INTRODUCTION
The novel coronavirus (COVID-19) causes a disease which mainly impairs the respiratory system of a human being (Paules et al., 2020; Wu and McGoogan, 2020). The disease was officially named COVID-19 by the World Health Organization (WHO, 2020a). In the beginning, the spread was confined to nearby neighboring countries of China with confirmed cases reported in Japan, Thailand, and South Korea till January 20, 2020. An initial report by the WHO (2020b) declared 282 confirmed cases of COVID-19 in China and in its neighborhood. The infection continued to rise and spread to other parts of the globe, and the WHO named it an international public health crisis on January 30, 2020, and the situation turned grimmer on March 11, 2020, when COVID-19 was declared a pandemic (WHO Director General, 2020). The disease proliferated fast, and according to the WHO (2020b) reports, the disease had shown its presence in around 213 countries and territories with more than 14 million confirmed COVID-19 cases and over 1 million deaths worldwide. COVID-19 due to its lethal nature has paralyzed the healthcare system of not only developing countries but also developed countries. However, the situation is outrageous for countries with fragile healthcare systems (Hayat et al., 2020).
At that time, there was no defined treatment/cure for the COVID-19 disease, and it was being managed symptomatically (Hayat et al., 2020). Proper management to control the epidemic is basically comprised of the enforcement of isolation, quarantine, and physical distancing. Numerous countries have adopted variable measures to cease the rapid spread of disease, but all the efforts to control the epidemic seemed to be in vain. An efficient vaccine against COVID-19 was urgently required to cut the load of mortality and morbidity associated with the COVID-19 infection (Zhu et al., 2020). Regarding the desperate need for vaccination, there were 150 countries indulged in the race to produce a vaccine, and a few entered phase 2 clinical trials (WHO, 2020c; Zhu et al., 2020). Some proceeded to phase 3 clinical trials (Salzberg, 2020). The success of the vaccine relies on the people’s acceptability of immunization. In the past, even though the effective and safe vaccine was available, the acceptability among the population was low due to various factors (Bödeker et al., 2014; Donaldson et al., 2015; Mak et al., 2015). In an online survey in France, it was reported that 26% of the surveyed population were reluctant to use the vaccine against COVID-19 even if it is available (COCONEL Group, 2020).
Pakistan falls in the category of low-middle-income countries having a number of residents exceeding 197 million. It has four provinces, namely, Sindh, Punjab, Khyber Pakhtunkhwa (KPK), and Baluchistan, and three territories, including Gilgit-Baltistan, Islamabad Capital Territory and Azad Jammu, and Kashmir (Nations Online, 2020). The first two confirmed cases of COVID-19 in Pakistan were reported on February 26, 2020, which was a sign of high alert (France24, 2020). The spread was slightly slow till March 14, 2020, and there were only 31 definite cases afterward, a dramatic boom was recorded, and the number of cases rose rapidly. By August 22, 2020, the confirmed cases in Pakistan had crossed a figure of 292,173 (Government of Pakistan, 2020). Immunization for polio eradication in Pakistan has already proven to be a challenge. There are only two countries left behind in the war against polio: Pakistan and Afghanistan (Dawn, 2020). The Pakistani government is taking the utmost measures to eliminate polio from Pakistan, but there are hurdles in the immunization process (Kabir and Afzal, 2016). The most significant ones are less acceptability by the parents due to spiritual beliefs and safety concerns (Hussain et al., 2016; Khan and Ahmad, 2015). Recently a study conducted in Malaysia has used the health belief model (HBM) to predict the acceptability of a new vaccine and to estimate the factors hindering vaccine acceptance (Wong et al., 2020), but more and more data is needed to estimate the success of vaccination and willingness to pay (WTP) that will decide the amount the public is going to pay for the vaccine. As the development of the vaccine is in the pipeline but its success depends on the people’s behaviors of acceptance, checking the acceptability of the potential COVID-19 vaccine is needed. Thus, this study was designed to evaluate the public’s acceptance of the vaccine using the HBM.
MATERIALS AND METHODS
Study setting
An online study was conducted from July 1, 2020, to July 30, 2020, targeting multiple cities, villages (in close vicinity to the cities) from three provinces (Punjab, Sindh, and KPK). We preferred online platforms to collect the data after considering the fact that, in Pakistan, 76 million people have Internet access and 37 million people are actively using various social media platforms (Anjum, 2020), but due to low response rate and time limitation, we decided to conduct paper-based data collection from four cities of three provinces: Bahawalpur and Lahore from Punjab, Karachi from Sindh, and Peshawar from KPK. The paper-based data were collected from August 1 to August 30. The selection of these cities was due to the convenience of the data collectors. However, the fourth province could not be targeted due to the lack of data collectors there.
Study design and questionnaire
A quantitative, cross-sectional study was conducted using a modified version of a published questionnaire (Wong et al., 2020). Before using the tool, we conducted an online and paper-based pilot study, and changes were made accordingly. Also, a few partial changes and adjustments were made in accordance with the real scenario of Pakistan. The questionnaire was developed according to the HBM theory. The HBM was developed in the 1950s by social psychologists in the United States Public Health Service to predict and explain the acceptance of preventative measures such as vaccines (Anjum, 2020; Janz and Becker, 1984). This theory is one of the most frequently used in health behavior research (Carpenter, 2010). In our study, the HBM theory assessed the acceptability of the COVID-19 vaccine for the following aspects: perceived susceptibility and severity, which was collectively called the perceived threat of the COVID-19 infection, perceived barriers, perceived benefits, belief, and self-efficacy. WTP is an approach to estimate the maximum amount that an individual is willing to allocate for vaccination, services, and health technologies. The decision to receive a vaccination depends on the willingness of the society to pay for increased health benefits (Wong et al., 2020).
Demographics, including occupation, age, educational level, and household income, were collected in the first part of the data collection tool. Then, one question assessed knowledge about COVID-19, one recorded the response on testing for COVID-19, and one accumulated the data of the testing results. Eighteen questions were presented to explore the knowledge, attitudes, and beliefs toward the COVID-19 vaccine, and each measurement scale was reported using a five-point Likert scale. We asked the respondents to make a choice between the following responses: “strongly agree,” “agree” (combined and scored 1), “unsure,” “disagree,” and “strongly disagree” (combined and scored 0). The expected price for a COVID-19 vaccine to the respondents was also measured. The outcome was considered positive if the participant said that they “probably would get” or “definitely would get” the COVID-19 vaccine once it has been approved.
Sampling and study procedures
The convenience sampling method was used for collecting data. Data collection was done both electronically and in paper-based format. Online data were collected by making an online questionnaire on Google Form. The link was copied and shared on multiple social media platforms like email, WeChat, WhatsApp, and Facebook. The participants were able to answer all the questions by simply clicking on the link. The individuals were requested to fill out the questionnaire and share the link to as many as possible. The questionnaire took 5–7 minutes to complete, and all the data collected by the questionnaire was put into an electronic database. Paper-based data were collected with the help of trained data collectors from different cities of Pakistan. Interviews were conducted in different regions of the cities targeting houses from different geographical locations. The selection of the respondents was made based on the lottery method which was used in previous research studies (Gillani et al., 2018, 2021). A brief introduction of the study was mentioned at the beginning of the online data page and paper. The interviewer further explained the objective to the interviewee briefly. Participants over 18 years old currently living in Pakistan were included in this study.
Training of data collectors
Six data collectors were designated to collect data simultaneously in three different provinces. A team of two data collectors collected data from each city in different provinces while the team in Punjab were assigned two cities. They were mostly comprised of the local pharmacy students. Prior training was given which involved the following aspects: (1) presenting a brief introduction of the study purpose to respondents, (2) selecting the candidate by employing the lottery method, (3) conducting face-to-face interviews, and (4) coping with respondents’ lack of cooperation or other difficulties during the interview. The training was carried out for three days, with a demonstration given by the primary researcher. The trainees then conducted a pilot study in each of their respective districts and were observed for their interviewing skills.
Statistical analysis
Descriptive data were presented as percentages (frequencies). Fisher’s exact and the chi-squared tests were used to compare categorical variables where a p value of ≤0.05 was considered statistically significant. All the psychological consciousness items were compared with the outcomes (“would definitely” or “would probably” get the COVID-19 vaccine). The data analysis was performed using Statistical Package for the Social Sciences (SPSS) version 18.0 (SPSS Inc., Chicago, IL).
Ethical approval
This study was approved by the Ethics Committee for Medical Research of Xi’an Jiaotong University (Ethical Approval no. COV2020) and the Research Ethics Committee of the Pharmacy Department of the Superior University Lahore (PHR-73/20). Participation in this study was voluntary, prior verbal approval was obtained from the participants, and all the respondents were made aware of their right to leave the study at any time in the ethical approval statement. No personal identifying information was collected, and participants were asked to sign the paper-based questionnaire, and in the case of the online survey, the participants were advised to start it only after reading the statement.
RESULTS
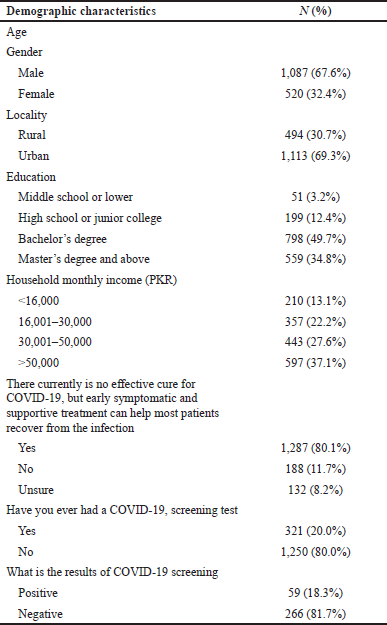
In total, 1,607 individuals participated (including both paper-based and online). The response rate for the paper-based study was 85.8% (1,340/1,560). Among these, 1,087 (67.6%) were male and 1,113 participated from urban areas, 51 (3.2%) had middle school or lower education, and 798 (49.7%) had completed their bachelor’s degree. The complete demographic characteristics of the respondents are presented in Table 1.
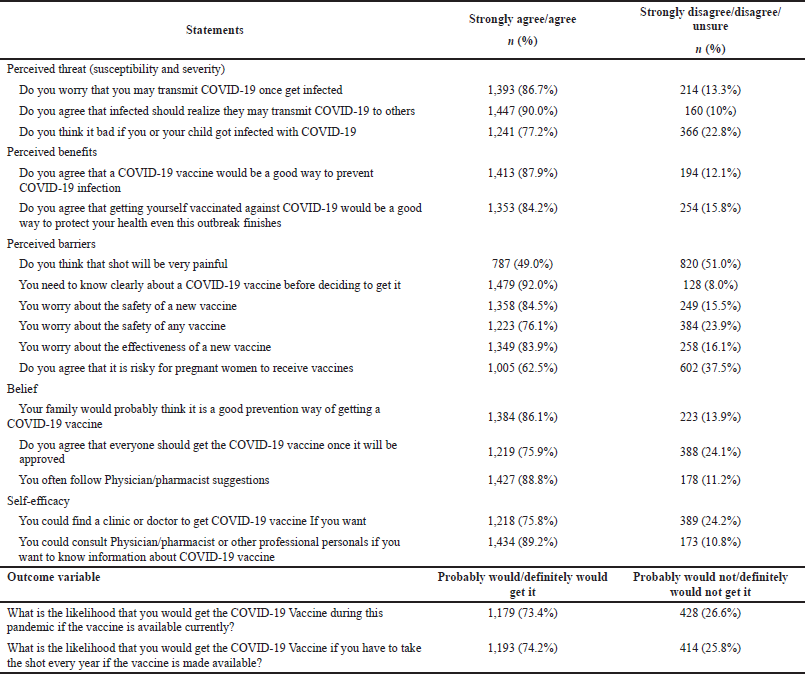
Table 2 demonstrates the attitudes of the participants toward the COVID-19 vaccine. Most of them, 1,447 (90.0%), agreed with the statement that infected people can pass the infection to others, 1,393 (86.7%) were concerned about the transmission of COVID-19, and 1,241 (77.2%) strongly agreed or agreed that it is bad for their children to become infected with the COVID-19.
About 1,413 (87.9%) of the respondents had admitted (agree or strongly agree) that vaccination is a safer way to protect their health against COVID-19, and 1,353 (84.2%) individuals said that getting vaccinated is beneficial for preventing the COVID-19 infection. Nearly half of the respondents, 787 (49.0%), thought that the vaccine would be painful, 92.0% said that they want complete information about the vaccine prior to its use, and also 84.5% of the participants confessed that they worry about the safety of the new vaccine. Almost 1,005 (62.5%) respondents felt that receiving the COVID-19 vaccine could be perilous for pregnant females. Around 979 (83.0%) persons agreed that everyone should be vaccinated once the vaccine gets approved.
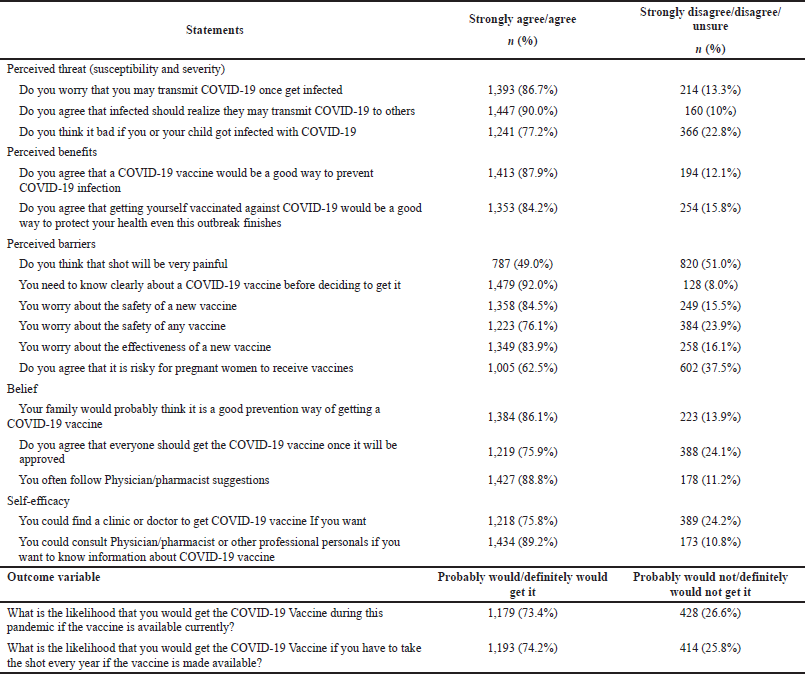 | Table 2. Percentage of respondents’ responses to the statements of the proposed constructs.
[Click here to view] |
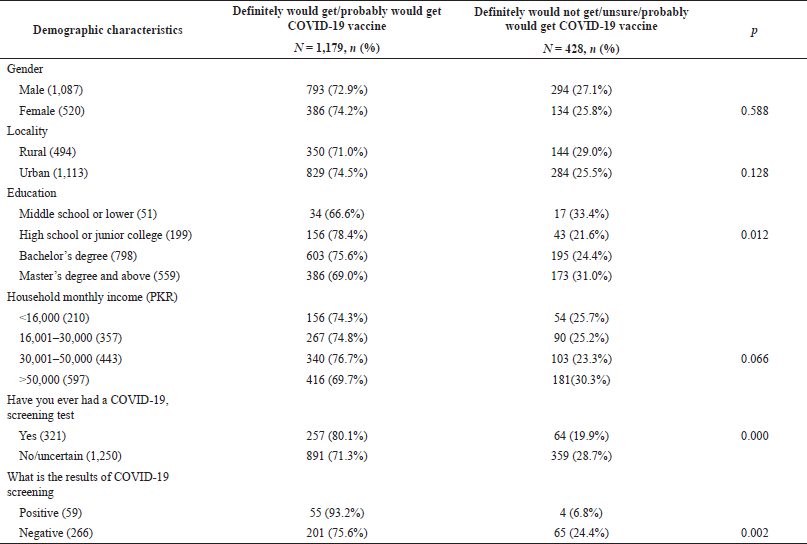
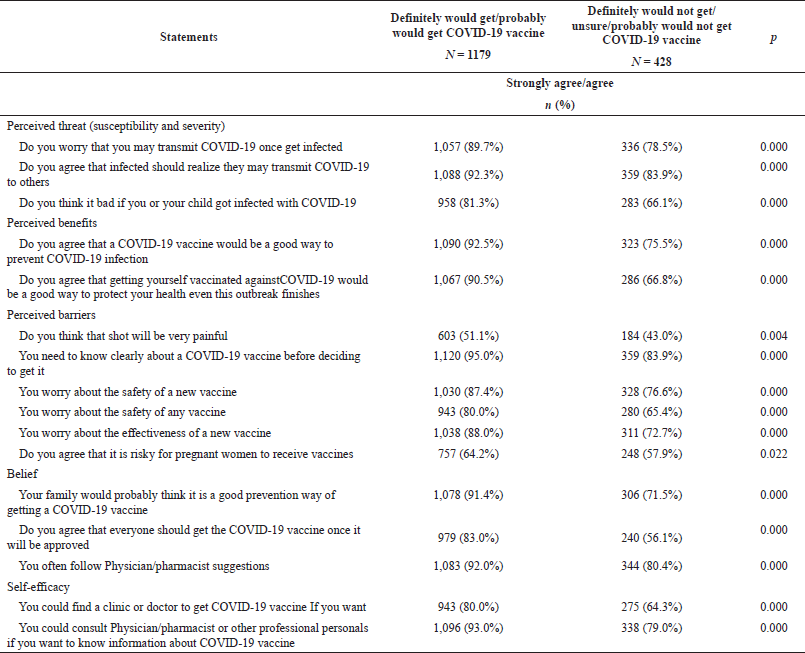
As displayed in Table 3, 1,179 (73.4%) participants of the study population said that they would (probably or definitely) get the COVID-19 vaccine. Moreover, the bivariate analysis indicated that marital status and education level were significantly associated with the outcome. Keeping the lowest score as a reference, all items including perceived threat, perceived benefits, belief, and self-efficacy were statistically and strongly associated with “probably” or “definitely” getting vaccinated in this current pandemic (Table 4).
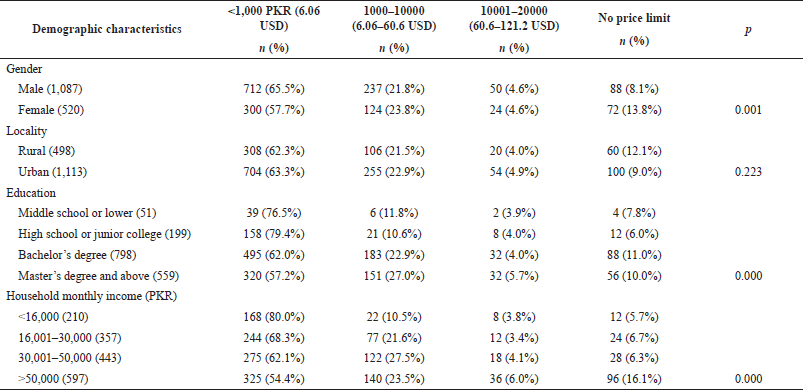
Willingness to pay
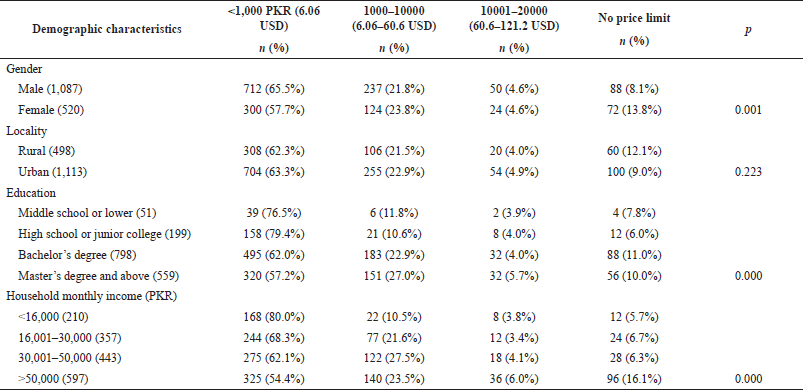
The price options ranged from the minimum amount of 1,000 Pakistani Rupees (PKR) to the maximum option of no limit for price. As shown in Table 5, all the demographic factors (except for locality) including marital status, education level, gender, and monthly household income were strongly associated with the marginal WTP for the COVID-19 vaccine, which means most of the demographic factors served as affordability barriers to the COVID-19 vaccine.
DISCUSSION
The COVID-19 vaccine is available, and its success largely relies on the people’s attitude and willingness to accept vaccination (Gillani et al., 2021). This study aims to track the public perceptions towards a COVID-19 vaccine and WTP by using the HBM in the Pakistani community. The finding of our research suggests that 26.6% of the participants would refrain from being vaccinated once the vaccine is available. Our research results are similar to the recent study in which 26% of the participants disagreed with being vaccinated in France (Donaldson et al., 2015) but not in accordance with the result in Australia in which merely 4.9% of individuals wanted to remain unvaccinated during the current pandemic (Gillani et al., 2018).
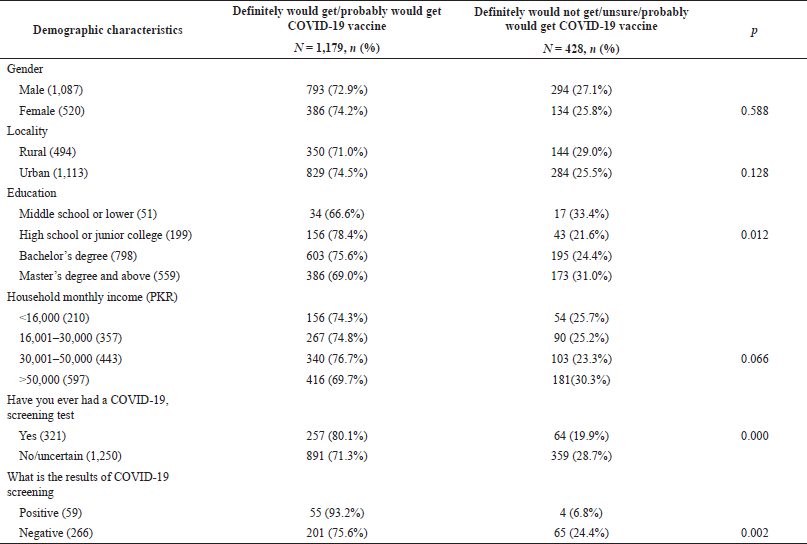 | Table 3. Bivariate associations of demographics with the outcome of “probably” or “definitely” would get the vaccine in the present pandemic.
[Click here to view] |
The reasons for the low acceptance of the COVID-19 vaccine in our current study may include the following. Firstly, only 20.0% of the total participants had the COVID-19 screening test, which means a large proportion of the sample population was unaware of the fact of whether they suffered from COVID-19. A lack of screening may impact the perception and attitude toward receiving a vaccine because the participants may consider themselves healthy and may not think it is necessary to take the vaccine. However, 86.7% were worried about the likelihood of transmission of COVID-19 if they become infected. Therefore, educating the public about COVID-19 and motivating them to get COVID-19 screening are recommendable.
One more leading reason for vaccine rejection was safety concerns. The majority of the participants (84.5%) were worried about the safety of the vaccine. Earlier, safety concerns were also observed as a barrier to polio vaccination in Pakistan (The Conversation, 2020). Polio eradication has not been successful in Pakistan because many people hold skeptical views regarding vaccine safety (The Conversation, 2020). People were also reluctant to receive the polio vaccine due to misconceptions, for example, that the polio vaccine can cause infertility (Dodd et al., 2020). The Pakistani government is working to the best of its abilities to get rid of these false perceptions about the polio vaccines, but militant organizations such as Tehreek-e-Taliban Pakistan and Al-Qaeda are a major hurdle to the eradication of polio from Pakistan. The misconception of people about the polio vaccine, insecurity within the country, and the poor health system are the reasons for the failure of polio eradication campaigns in the region (Basharat and Shaikh, 2017). This may affect COVID-19 vaccination campaigns in the future as well. Also, the media plays a role in building perceptions about the vaccination as in the Republic of Congo. Since the first case appeared, misinformation has spread across traditional media and social media, called by the WHO an infodemic. After hearing about the poor quality of the vaccine and the false information conveyed by the mass media which has included rumors on using the vaccination for the purpose of the extermination of the black race, healthcare workers may have developed vaccine hesitancy, which can influence their decisions to get vaccinated and to promote the vaccine to their patients (Khan and Sahibzada, 2016). A recent study conducted in Malaysia found that efficacy, side effects, and safety were the major perceived barriers to the COVID-19 vaccination (Hussain et al., 2016).
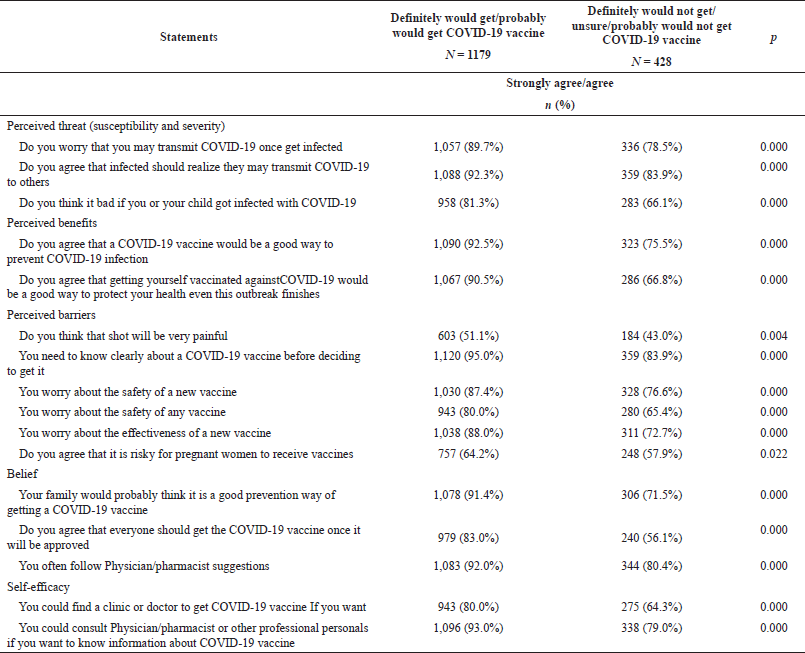 | Table 4. Bivariate associations of demographics with the outcome of “probably” or “definitely” would get the vaccine in the present pandemic.
[Click here to view] |
Additionally, religious beliefs in Muslim countries (Pakistan) also play an important role in immunization. As in our study, almost 95% of the participants stated that they would only get the vaccine if given sufficient information. Consistent with these results, a study performed in Malaysia found that more than half of the respondents were concerned about the formulation of the COVID-19 vaccine and predicted that the acceptance rate of the new vaccine could be low, which would be drastic for the future (Hussain et al., 2016). Previously, in Pakistan, the refusal of the polio vaccine was also linked to religious beliefs because many believed that the polio vaccine contained haram (prohibited in Islam) material (The Conversation, 2020). If many Pakistanis forewent receiving the COVID vaccine due to religious beliefs, then this would definitely jeopardize the health and recovery process.
Lastly, there was a strong relationship between the marginal WTP and demographic factors in our study, which means affordability barriers along with socioeconomic factors, namely, higher education levels, marital status, and higher-income groups, resulted in a lower WTP. These results of our study were dissimilar to those of the study performed in Malaysia in which no significant association between marginal WTP and socioeconomic factors was found (Hussain et al., 2016), and the same is the case with Chinese results (Shah et al., 2016; Zhang et al., 2020; The World Bank, 2020). Pakistan is a low-middle-income country (Kabamba et al., 2020), and many people cannot afford high healthcare expenditures. Therefore, incorporating the COVID-19 vaccine into the national immunization program would definitely increase the vaccine coverage, particularly in the lower-middle-income groups.
 | Table 5. Binomial association of factors associated with marginal WTP for the COVID-19 vaccine (N = 1,607).
[Click here to view] |
REFERENCES
Anjum U. Total number of active social media users in Pakistan as of 2020. 2020. Available via Phoneworld.com. pk/active-social-media-users-in-pakistan/ (Accessed 30 April 2020).
Basharat S, Shaikh BT. Polio immunization in Pakistan: ethical issues and challenges. Public Health Rev, 2017; 38:1–6. CrossRef
Bödeker B, Walter D, Reiter S, Wichmann O. Cross-sectional study on factors associated with influenza vaccine uptake and pertussis vaccination status among pregnant women in Germany. Vaccine, 2014; 32:4131–9. CrossRef
Carpenter CJ. A meta-analysis of the effectiveness of health belief model variables in predicting behavior. Health Commun, 2010; 25:661–9. CrossRef
COCONEL Group. A future vaccination campaign against COVID-19 at risk of vaccine hesitancy and politicisation. Lancet Infect Dis, 2020; 20:769–70. CrossRef
Dawn. Two more polio cases detected in Pakistan. Available via https://reliefweb.int/report/pakistan/two-more-polio-cases-detected-taking-year-s-tally41#:~:text=There%20are%20only%20two%20countries,to%20carry%20a%20vaccination%20certificate (Accessed 17 August 2020).
Dodd RH, Cvejic E, Bonner C, Pickles K, McCaffery KJ, Sydney Health Literacy Lab COVID-19 group. Willingness to vaccinate against COVID-19 in Australia. Lancet Infect Dis, 2020; 21:318–9. CrossRef
Donaldson B, Jain P, Holder BS, Lindsay B, Regan L, Kampmann B. What determines uptake of pertussis vaccine in pregnancy? A cross sectional survey in an ethnically diverse population of pregnant women in London. Vaccine, 2015; 33:5822–8. CrossRef
France24. Pakistan confirms first two cases of coronavirus. 2020. Available via https://www.france24.com/en/20200226-pakistan-confirms-first-two-cases-of-coronavirus (Accessed 17 April 2020).
Gillani AH, Chang J, Aslam F, Saeed A, Shukar S, Khanum F, Jairoun A, Nicholson A, Mohamed Ibrahim MI, Fang Y. Public knowledge, attitude, and practice regarding antibiotics use in Punjab, Pakistan: a cross-sectional study. Expert Rev Anti Infect Ther, 2021; 19(3):399–411. CrossRef
Gillani AH, Amirul Islam FM, Hayat K, Atif N, Yang C, Chang J, Qu Z, Fang Y. Knowledge, attitudes and practices regarding diabetes in the general population: a cross-sectional study from Pakistan. Int J Environ Res Public Health, 2018; 15(9):1906. CrossRef
Government of Pakistan. Know about COVID-19. 2020. Available via http://covid.gov.pk/ (Accessed 22 August 2020).
Hayat K, Rosenthal M, Xu S, Arshed M, Li P, Zhai P, Desalegn GK, Fang Y. View of Pakistani residents toward coronavirus disease (COVID-19) during a rapid outbreak: a rapid online survey. Int J Environ Res Public Health, 2020; 17:3347. CrossRef
Hussain SF, Boyle P, Patel P. Eradicating polio in Pakistan: an analysis of the challenges and solutions to this security and health issue. Global Health, 2016; 12:63. CrossRef
Janz NK, Becker MH. The health belief model: a decade later. Health Educ Q, 1984; 11:1–47. CrossRef
Kabamba Nzaji M, Kabamba Ngombe L, Ngoie Mwamba G, Banza Ndala DB, Mbidi Miema J, Luhata Lungoyo C, Lora Mwimba B, Cikomola Mwana Bene A, Mukamba Musenga E. Acceptability of vaccination against COVID-19 among healthcare workers in the Democratic Republic of the Congo. Pragmat Obs Res, 2020; 11:103–9. CrossRef
Kabir M, Afzal MS. Epidemiology of polio virus infection in Pakistan and possible risk factors for its transmission. Asian Pac J Trop Med, 2016; 9:1044–7. CrossRef
Khan MU, Ahmad A. Polio vaccination in Pakistan. Lancet, 2015; 386:337. CrossRef
Khan TM, Sahibzada MU. Challenges to health workers and their opinions about parents’ refusal of oral polio vaccination in the Khyber Pakhtoon Khawa (KPK) province, Pakistan. Vaccine, 2016; 34:2074–81. CrossRef
Mak DB, Regan AK, Joyce S, Gibbs R, Effler PV. Antenatal care provider’s advice is the key determinant of influenza vaccination uptake in pregnant women. Aust N Z J Obstet Gynaecol, 2015; 55:131–7. CrossRef
Nations Online. Administrative Map of Pakistan (Islamic Republic of Pakistan). 2020. Available via https://www.nationsonline.org/oneworld/map/pakistan-administrative-map.htm (Accessed 17 July 2020).
Paules CI, Marston HD, Fauci AS. Coronavirus infections—more than just the common cold. JAMA, 2020; 323(8):707–8. CrossRef
Salzberg S. We should consider starting Covid-19 vaccinations now. Available via https://www.forbes.com/sites/stevensalzberg/2020/08/02/start-vaccinating-now/#3b0576d8cf6e (Accessed 21 July 2020).
Shah SZ, Saad M, Rahman Khattak MH, Rizwan M, Haidari A, Idrees F. Why we could not eradicate polio from Pakistan and how can we? J Ayub Med Coll Abbottabad, 2016; 28(2):423–5.
The Conversation. A majority of vaccine skeptics plan to refuse a COVID-19 vaccine, a study suggests, and that could be a big problem. 2020. Available via https://theconversation.com/a-majority-of-vaccine-skeptics-plan-to-refuse-a-covid-19-vaccine-a-study-suggests-and-that-could-be-a-big-problem-137559 (Accessed 26 July 2020).
The World Bank. Pakistan. 2020. Available via https://data.worldbank.org/country/pakistan (Accessed 22 July 2020).
WHO. Naming the coronavirus disease. 2020a. Available via https://www.who.int/emergencies/diseases/novel-coronavirus-2019/technical-guidance/naming-the-coronavirus-disease-(covid-2019)-and-the-virus-that-causes-it (Accessed 21 August 2020).
WHO. Novel coronavirus situation report-181. 2020b. Available via https://www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (Accessed 19 July 2020).
WHO. More than 150 countries engaged in COVID-19 vaccine global access facility. 2020c. Available via https://www.who.int/news-room/detail/15-07-2020-more-than-150-countries-engaged-in-covid-19-vaccine-global-access-facility (Accessed 21 July 2020).
WHO Director General. Media briefing 11 March 2020 Covid-19 a pandemic. Available via https://www.who.int/dg/speeches/detail/who-director-general-s-opening-remarks-at-the-media-briefing-on-covid-19---11-march-2020 (Accessed 22 March 2020).
Wong LP, Alias H, Wong PF, Lee HY, AbuBakar S. The use of the health belief model to assess predictors of intent to receive the COVID-19 vaccine and willingness to pay. Hum Vaccin Immunother, 2020; 16(9):2204–14. CrossRef
Wu Z, McGoogan JM. Characteristics of and important lessons from the coronavirus disease 2019 (COVID-19) outbreak in China: summary of a report of 72?314 cases from the Chinese Center for Disease Control and Prevention. JAMA, 2020; 323:1239–42. CrossRef
Zhang Y, Luo X, Ma ZF. Willingness of the general population to accept and pay for COVID-19 vaccination during the early stages of COVID-19 pandemic: a nationally representative survey in mainland China. Hum Vaccin Immunother, 2020; 17:1622–7. CrossRef
Zhu FC, Li YH, Guan XH. Safety, tolerability, and immunogenicity of a recombinant adenovirus type-5 vectored COVID-19 vaccine: a dose-escalation, open-label, non-randomised, first-in-human trial. Lancet, 2020; 395:1845–54. CrossRef