGMS Task and Finish group on FRIDs support more efforts for the dissemination of knowledge of FRIDs to OP through various platforms, such as the media, and education materials (EMs), such as brochures and posters (Seppala et al., 2019). Nevertheless, at present, most available EMs in the context of fall prevention generally include a combination of topics that cover the multiple risk factors of falls with little or lack of discussion on medications (Andrade et al., 2017). Additionally, EMs that focus on FRIDs developed for Malaysian OP are currently lacking.
The present study employed a focus group discussion (FGD) with the objectives of seeking the opinions of Malaysian key stakeholders in OP care, i.e., geriatricians, pharmacists, and nurses, about EMs on FRIDs. Specifically, we aimed to seek the HCPs’ perceptions on the appropriate content of EMs on FRIDs, the potential benefits and limitations, and the level of support for the development of the EMs. Findings from this study may assist the development of EMs on FRIDs that are relevant, suitable, and useful for Malaysian OP.
MATERIALS AND METHODS
Study design
A descriptive qualitative study using FGD among key stakeholders in OP care, namely geriatricians, pharmacists, and nurses, was conducted. The FGD method was utilized to obtain information about the ideas and opinions of individuals when little preknowledge about an issue existed, especially in the local context, and to test a new product or concept through group thinking and brainstorming (Kitzinger, 1995; Krueger, 2006). FGD can provide in-depth information about the topic discussed through detailed probing of the issues. The exchanges of ideas and opinions among the participants can generate new ideas (Newcomer et al., 2015). The Consolidated Criteria for Reporting Qualitative Research (COREQ) checklist was used as a quality check for the study and to guide the reporting (Tong et al., 2007). This study was approved by the Research Ethics Committee of Universiti Teknologi MARA, Malaysia [REC/01/2021 (MR/34)].
Settings and participants
Four FGDs were conducted separately 1 week apart in February 2021 to seek HCPs’ opinions on the various aspects of EMs on FRIDs. As suggested by Hennink et al. (2019), four focus groups were sufficient to identify a range of new issues. The FGDs were conducted online due to the movement control order enforced during the study period due to the coronavirus pandemic. In this study, participants were purposively selected using maximum variation sampling. Malaysian geriatricians, pharmacists, and nurses with at least 3 years of clinical experience who agreed to participate in this study were included in the sample. Additional inclusion criteria for the pharmacists were a certification in geriatric pharmacy or being part of a fall intervention team for at least 6 months. Additional inclusion criterion for the nurses was a completion of the postbasic program in gerontology.
In the beginning, names of potential participants were identified from the researchers’ professional network. Subsequent participants were recruited using the snowball sampling technique. Overall, 24 HCPs were invited to participate in the FGD, with 21 of them confirming their participation. Of all the HCPs contacted, three did not respond to the invitation.
Data collection
In this study, the FGD was conducted using the Google Meet online application led by the principal investigator (MSS). The FGDs were moderated in English, but participants could speak in either the English or the Malay language. Before each FGD session, the interviewer introduced himself and explained the purpose of the study. The FGD participants were informed that a voice recorder was being used, and they were ensured of confidentiality and anonymity. The participants were also reminded that their participation in the study is voluntary, and they could withdraw themselves from the FGD at any time. The FGDs were guided using a set of semistructured interview questions developed by the research team (Table 1). Each FGD lasted about 90 minutes. Field notes were taken by the interviewer. Each participant received an honorarium of MYR100 (~USD24). Data saturation was considered achieved when the data collected did not contribute to new information on the opinions of the HCPs about the study topic (Hennink et al., 2019).
Discussion questions
A semistructured interview guide was developed and used in the FGDs (Table 1). Three academic pharmacists who are experienced in clinical pharmacy and pharmacy practice research examined the face validity of the discussion questions to ensure they were suitable and relevant. Participants’ information and demographic details (e.g., gender, ethnicity, years of working experience, and working place) were collected using an online demographic survey form developed using the Google Forms application.
Data analysis
Audio recordings of each FGD were transcribed verbatim by MSS and validated by another author (MSAW). The names of the participants were removed from the transcripts to maintain anonymity. Data were entered into NVivo version 12 and were analyzed line-by-line using thematic analysis. In thematic analysis, transcripts were familiarized through repeated readings to gain an understanding of the data. Opinion statements by the FGD participants were summarized as meaning units. Short explanatory codes were then generated for each meaning unit. Subsequently, all codes were examined to identify the similarities and differences. Similar codes were grouped under relevant themes. Two researchers (MSS and MSAW) who are educated in the thematic analysis processes performed the analysis independently. A good interrater reliability result (95%) (Atkins et al., 2017) was obtained for the coding of the two researchers.
All discrepancies in coding or assignment of codes under themes were discussed and agreed upon among the two researchers. Final codes were discussed among all research team members. For the purpose of reporting, relevant quotes were presented to capture the meaning of the statements provided by the participants. Those quotes that were in the Malay language were translated into English. In this study, the use of a standardized discussion guide, peer and member checking, independent coding, and audit trail throughout the study data collection and analysis enhanced the trustworthiness and credibility of the study findings.
RESULTS
Characteristics of FGD participants
Table 2 shows the characteristics of the FGD participants. Initially, 21 HCPs agreed to participate in the FGD. However, only 19 HCPs consisting of 5 geriatricians, 8 pharmacists, and 6 nurses participated in the study. One geriatrician withdrew from the FGD due to the need to attend to an emergency case, and one had another commitment. Five HCPs participated in each FGD except for the second FGD where four HCPs participated. The age of the HCPs ranged from 29 to 47 years, and the years of working experience ranged from 3 to 20 years.
 | Table 1. Discussion questions used in the FGD. [Click here to view] |
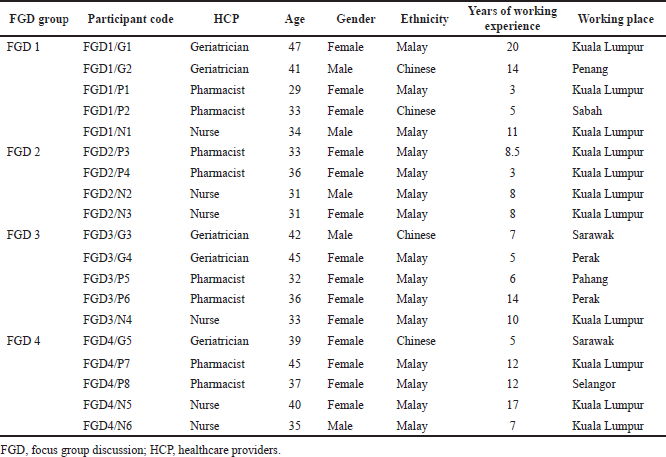 | Table 2. Characteristics of FGD participants. [Click here to view] |
Opinions of HCPs on the level of awareness of OP about FRIDs and EMs on FRIDs
The opinions of the HCPs were categorized into five major themes (Table 3): (1) awareness of OP of medications that can increase their ROF, (2) content for EMs on FRIDs, (3) potential benefits of EMs on FRIDs, (4) concerns and limitations of EMs on FRIDs, and (5) support for EMs on FRIDs. The vast majority of codes (86%) were identified in the first FGD, with a sharp decline in new codes in the following FGDs. The data were deemed to have reached the saturation point as no new theme or subtheme was identified in the fourth FGD. Figure 1 shows the overall findings obtained from the FGD.
Theme 1: Awareness of OP of medications that can increase their ROF
The HCPs consistently agreed that, in general, the majority of OP have low awareness of FRIDs. As mentioned by the HCPs, OP normally blame other causes such as old age, physical limitations, existing diseases/illnesses, and their environments for their falls. Some HCPs stated that falls were perceived by OP as normal. The HCPs commented:
“Majority of them are not aware... oftentimes they blame it on their old age, their painful knees, being too weak, the slippery floor. Rarely do they think it’s from their medications.”—FGD1/G1 (geriatrician, 20 years of working experience)
“They are not aware… For them a fall is normal… as long as they are not admitted, not bleeding, not fractured, they are okay.”—FGD3/P5 (pharmacist, 6 years of working experience)
 | Table 3. Themes identified in the study. [Click here to view] |
 | Figure 1. Themes identified in the study. [Click here to view] |
Some pharmacists highlighted that the low awareness of FRIDs was seen even in OP with a high education level. Two of them mentioned:
“We had highly educated patients… they are literate… but they are still not aware of the risks.”—FGD4/P8 (pharmacist, 12 years of working experience)
“Some are educated but they just know the surface about their medications.”—FGD1/P1 (pharmacist, 3 years of working experience)
The HCPs suggested that HCP–patient communication about the side effects of medications that can potentially increase their ROF could be inadequate, resulting in low awareness among OP of the topic.
Theme 2: Content of EMs on FRIDs
The HCPs stressed the importance of highlighting medications as one of the risk factors of falls since OP generally do not have this knowledge. The HCPs mentioned that an ideal EM on FRIDs must include common medication classes that are linked to falls with an emphasis on their side effects, such as dizziness and unsteadiness, and the complications of falls. Some HCPs believed that information on how medications can cause falls may be beneficial for OP to further enhance their knowledge of FRIDs. The HCPs also highlighted the importance of information to guide OP to self-monitor the side effects of FRIDs they are taking.
Of note, many HCPs emphasized that EMs on FRIDs must include information that can encourage OP to communicate with HCPs about any concerns they have about FRIDs or if they experience any undesirable side effects. This will allow necessary interventions to be performed by the HCPs, such as the provision of additional patient education or changes in a patient’s medications. The pharmacists, in particular, stated that the benefits of medication review should be highly emphasized in the EMs. Some comments from the HCPs are as follows:
“Make sure they know who to refer… if they think they are at risk, consult the doctors or pharmacists.”—FGD1/G1 (geriatrician, 20 years of working experience)
“It’s not just about knowing the drugs and the risks… they need to communicate with the healthcare providers to tell them their problems… so that something can be done.”—FGD1/P2 (pharmacist, 5 years of working experience)
“They should be informed about medication review… they are not aware that they should have their medications reviewed regularly.”—FGD4/P8 (pharmacist, 12 years of working experience)
Theme 3: Potential benefits of EMs on FRIDs
Overall, HCPs agreed that EMs on FRIDs have potential benefits to both the HCPs and OP. An EM on FRIDs was seen as a tool to assist patient education or counseling as it can guide HCPs on the important points to discuss. Several HCPs also believed that the EMs could reduce consultation time. One HCP mentioned:
“I think it would make counseling much easier.”—FGD1/G1 (geriatrician, 20 years of working experience)
More importantly, the HCPs believed that EMs on FRIDs can serve as a tool to promote awareness to OP of FRIDs and to enhance and reinforce their knowledge of the medications. Two HCPs shared their opinions:
“It would improve their understanding and awareness about drugs that cause falls.”—FGD4/P8 (pharmacist, 12 years of working experience)
“It can improve their awareness… and can complement our effort to communicate with patients.”—FGD3/G3 (geriatrician, 7 years of working experience)
The HCPs believe that the awareness of FRIDs among OP will make them more careful and alert about the side effects of those medications. Consequently, with such awareness, the HCPs hope that OP can become more empowered and will come forward to talk with them about their concerns so that they can provide further advice or recommendation.
As shared by the HCPs, many OP had difficulties recalling information on FRIDs provided to them during consultation or counseling due to the multiple medications they are taking. Thus, the HCPs believed that the EMs might reinforce patient education on the drugs as it can be referred to by OP at home or used by family members or caregivers as an information resource on FRIDs. A pharmacist mentioned:
“They can read it again and again… make it easier for them to understand.”—FGD1/P2 (pharmacist, 5 years of working experience)
Theme 4: Concerns and limitations of EMs on FRIDs
Despite the numerous benefits mentioned by the HCPs for EMs on FRIDs, many HCPs were concerned that the details on FRIDs may scare or cause the OP to have a negative perception of their treatment which can potentially cause unwanted implications such as intentional discontinuation of treatment. The HCPs mentioned:
“We don’t want them to have negative thoughts on their medications… or else from being compliant to their medications, they will become incompliant.”—FGD1/P2 (pharmacist, 5 years of working experience)
“We don’t want to scare them… we need to be sensible.”—FGD3/G4 (geriatrician, 5 years of working experience)
Additionally, the HCPs highlighted that information about FRIDs may cause an information burden to the OP, while some others raised concerns that the EMs may be underutilized. The HCPs shared their thoughts:
“They will just put it in their handbag… that’s it.”—FGD1/G1 (geriatrician, 20 years of working experience)
“We have posters, but they don’t look at it.”—FGD4/N5 (nurse, 17 years of working experience)
The HCPs also had the opinion that EMs on FRIDs may not be useful to the OP with low education levels, low literacy, cognitive decline, and poor vision. Some comments from the HCPs are as follows:
“Not all of our patients can read… and some have cognitive impairment.”—FGD4/N6 (nurse, 7 years of working experience)
“Low literacy, low educational level… these become the limitations of the education materials.”—FGD2/P4 (nurse, 7 years of working experience)
The other limitation of the EMs is the language barrier among OP as observed by the HCPs. The HCPs suggested the need for EMs in multiple languages so that OP of different races can benefit from them. One geriatrician highlighted:
“Malaysia is a multiracial country… some people are fluent in Malay, some others in Mandarin or Tamil… so it need to be in various languages.”—FGD3/G3 (geriatrician, 7 years of working experience)
Theme 5: Support for EMs on FRIDs
Despite the mentioned potential limitations of EMs on FRIDs, the HCPs expressed support for the development of the EMs and believed similar support would be received from other HCPs. Additionally, the HCPs believed that EMs on FRIDs might receive support from various key stakeholders such as the government, nongovernmental organizations, and other professional bodies. During the FGDs, the HCPs enthusiastically shared various names of nongovernmental organizations that may potentially support and benefit from the EMs.
DISCUSSION
This paper describes the findings of a qualitative, exploratory study using a pragmatic approach that captures the opinions of Malaysian HCPs about EMs on FRIDs. The overall impression was that HCPs saw the benefits of EMs on FRIDs to both HCPs and OP. The EMs were anticipated as a valuable tool to enhance the awareness of OP of medications that can potentially increase their ROF and to facilitate HCP–patients discussion on the topic. Despite providing support for the development of EMs on FRIDs, HCPs feared that the information on FRIDs may evoke fear among OP that can potentially result in other issues.
In this study, the HCPs believed OP generally had low awareness of the possibility of medications in causing falls, thus presenting a gap in OP’s knowledge, especially those at ROF. Such low awareness of FRIDs and their side effects has also been reported among OP in several previous studies (Bell et al., 2017; Leonetti and Lee, 2014; Loke et al., 2018; Wien et al., 2006).
Ideally, patients should have knowledge of the side effects of their medications as it is an integral part of medication knowledge (Ascione et al., 1986). However, in general, the knowledge of side effects of medications was generally low among OP. Previous studies had shown that between 84% and 96% of OP lacked knowledge of their medication side effects (Barat et al., 2001; Chan et al., 2013; Modig et al., 2009).
As mentioned by our FGD participants, an inadequate discussion about medication side effects among HCPs and patients may contribute to patients having low awareness of their medication side effects. A lack of time and the inclination to prioritize other medication information are some barriers for HCPs to disclose information on medication side effects (Chan et al., 2013).
Thus, EMs on FRIDs can serve as a tool to educate OP about the drugs, including the side effects. This, together with the multiple benefits of EMs on FRIDs mentioned by the FGD participants in this study, may warrant their development. Furthermore, since EMs in the context of falls generally do not adequately cover information on FRIDs or medications as a risk factor for falls (Andrade et al., 2017), EMs on FRIDs can fill the gap in enhancing knowledge of OP of the topic (Wahab, 2015). The EMs can be supplemented with other EMs on non-medication-related risk factors for falls, thus providing OP with the overall knowledge of fall prevention.
The HCPs had concerns about the possibility of inciting fear among OP due to the exposure of information on the potential side effects of FRIDs. Data is inconclusive, but as few authors suggested, the fear of medication side effects may result in treatment refusal (Van Grunsven, 2001) or medication nonadherence (Osterberg and Blaschke, 2005). Arguments from other authors suggested that proper education of patients on medication side effects may help them understand their treatment better, thus promoting medication adherence (Papaioannou et al., 2007; Pasina et al., 2014; Van Grunsven, 2001). Additionally, patient education on medication side effects may create risk perceptions that could result in positive behaviors among patients. For instance, in a study by Martin et al. (2013), a brochure on the risk of BZD had increased the risk perceptions of the drug in 45% of older BZD consumers. Those OP with the increased risk perceptions were noted to be more likely to reread the EM and discuss medication safety with a HCP (Martin et al., 2013). In the context of falls, the awareness and knowledge of FRIDs can help OP to recognize adverse effects of the medications and empower them to communicate and collaborate with HCPs to minimize the risks (Parekh et al., 2018).
For the content of EMs on FRIDs, the FGD participants in the present study suggested the incorporation of information that can serve two main objectives: (1) to enhance the awareness and knowledge of OP about FRIDs, including the side effects, and (2) to encourage OP to communicate with HCPs about FRIDs and have their medications reviewed. As mentioned by our study participants, EMs targeted for OP are frequently neglected or underutilized. Therefore, the EMs should be designed to include easily understood messages about FRIDs that are clear and logical, using effective OP “friendly design” (e.g., bigger fonts, usage of layman’s terms, and graphics) (Clayton, 2009). To ensure the EMs are useful, relevant, and suitable for the OP, the EMs should be reviewed to establish their content validity (Cordeiro et al., 2017). Additionally, a pilot test can be conducted to assess the comprehension of OP of the content of the EMs and their practicality (Kim et al., 2004). A survey among OP on the acceptance of the EMs can also be conducted to reveal their usefulness (Yahya et al., 2020).
Strengths and limitations of the study
A major strength of the study is the use of a qualitative research method to provide in-depth information about the study topic. Additionally, the HCPs included in the present study were key persons in OP care with a wide range of years of working experience. Findings from the study may help in generating information that could be used to inform the future development of EMs on FRIDs.
There are some limitations of the study. We only conducted a small number of FGDs, thus limiting the generalizability of this research. With that being said, it is important to note that the goal of a qualitative study is not to achieve generalization but to gain in-depth information from the participants’ unique perspectives. Additionally, the HCPs recruited in this study were mostly practicing in general hospitals located in urban areas. The transferability of their views to those practicing in rural or suburban settings may be limited. Since we included interprofessional HCPs in each FGD, the willingness of some participants to share their opinions regarding the topic may have been limited. Of note, we noted that nurses were the least spoken participants.
Although social desirability bias may have been present, we believe that this bias was somewhat minimal since the participants provided a balanced view consisting of both benefits and limitations of the EMs. Additionally, although the inclusion of multidisciplinary FGDs can be considered a strength as it could provide comprehensive perspectives of HCPs from different fields, it is also a weakness due to the unequal representation of HCPs in the FGDs. Also, the purposive sampling can result in self-selection that may potentially lead to overrepresentation of HCPs who are more interested in FRIDs or EMs, which can introduce bias.
CONCLUSION
This qualitative, exploratory study provides valuable insights into the opinions of geriatricians, pharmacists, and nurses on various aspects of EMs on FRIDs. The HCPs acknowledged that, in general, the awareness of OP of medications as a risk factor for falls is low. The idea of EMs on FRIDs was generally accepted by the HCPs, and they anticipated that the EMs might provide benefits to both the HCPs and OP. The HCPs suggested several topics to be included in the EMs with the main aims of enhancing OP’s knowledge and awareness of FRIDs and promoting HCP–patients communication about the drugs. Major concerns regarding the EMs include the concern of inciting fear among OP as a result of exposing them to information regarding FRIDs and the possible underutilization of the EMs.
CONFLICT OF INTEREST
The authors declare no potential conflicts of interest in conducting this research.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All the authors are eligible to be an author as per the international committee of medical journal editors (ICMJE) requirements/guidelines.
ETHICAL APPROVALS
This study was approved by the Research Ethics Committee of Universiti Teknologi MARA, Malaysia [REC/01/2021 (MR/34)].
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
FUNDING
The study was funded by the Ministry of Science, Technology and Innovation, Malaysia, under the Fundamental Research Grant Scheme (FRGS/1/2019/SS09/UITM/03/2).
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
Alex D, Khor HM, Chin AV, Hairi NN, Othman S, Khoo SPK, Kamaruzzaman SB, Tan MP. Cross-sectional analysis of ethnic differences in fall prevalence in urban dwellers aged 55 years and over in the Malaysian Elders Longitudinal Research study. BMJ Open, 2018; 8(7):e019579. CrossRef
Ambrose AF, Paul G, Hausdorff JM. Risk factors for falls among older adults: a review of the literature. Maturitas, 2013; 75(1):51–61. CrossRef
Andrade I, Silva C, Martins AC. Application of the health literacy INDEX on the development of a manual for prevention of falls for older adults. Patient Educ Couns, 2017; 100(1):154–9. CrossRef
Ascione FJ, Kirscht JP, Shimp LA. An assessment of different components of patient medication knowledge. Med Care, 1986; 24(11):1018–28. CrossRef
Atkins L, Francis J, Islam R, O’Connor D, Patey A, Ivers N, Foy R, Duncan EM, Colquhoun H, Grimshaw JM, Lawton R, Michie S. A guide to using the Theoretical Domains Framework of behaviour change to investigate implementation problems. Implement Sci, 2017; 12(1):1–18. CrossRef
Barat I, Andreasen F, Damsgaard E. Drug therapy in the elderly: what doctors believe and patients actually do. Br J Clin Pharm, 2001; 51(6):615–22. CrossRef
Bell HT, Steinsbekk A, Granas AG. Elderly users of fall-risk-increasing drug perceptions of fall risk and the relation to their drug use—a qualitative study. Scand J Prim Health Care, 2017; 35(3):247–55. CrossRef
Berg RL, Cassells JS. Falls in older persons: risk factors and prevention. The second fifty years: promoting health and preventing disability. National Academies Press, Washington, DC, 1992.
Beunza-Sola M, Hidalgo-Ovejero ÁM, Martí-Ayerdi J, Sánchez-Hernández JG, Menéndez-García M, García-Mata S. Study of fall risk-increasing drugs in elderly patients before and after a bone fracture. Postgrad Med J, 2018; 94(1108):76–80. CrossRef
Chan FWK, Wong FYY, So WY, Kung K, Wong CKM. How much do elders with chronic conditions know about their medications? BMC Geriatr, 2013; 13(1):1–7. CrossRef
Chen LL, Tangiisuran B, Shafie AA, Hassal MAA. Evaluation of potentially inappropriate medications among older residents of Malaysian nursing homes. Int J Clin Pharm, 2012; 34(4):596–603. CrossRef
Clayton LH. TEMPtEd: development and psychometric properties of a tool to evaluate material used in patient education. J Adv Nurs, 2009; 65(10):2229–38. CrossRef
Cordeiro LI, Lopes TO, Lira LEA, Feitoza SMS, Bessa MEP, Pereira MLD, Feitoza AR, Souza AR. Validation of educational booklet for HIV/Aids prevention in older adults. Rev Bras Enferm, 2017; 70(4):775–82. CrossRef
Falls, 2021. Available via https://www.who.int/news-room/fact-sheets/detail/falls#:~:text=A%20fall%20is%20defined%20as,though%20most%20are%20non%2Dfatal (Accessed 16 December 2021).
Fuller GF. Falls in the elderly. Am Fam Physician, 2000; 61(7):2159–68.
Gale CR, Westbury LD, Cooper C, Dennison EM. Risk factors for incident falls in older men and women: The English longitudinal study of ageing. BMC Geriatr, 2018; 18(1):1–9. CrossRef
Ghazi HF, Elnajeh M, Abdalqader MA, Baobaid MF, Rosli NSR, Syahiman N. The prevalence of falls and its associated factors among elderly living in old folks home in Kuala Lumpur, Malaysia. Int J Community Med Public Health, 2017; 4(10):3524–9. CrossRef
Hami R, Hassan MHM, Kadir AA, Ismail HC, Bachok N. Prevalence of geriatric giants among older people in Kelantan Malaysia. Mal J Med Health Sci, 2019; 15(2):16–21.
Hennink MM, Kaiser BN, Weber MB. What influences saturation? Estimating sample sizes in focus group research. Qual Health Res, 2019; 29(10):1483–96. CrossRef
Huang AR, Mallet L, Rochefort CM, Eguale T, Buckeridge DL, Tamblyn R. Medication-related falls in the elderly. Drugs Aging, 2012; 29(5):359–76. CrossRef
Ibrahim A, Singh DKA, Shahar S, Omar MA. Timed up and go test combined with self-rated multifactorial questionnaire on falls risk and sociodemographic factors predicts falls among community-dwelling older adults better than the timed up and go test on its own. J Multidiscip Healthc, 2017; 10:409–16. CrossRef
Kim K, Hyunjoo K, Eunmi S, Kim HS. Development of the Booklet ″Prevention and Management of Hypertension for Older Adults″. J Commun Nutr, 2004; 6(1):26–34.
Kioh SH, Rashid A. The prevalence and the risk of falls among institutionalised elderly in Penang, Malaysia. Med J Malaysia, 2018; 73(4):212–9.
Kitzinger J. Qualitative research: introducing focus groups. BMJ, 1995; 311(7000):299–302. CrossRef
Krueger RA. Analyzing focus group interviews. J Wound Ostomy Continence Nurs, 2006; 33(5):478–81. CrossRef
Laing SS, Silver IF, York S, Phelan EA. Fall prevention knowledge, attitude, and practices of community stakeholders and older adults. J Aging Res, 2011; 2011:1–9. CrossRef
Leonetti G, Lee J. Awareness of medication-related fall risk: a survey of community-dwelling older adults. Healthy Aging Res, 2014; 3(10):1–7.
Liew NY, Chong Y, Yeow SH, Kua KP, San Saw P, Lee SWH. Prevalence of potentially inappropriate medications among geriatric residents in nursing care homes in Malaysia: a cross-sectional study. Int J Clin Pharm, 2019; 41(4):895–902. CrossRef
Loke MY, Yen Gan LL, Islahudin F. Awareness of medication related falls and preferred interventions among the elderly. Pak J Pharm Sci, 2018; 31(2):359–64.
Martin P, Tamblyn R, Ahmed S, Tannenbaum C. A drug education tool developed for older adults changes knowledge, beliefs and risk perceptions about inappropriate benzodiazepine prescriptions in the elderly. Patient Edu Couns, 2013; 92(1):81–7. CrossRef
Marvin V, Ward E, Poots AJ, Heard K, Rajagopalan A, Jubraj B. Deprescribing medicines in the acute setting to reduce the risk of falls. Eur J Hosp Pharm, 2017; 24(1):10–5. CrossRef
Mazlan AZ, Omar M, Mhd-Ali A, Makmor-Bakry M. Identification of medications that increase fall risk among residents in residential aged care facilities in Klang Valley, Malaysia. Sains Malays, 2021; 50(4):1057–63. CrossRef
Milos V, Bondesson Å, Magnusson M, Jakobsson U, Westerlund T, Midlöv P. Fall risk-increasing drugs and falls: a cross-sectional study among elderly patients in primary care. BMC Geriatrics, 2014; 14(1):1–7. CrossRef
Modig S, Kristensson J, Ekwall AK, Hallberg IR, Midlöv P. Frail elderly patients in primary care—their medication knowledge and beliefs about prescribed medicines. Eur J Clin Pharmacol, 2009; 65(2):151–5. CrossRef
Newcomer KE, Hatry HP, Wholey JS. Handbook of practical program evaluation. John Wiley & Sons, Hoboken, NJ, 2015.
Osterberg L, Blaschke T. Adherence to medication. N Engl J Med, 2005; 353(5):487–97. CrossRef
Papaioannou A, Kennedy CC, Dolovich L, Lau E, Adachi JD. Patient adherence to osteoporosis medications. Drugs Aging, 2007; 24(1):37–55. CrossRef
Parekh N, Ali K, Davies K, Rajkumar C. Can supporting health literacy reduce medication-related harm in older adults? Ther Adv Drugs Saf, 2018; 9(3):167–70. CrossRef
Pasina L, Brucato A, Falcone C, Cucchi E, Bresciani A, Sottocorno M, Taddei GC, Casati M, Franchi C, Djade C, Nobili A. Medication non-adherence among elderly patients newly discharged and receiving polypharmacy. Drugs Aging, 2014; 31(4):283–9. CrossRef
Pfortmueller C, Lindner G, Exadaktylos A. Reducing fall risk in the elderly: Risk factors and fall prevention, a systematic review. Minerva Med, 2014; 105(4):275–81.
Sahril N, Shahein NA, Yoep N, Mahmud NA, Sooryanarayana R, Maw Pin T, Muhammad NA, Ismail H. Prevalence and factors associated with falls among older persons in Malaysia. Geriatr Gerontol Int, 2020; 20:33–7. CrossRef
Seppala LJ, van der Velde N, Masud T, Blain H, Petrovic M, van der Cammen TJ, Szczerbinska K, Hartikainen S, Kenny RA, Ryg J, Eklud P, Topinkova E, Mair A, Laflamme L, Thaler H, Bahat G, Gutierrez-Valencia M, Caballero-Mora M, Landi F, Emmelot-Vonk MH, Cherubini, A, O’Mahony D, Parekh N, Pisa FE, Rajkumar C Wehling M, Ziere G. EuGMS task and finish group on fall-risk-increasing drugs (FRIDs): position on knowledge dissemination, management, and future research. Eur Geriatr Med, 2019; 10(2):275–83. CrossRef
Seppala LJ, van de Glind EM, Daams JG, Ploegmakers KJ, de Vries M, Wermelink A. M, van der Velde N. Fall-risk-increasing drugs: a systematic review and meta-analysis: III. Others. J Am Med Dir Assoc, 2018; 19(4):372. CrossRef
Siqueira FV, Facchini LA, da Silveira DS, Piccini RX, Tomasi E, Thumé E, Silva SM, Dilélio A. Prevalence of falls in elderly in Brazil: a countrywide analysis. Cad Saúde Pública, 2011; 27(9):1819–26. CrossRef
Sjöberg C, Bladh L, Klintberg L, Mellström D, Ohlsson C, Wallerstedt SM. Treatment with fall-risk-increasing and fracture-preventing drugs before and after a hip fracture. Drugs Aging, 2010; 27(8):653–61. CrossRef
Susilowati IH, Nugraha S, Sabarinah S, Peltzer K, Pengpid S, Hasiholan BP. Prevalence and risk factors associated with falls among community-dwelling and institutionalized older adults in Indonesia. Malays Fam Physician, 2020; 15(1):30–8.
Tong A, Sainsbury P, Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int J Qual in Health Care, 2007; 19(6):349–57. CrossRef
van Grunsven P. The magnitude of fear of adverse effects as a reason for nonparticipation in drug treatment: a short review. J Asthma, 2001; 38(2): 113-119. CrossRef
Wahab MSA. The relevance of educating doctors, pharmacists and older patients about potentially inappropriate medications. Int J Clin Pharm, 2015; 37(6):971–4. CrossRef
Wien CA, Koleba T, Jones CA, Feeny DF. The falls risk awareness questionnaire: development and validation for use with older adults. J Gerontol Nurs, 2006; 32(8):43–50. CrossRef
Yahya HM, Suzana S, Singh DK. Development and evaluation of a booklet on nutrition education for falls prevention among older adults. Malays J Health Sci, 2020; 18(2):9–17. CrossRef