INTRODUCTION
General including the costs of care
There has been a growing number of patients with diabetes, including type 2 diabetes (T2DM), in Bangladesh in recent years, which has increased morbidity, mortality and health related costs (Afroz et al., 2019a). Fottrell et al. (2018) found that the combined prevalence of impaired glucose tolerance and fasting glucose levels, as well as diabetes among adults in rural Bangladesh, was 26.1% and 34.9% among men and women, respectively, and prevalence rates in both genders increased with age. Among the elderly in Bangladesh, it was estimated that nearly 60% of those surveyed had at least one non-communicable disease including diabetes, with just under one-quarter had multiple co-morbidities (Mistry et al., 2021). Overall, it is estimated by Afroz et al. (2019a) that the number of patients with diabetes in Bangladesh will increase to 13.7 million by 2045 (Afroz et al., 2019a), which may well be an under-estimate given appreciable under-diagnosis of patients with diabetes in Southeast Asia including Bangladesh exacerbated by the recent COVID-19 pandemic (Kluge et al., 2020; Mistry et al., 2021; Shariful Islam et al., 2017). More recently, the International Diabetes Federation stated that there were already 13.1 million adults with diabetes in Bangladesh in 2021, with the number of people with diabetes in South East Asia expected to rise by 69% between 2021 and 2045 (IDF, 2021). This will equate to 22.3 million people in Bangladesh with diabetes by 2045 unless addressed, resulting in Bangladesh having the seventh highest prevalence rate for diabetes globally by then (IDF, 2021).
Alongside this, there are concerns with current management of patients with T2DM in Bangladesh in terms of a general lack of facilities and equipment to manage them (Rawal et al., 2019). There are also concerns with high rates of misdiagnosis, exacerbated by a lack of facilities in Bangladesh (Shariful Islam et al., 2017). Access to specialist diabetes services is also currently hindered in Bangladesh by time considerations including distances to travel to available clinics as well as often crowded conditions in clinics once patients arrive adding to the time taken to be seen. There are also concerns with associated costs of care with high co-payment levels in Bangladesh (Jennings et al., 2021). Alongside this, while locally available services are more accessible, they currently lack appropriate infrastructure as well as expertise to comprehensively manage patients (Jennings et al., 2021). Overall, even in specialist clinics in Bangladesh, there can be high rates of uncontrolled T2DM, especially among females and those with lower levels of education (Akter et al., 2019). These combined factors are a concern with high rates of complications seen among patients with T2DM, especially if uncontrolled (Afroz et al., 2019a, 2019b, 2019c; Akhter et al., 2013). Afroz et al. (2019c) in their study found prevalence rates of 10.1% and 30.5% for strokes and coronary artery disease, respectively, among patients with T2DM in Bangladesh, and 12.0%, 34.2%, 25.1%, and 5.8% of for diabetic foot alterations, nephropathy, retinopathy, and neuropathy, respectively.
These high complication rates increase the costs of care (Afroz et al., 2019b; Chan et al., 2021), which is important in Bangladesh due to high rates of patient co-payments (Haque et al., 2021a, 2021b; Khan et al., 2017; Rahman et al., 2020). Shariful Islam et al. (2017) estimated that in Bangladesh the total annual per capita expenditure on medical care was 6.1 times higher for patients with diabetes versus those without diabetes. The costs of medicines contribute most to the overall costs of treating patients with diabetes in Bangladesh (60.7%) followed by hospitalization costs (27.7%) (Afroz et al., 2019a). This can be an issue for patients as there are no national insurance programs in Bangladesh unlike among European and other countries providing universal healthcare, or discounted prices for medicines to treat diabetes mellitus and associated complications (Afroz et al., 2019a; Hamid et al., 2021). As a result, marginalized communities may struggle to fund their medication as well as pay to see a physician (Jennings et al., 2021).
However, greater proactivity in managing these patients in Bangladesh, enhanced by ongoing activities by the Government of Bangladesh, should bring considerable improvement in patient outcomes alongside net economic benefits given the current high costs of managing these patients (Afroz et al., 2019a). There are concerns though with the extent of monitoring and data routinely collected in public clinics in Bangladesh to adequately monitor patients with T2DM to reduce the extent of complications (Rawal et al., 2019).
Current management
The management of patients with diabetes in Bangladesh is increasingly orchestrated by the Diabetic Association of Bangladesh (BADAS), which was established in 1956. BADAS arranges diabetic healthcare via a number of establishments throughout Bangladesh incorporating a number of organizations. These include the Bangladesh Institute of Research and Rehabilitation in Diabetes, Endocrine and Metabolic Disorders, the National Health Care Network, Bangladesh University of Health Sciences, and the Health Care Development Projects as well as an appreciable number of affiliated associations in almost all the districts throughout Bangladesh alongside a few sub-districts (Azad, 2015; Khan et al., 2015). These organizations are typically heavily funded by the Government but operate as private organizations (Banglapedia, 2021). In addition, diabetic patients attending public hospitals do receive medicines, including traditional insulins, free of charge so long as supplies exists; however, this does not include long-acting insulin analogues (Godman et al., 2021a, 2021b; Haque et al., 2021b).
However, there are concerns with the routine availability of medicines to treat patients with diabetes, as well as routine laboratory and reporting systems, among clinics in Bangladesh (Biswas et al., 2018). These issues and concerns have been exacerbated by the instigation of lockdown and other measures to help control the spread of COVID-19, which impacts on the running of clinics as well as regular access and availability of medicines (Ahmed et al., 2020; Haque et al., 2020; Kluge et al., 2020; Mistry et al., 2021). Changes in lifestyles and diet through lockdown and other measures, coupled with reduced ability to visit clinics and pharmacies, have resulted in the worsening of glycemic values and outcomes in patients with T2DM (Eberle and Stichling, 2021; Hartmann-Boyce et al., 2020; Mohseni et al., 2021; Tewari et al., 2021). This though is not always the case with some studies showing no change in HbA1c levels or body weight pre- and post-lockdown (Sankar et al., 2020). To address concerns with patient management in Bangladesh, BADAS has published guidelines on aspects of care for patients with diabetes during the pandemic, including lifestyle advice (Diabetic Association of Bangladesh, 2020).
Study aims
In view of the current controversies and concerns, we sought to ascertain what data is routinely collected among patients with T2DM attending ambulatory clinics within public hospitals in Bangladesh. Secondly what impact, if any, did the COVID-19 pandemic have on the management of these patients building on published studies.
Most published studies regarding the management of patients with T2DM in Bangladesh have been prospective studies, including interview-based studies, rather than retrospective studies (Afroz et al., 2019b, 2019c; Rahman et al., 2020; Rawal et al., 2019; Shariful Islam et al., 2017). Consequently, such studies may not always fully capture the extent of care currently being provided to patients with T2DM attending public clinics in Bangladesh. These concerns are exacerbated by patients attending public clinics usually carrying their notes, including investigation reports, with them rather than these being stored, including electronically, within hospitals (Akter et al., 2021). Alongside this, COVID-19 itself may increase the potential for patients to develop T2DM (Maestre-Muñiz et al., 2021; Steenblock et al., 2021). Physicians may also only record advice, including lifestyle and dietary advice, if the patient is not complying. As a result, there could be concerns if patients see different physicians on different occasions and key activities are not recorded.
We were particularly interested in public hospitals due to high patient co-payment levels in Bangladesh (Khan et al., 2017; Rahman et al., 2020). Having said this, there is growing prescribing of long-acting insulin analogues in patients with diabetes in Bangladesh attending both public and private hospitals unlike the situation among patients in Africa attending public clinics (Godman et al., 2021a, 2021c; Haque et al., 2021a). This has been helped in Bangladesh by increased prescribing of lower cost long-acting insulin biosimilars, with increased competition helping to lower prices (Haque et al., 2021b).
The findings from this pilot study can subsequently be used to suggest improvements in the monitoring of patients with T2DM within public hospitals in Bangladesh to improve future care. In addition, potentially help with suggestions to improve the care of patients with T2DM among similar low- and middle-income countries (LMICs) with high co-payment levels.
MATERIALS AND METHODS
This was a retrospective pilot study of patients attending the outpatient clinic at Department of Endocrinology, Chittagong Medical College, Bangladesh. Chittagong Medical College is seen as a representative tertiary care hospital among the leading public hospitals in Bangladesh. This study builds on an earlier study in Chittagong documenting high prevalence rates of uncontrolled diabetes among those attending outpatient clinics (Akter et al., 2019).
A case report form (CRF) was developed to assess the level of clinical data usually captured during out-patient visits as well as any subsequent impact of COVID-19 lockdown measures on key outcome measures. Key measures include HbA1c, fasting plasma glucose (FPG), postprandial blood glucose (PPG), lipid levels (total cholesterol, HDL, LDL, and triglycerides), BP, serum creatinine, and urinary albumin as well as medicines prescribed for treating T2DM including insulins. In addition, the extent of micro- and macrovascular complications and other relevant complications including thyroid disorders. The final content of the CRF was based on the knowledge of the co-authors combined with published papers including a previous study conducted in Chittagong Medical College (Afroz et al., 2019c; Akter et al., 2019; Health Improvement Scotland, 2017; Mwita et al., 2019; Park and Pastakia, 2018). There was no contact with patients to clarify certain aspects of care including ongoing dietary and lifestyle changes incorporating exercise levels.
Current values of key parameters were also assessed against published targets (Table 1) to evaluate the level of care provided and the impact. Table 1 also contains details of the extent of complications and other key measures contained in the CRFs for this pilot study as well as any target levels where pertinent.
Just the names of the medicines prescribed for managing patients with T2DM, including those for complications incorporating cardiovascular medicines and statins, were recorded for this pilot study. There was no documentation of actual doses as this was outside the objectives of the study. There was also no recording whether the patients had any other co-morbidities in addition to the targeted comorbidities (Table 1).
The retrospective data collection started in December 2019, i.e., before the current COVID-19 pandemic and associated lockdown activities in Bangladesh (Godman et al., 2020a; Haque et al., 2020), and continued at 6-monthly intervals until November 2021. A 6-monthly interval was seen as optimal to monitor changes in key clinical measures (Table 1).
A pilot study was conducted among eight patients to assess the practicality of use of the CRF, with suggestions subsequently considered for improving the CRF before a full retrospective study would be undertaken in this and other clinics in Bangladesh.
Ethical approval
Ethical approval was obtained (CMC/PG/2021/232), and all patients gave verbal informed consent before starting the study.
RESULTS
Table 2 contains the characteristics of the eight patients with T2DM taking part in the pilot study. The employment status of patients was not included as this characteristic is typically not included within the patient’s notes.
Table 3 contains details of key clinical parameters and treatments during their last visit (November 2021).
Table 4 contains a history of known complications in November 2021 building on Table 1.
Table 5 contains details of typical data sets available in the patient’s notes in the studied period in accordance with Tables 3 and 4. Data sets not recorded are left out, which was typically clinical parameters including details of glycemic control, BP, and kidney function. The rationale for the visit was also variably recorded.
DISCUSSION
There was variable control of blood glucose levels among the eight patients with T2DM in November 2021 as measured by HbA1c, FPG, and PPG levels (Table 3). None of the eight patients had their PPG levels within target levels. Similarly, six out of seven patients had their FPG levels outside target levels (Table 1), and in one patient FPG levels were not recorded (Table 3). HbA1c levels was also above target levels in the majority of studied patients (Tables 1 and 3). This is similar to the findings of Akter et al.(2019) where 72% of studied patients with T2DM did not reach target HbA1c levels (Akter et al., 2019), and Afroz et al. (2019a) where 62.0% of patients with T2DM in their study had poor control and only 18.2% good control as measured by HbA1c levels. In addition, similar to concerns with increasing blood glucose levels among patients with T2DM as a result of the pandemic (Eberle and Stichling, 2021; Tewari et al., 2021). In a separate study, Afroz et al. (2019c) found key factors associated with complications of T2DM included being female, older, having a low level of education, living in an urban area, having poor dietary habits and poor adherence to prescribed treatments, physical inactivity and a longer duration of diabetes. There appeared though to be better control of BP, lipid levels, and urinary albumin levels among the eight studied patients (Table 3). However, there was no recording of lipid levels in the notes of an appreciable number of patients.
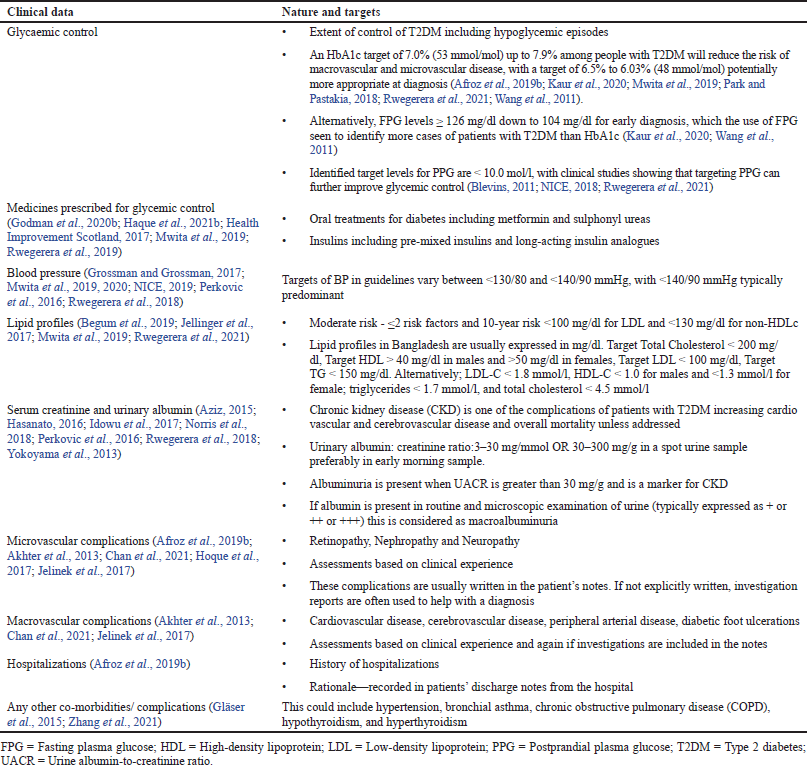 | Table 1. Key clinical data sets included in the CRFs and potential targets. [Click here to view] |
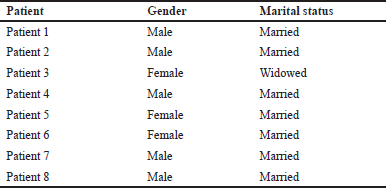 | Table 2. Key patient characteristics among the eight patients. [Click here to view] |
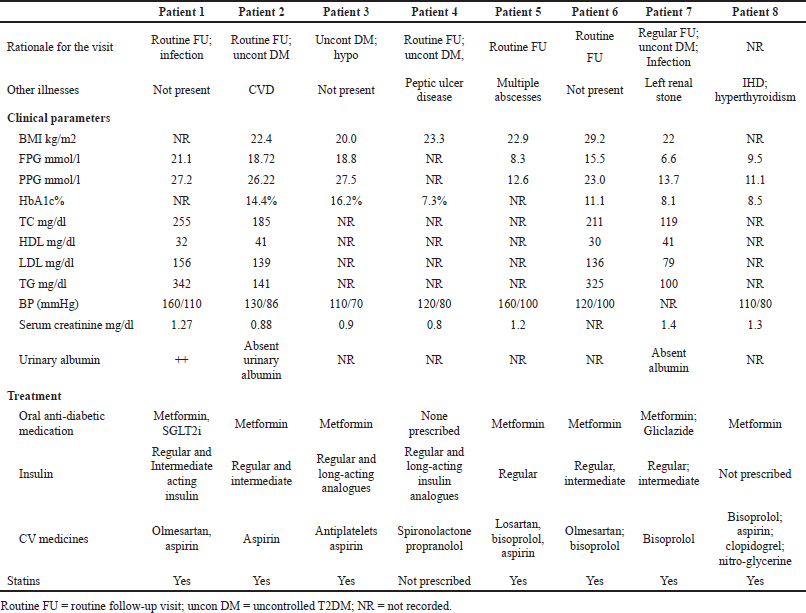 | Table 3. Key clinical parameters and treatments among the eight patients in November 2021. [Click here to view] |
Not surprisingly in view of concerns with blood glucose levels, there was increased prescribing of insulin in the majority of the studied patients alongside the prescribing of a sensitizer such as metformin. In addition, the routine prescribing of cardiovascular medicines including statins (Table 3) to help reduce the extent of macrovascular complications. Encouragingly as well, there appeared to be greater availability and prescribing of medicines to help control blood glucose levels as well as prevent cardiovascular complications compared with the situation in many other LMICs (Flood et al., 2021; Manne-Goehler et al., 2019; Mwita et al., 2020).
Despite this, microvascular and macrovascular complications did develop in a number of the studied patients (Table 4) although this was not always recorded. This is a concern given the costs associated with such complications, adding to the overall costs of managing patients with diabetes in Bangladesh (Afroz et al., 2019a; Chan et al., 2021; Moucheraud et al., 2019; Shariful Islam et al., 2017), and should be the target for future quality improvement programs. Key target areas include increasing the percentage of patients reaching target blood glucose and other targets (Table 1) to prevent subsequent complications. However, this will require changes in the way data is routinely collected in public hospitals in Bangladesh given current concerns (Table 3–5) to reduce diabetes related complications (Chamnan, 2021; Manne-Goehler et al., 2019). In addition, the development of country specific guidelines with regular updates, cognizant of the situation within a country, especially with issues of availability and affordability of medicines as well as pharmacogenetic issues as seen in the case of managing hypertension in certain groups of people (Jellinger et al., 2017; Mbui et al., 2017; Owolabi et al., 2018). There are also concerns regarding the dissemination, publication of regular updates, and follow-up of adherence to guidelines among physicians treating patients with T2DM in Bangladesh, with adherence to guidelines known to improve the quality of care provided (Campbell et al., 2021; Niaz et al., 2019; Owolabi et al., 2018). This needs to be addressed going forward.
It did appear as if the current COVID-19 pandemic interfered with out-patient clinics as seen by large gaps in patient follow-up, which needs to be improved going forward (Table 3 and 5). This is starting to be addressed as seen by the increase in patient data being collected in November 2021 versus previous studied periods following the start of the pandemic (Table 3). The instigation of electronic data sets is one way forward, building on the situation in other countries (Kerkenbush and Lasome, 2003; Kaufman, 2010). In the meantime, re-looking at the current situation to improve patient monitoring and adherence to prescribed medicines including those to prevent cardiovascular diseases and lifestyle advice (Godman et al., 2020b). This could include greater use of mobile technologies to improve the education of patients with T2DM, establishing digital support groups, as well as routine collection of key clinical parameters when clinic visits are a concern (Ranscombe, 2020).
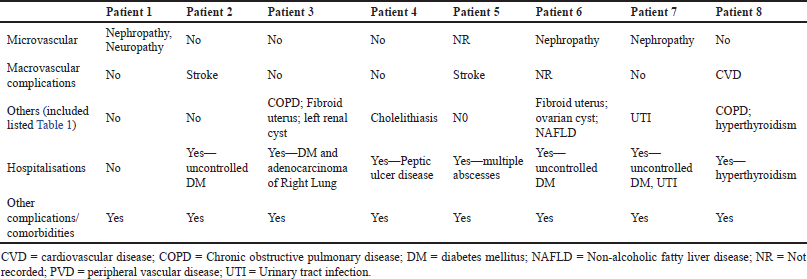 | Table 4. Noted complications in November 2021 among the eight patients. [Click here to view] |
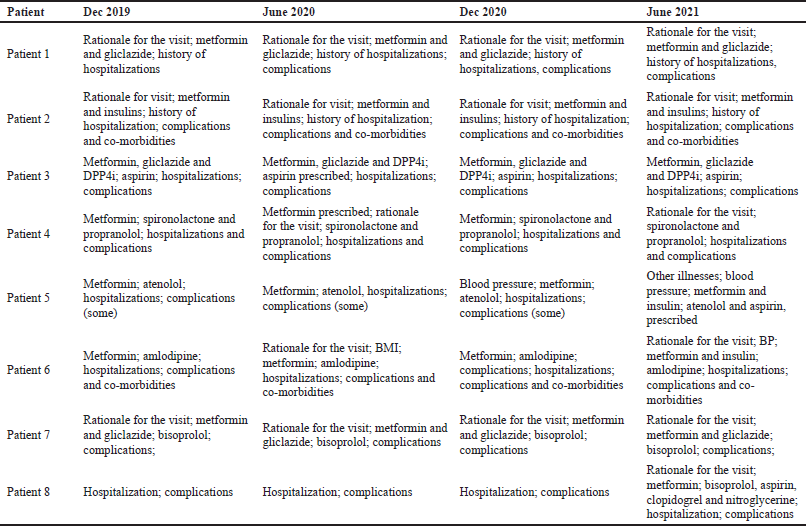 | Table 5. Key data actually recorded and available to track patient care December 2019 to June 2021. [Click here to view] |
We are aware of developments such as continuous glucose monitoring and the use of insulin pumps to further improve the care of patients with T2DM (Edelman et al., 2018; Janapala et al., 2019; Mardare et al., 2021; Wright and Hirsch, 2017). However, there are issues with affordability across LMICs (Mardare et al., 2021). In the meantime, the focus in LMICs should be on improving the care of patients with T2DM to reduce the potential for insulin in the first place as well as macrovascular complications (Godman et al., 2021c). This includes re-looking at issues such as data collection and analysis through electronic systems.
We are aware of a number of limitations with this study. This includes the fact that this is only a pilot study. In addition, it is a retrospective study subject to the typical data collection limitations of retrospective studies. Nevertheless, we believe our findings give guidance regarding potential ways to improve the care of patients with T2DM in the public health system in Bangladesh, and we will be taking this forward in future studies.
CONCLUSION
There are concerns with the management of patients with T2DM in Bangladesh; however, the outcomes of care of patients with T2DM in this pilot study appear to be better compared with a number of LMICs. However, there is considerable room for improvement to reduce future complications, including both microvascular and macrovascular complications. Improved data collection and monitoring of patients can improve the future care of patients with T2DM in the public system in Bangladesh and reduce subsequent complications in a cost-effective way. Enhancing the availability of clinics and services, including earlier diagnosis, in the public system should help to further improve the care of patients with T2DM in Bangladesh. This should be a priority, especially as we are celebrating 100 years of insulin discovery.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
FUNDING
There was no funding for this study or the write up of the study.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to the content of the paper including conception, acquisition and interpretation of the data, critically reviewing successive drafts; agreed to submit to the current journal and approving the version to be published. In addtion, FA, MH and BG were accountable for all aspects of the work. All the authors are eligible to be an author as per the international committee of medical journal editors (ICMJE) requirements/guidelines.
ETHICAL APPROVALS
Ethical approval was obtained (CMC/PG/2021/232), and all patients gave verbal informed consent before starting the study.
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
Afroz A, Alam K, Ali L, Karim A, Alramadan MJ, Habib SH, Magliano DJ, Billah B. Type 2 diabetes mellitus in Bangladesh: a prevalence based cost-of-illness study. BMC Health Serv Res, 2019a; 19(1):601; doi:10.1186/s12913-019-4440-3 CrossRef
Afroz A, Alam K, Hossain Mn, Biswas A, Ali L, Magliano Dj, Billah B. Burden of macro- and micro-vascular complications of type 2 diabetes in Bangladesh. Diabetes Metab Syndr, 2019b; 13:1615–22; doi:10.1016/j.dsx.2019.03.001 CrossRef
Afroz A, Zhang W, Wei Loh AJ, Jie Lee DX, Billah B. Macro- and micro-vascular complications and their determinants among people with type 2 diabetes in Bangladesh. Diabetes Metab Syndr, 2019c; 13(5):2939–46; doi:10.1016/j.dsx.2019.07.046 CrossRef
Ahmed SAKS, Ajisola M, Azeem K, Bakibinga P, Chen YF, Choudhury NN, Fayehun O, Griffiths F, Harris B, Kibe P, Lilford RJ, Omigbodun A, Rizvi N, Sartori J, Smith S, Watson SI, Wilson R, Yeboah G, Aujla N, Azam SI, Diggle PJ, Gill P, Iqbal R, Kabaria C, Kisia L, Kyobutungi C, Madan JJ, Mberu B, Mohamed SF, Nazish A, Odubanjo O, Osuh ME, Owoaje E, Oyebode O, Porto de Albuquerque J, Rahman O, Tabani K, Taiwo OJ, Tregonning G, Uthman OA, Yusuf R, Improving Health in Slums Collaborative. Impact of the societal response to COVID-19 on access to healthcare for non-COVID-19 health issues in slum communities of Bangladesh, Kenya, Nigeria and Pakistan: results of pre-COVID and COVID-19 lockdown stakeholder engagements. BMJ Glob Health, 2020; 5(8):e003042; doi:10.1136/bmjgh-2020-003042 CrossRef
Akhter A, Fatema K, Ahmed SF, Afroz A, Ali L, Hussain A. Prevalence and associated risk indicators of retinopathy in a rural Bangladeshi population with and without diabetes. Ophthalmic Epidemiol, 2013; 20:220–7; doi:10.3109/09286586.2013.8097704 CrossRef
Akter F, Alam SMMU, Hasan M, Rana M, Chowdhury NA, Karim M, Mannan A. The prevalence of uncontrolled type 2 diabetus mellitus and its associated factors among people within southern part of Bangladesh. JCMCTA, 2019; 30(2):92–8.
Akter F, Haque M, Kalemeera F, Kurdi A, Godman B. Key issues surrounding the management of non-communicable diseases including the management of diabetes post COVID-19 among developing countries with a specific focus on Bangladesh. J Appl Pharm Sci, 2021; 11(10):i–vi; doi:10.7324/JAPS.2021.11012ed
Azad K. Type 1 diabetes: the Bangladesh perspective. Indian J Endocrinol Metab, 2015; 19:S9–11; doi:10.4103/2230-8210.155344 CrossRef
Aziz KM. Correlation of urine biomarkers: microalbuminuria and spot urine protein among diabetic patients. Application of spot urine protein in diabetic kidney disease, nephropathy, proteinuria estimation, diagnosing and monitoring. Recent Pat Endocr Metab Immune Drug Discov, 2015; 9:121–33; doi:10.2174/1872214809666150708111022 CrossRef
Banglapedia. Banglapedia. 2021. Available via https://en.banglapedia.org/index.php/BIRDEM (Accessed 5 January 2022).
Begum A, Irfan SR, Hoque MR, Habib SH, Parvin S, Malek R, Akhter S, Sattar S, Sarkar S. Relationship between HbA1c and lipid profile seen in Bangladeshi type 2 diabetes mellitus patients attending BIRDEM hospital: a cross-sectional study. Mymensingh Med J, 2019; 28:91–5. CrossRef
Biswas T, Haider MM, Das Gupta R, Uddin J. Assessing the readiness of health facilities for diabetes and cardiovascular services in Bangladesh: a cross-sectional survey. BMJ Open, 2018; 8:e022817; doi:10.1136/bmjopen-2018-022817 CrossRef
Blevins T. Control of postprandial glucose levels with insulin in type 2 diabetes. Postgrad Med, 2011; 123:135–47; doi:10.3810/pgm.2011.07.2313 CrossRef
Campbell S, Meyer JC, Godman B. Why compliance to national prescribing guidelines is important especially across sub-Saharan Africa and suggestions for the future. J Biomed Pharm Sci, 2021; 4(6):1–7.
Chamnan P. Achieving sensible targets for a diabetes care cascade in LMICs. Lancet Glob Health, 2021; 9:e1481–2; doi:10.1016/S2214-109X(21)00403-4 CrossRef
Chan JCN, Lim LL, Wareham NJ, Shaw JE, Orchard TJ, Zhang P, Lau ESH, Eliasson B, Kong APS, Ezzati M, Aguilar-Salinas CA, McGill M, Levitt NS, Ning G, So WY, Adams J, Bracco P, Forouhi NG, Gregory GA, Guo J, Hua X, Klatman EL, Magliano DJ, Ng BP, Ogilvie D, Panter J, Pavkov M, Shao H, Unwin N, White M, Wou C, Ma RCW, Schmidt MI, Ramachandran A, Seino Y, Bennett PH, Oldenburg B, Gagliardino JJ, Luk AOY, Clarke PM, Ogle GD, Davies MJ, Holman RR, Gregg EW. The Lancet Commission on diabetes: using data to transform diabetes care and patient lives. Lancet, 2021; 396(10267):2019–82; doi:10.1016/S0140-6736(20)32374-6 CrossRef
Diabetic Association of Bangladesh. COVID-19 and diabetes—BADAS guide for healthcare professionals. 2020. Available via https://drive.google.com/file/d/1F2hHB1IMjeX-KHcyHYnvHuqYzoj00Xnj/view (Accessed 5 January 2022).
Eberle C, Stichling S. Impact of COVID-19 lockdown on glycemic control in patients with type 1 and type 2 diabetes mellitus: a systematic review. Diabetol Metab Syndr, 2021; 13(1):95; doi:10.1186/s13098-021-00705-9 CrossRef
Edelman SV, Argento NB, Pettus J, Hirsch IB. Clinical implications of real-time and intermittently scanned continuous glucose monitoring. Diabetes Care, 2018; 41:2265–74; doi:10.2337/dc18-1150 CrossRef
Flood D, Seiglie JA, Dunn M, Tschida S, Theilmann M, Marcus ME, Brian G, Norov B, Mayige MT, Gurung MS, Aryal KK, Labadarios D, Dorobantu M, Silver BK, Bovet P, Jorgensen JMA, Guwatudde D, Houehanou C, Andall-Brereton G, Quesnel-Crooks S, Sturua L, Farzadfar F, Moghaddam SS, Atun R, Vollmer S, Bärnighausen TW, Davies JI, Wexler DJ, Geldsetzer P, Rohloff P, Ramírez-Zea M, Heisler M, Manne-Goehler J. The state of diabetes treatment coverage in 55 low-income and middle-income countries: a cross-sectional study of nationally representative, individual-level data in 680,102 adults. Lancet, 2021; 2(6):E340–51; doi:10.1016/S2666-7568(21)00089-1 CrossRef
Fottrell E, Ahmed N, Shaha SK, Jennings H, Kuddus A, Morrison J, Akter K, Nahar B, Nahar T, Haghparast-Bidgoli H, Khan AKA, Costello A, Azad K. Distribution of diabetes, hypertension and non-communicable disease risk factors among adults in rural Bangladesh: a cross-sectional survey. BMJ Glob Health, 2018; 3:e000787; doi:10.1136/bmjgh-2018-000787 CrossRef
Gläser S, Krüger S, Merkel M, Bramlage P, Herth FJ. Chronic obstructive pulmonary disease and diabetes mellitus: a systematic review of the literature. Respiration, 2015; 89:253–64; doi:10.1159/000369863 CrossRef
Godman B, Haque M, Islam S, Iqbal S, Urmi UL, Kamal ZM, Shuvo SA, Rahman A, Kamal M, Haque M, Jahan I, Islam MZ, Hossain MM, Murshid ME, Kumar S, Charan J, Bhatt R, Dutta S, Abhayanand JP, Sharma Y, Saleem Z, Phuong TNT, Kwon HY, Kurdi A, Wale J, Sefah I. Rapid assessment of price instability and paucity of medicines and protection for COVID-19 Across Asia: findings and public health implications for the future. Frontiers in Public Health, 2020a; 8:585832; doi:10.3389/fpubh.2020.585832 CrossRef
Godman B, Basu D, Pillay Y, Mwita JC, Rwegerera GM, Anand Paramadhas BD, Tiroyakgosi C, Okwen PM, Niba LL, Nonvignon J, Sefah I, Oluka M, Guantai AN, Kibuule D, Kalemeera F, Mubita M, Fadare J, Ogunleye OO, Distiller LA, Rampamba EM, Wing J, Mueller D, Alfadl A, Amu AA, Matsebula Z, Kalungia A, Zaranyika T, Masuka N, Wale J, Hill R, Kurdi A, Timoney A, Campbell S, Meyer JC. Review of ongoing activities and challenges to improve the care of patients with type 2 diabetes across Africa and the implications for the future. Front Pharmacol, 2020b; 11:108; doi:10.3389/fphar.2020.00108 CrossRef
Godman B, Haque M, Leong T, Allocati E, Kumar S, Islam S, Charan J, Akter F, Kurdi A, Vassalo C, Bakar MA, Rahim SA, Sultana N, Deeba F, Khan MAH, Alam ABMM, Jahan I, Kamal ZM, Hasin H, Murshid ME, Nahar S, Haque M, Dutta S, Abhayanand JP, Kaur RJ, Rwegerera GM, do Nascimento RCRM, Dias Godói IP, Irfan M, Amu AA, Matowa P, Acolatse J, Incoom R, Sefah IA, Acharya J, Opanga S, Njeri LW, Kimonge D, Kwon HY, Bae S, Khuan KKP, Abubakar AR, Sani IH, Khan TA, Hussain S, Saleem Z, Malande OO, Piloya-Were T, Gambogi R, Hernandez Ortiz C, Alutuli L, Kalungia AC, Hoxha I, Markovi?-Pekovi? V, Tubic B, Petrova G, Tachkov K, Laius O, Harsanyi A, Inotai A, Jakupi A, Henkuzens S, Garuoliene K, Gulbinovi? J, Wladysiuk M, Rutkowski J, Mardare I, Fürst J, McTaggart S, MacBride-Stewart S, Pontes C, Zara C, Tagoe ET, Banzi R, Wale J, Jakovljevic M. The current situation regarding long-acting insulin analogues including biosimilars among African, Asian, European, and South American Countries; findings and implications for the future. Front Public Health, 2021a; 9:671961; doi:10.3389/fpubh.2021.671961 CrossRef
Godman B, Haque M, Kumar S, Islam S, Charan J, Akter F, Kurdi A, Allocati E, Bakar MA, Rahim SA, Sultana N, Deeba F, Halim Khan MA, Alam ABMM, Jahan I, Kamal ZM, Hasin H, Murshid ME, Nahar S, Haque M, Dutta S, Abhayanand JP, Kaur RJ, Acharya J, Sugahara T, Kwon HY, Bae S, Khuan KKP, Khan TA, Hussain S, Saleem Z, Pisana A, Wale J, Jakovljevic M. Current utilization patterns for long-acting insulin analogues including biosimilars among selected Asian countries and the implications for the future. Curr Med Res Opin, 2021b; 37(9):1529–45; doi:10.1080/ 03007995.2021.1946024. CrossRef
Godman B, Leong T, Abubakar AR, Kurdi A, Kalemeera F, Rwegerera GM, Patrick O, Niba LL, Ibrahim K, Amu AA, Matowa P, Acolatse J, Incoom R, Sefah IA, Opanga S, Njeri LW, Kimonge D, Oluka M, Chikowe I, Khuluza F, Phiri H, Kibuule D, Hango E, Sani IH, Malande OO, Piloya-Were T, Alutuli L, Kalungia AC, Chaibva BV, Zaranyika T, Haque M, Allocati E, Campbell S, Adwubi ET, Ogunleye OO. Availability and use of long-acting insulin analogues including their biosimilars across Africa: findings and implications. Intern Med, 2021c; 11:343.
Grossman A, Grossman E. Blood pressure control in type 2 diabetic patients. Cardiovasc Diabetol, 2017; 16(1):3; doi:10.1186/s12933-016-0485-3 CrossRef
Hamid SA, Khanam M, Azim MR, Islam MS. Health insurance for university students in Bangladesh: a novel experiment. Health Sci Rep, 2021; 4(4):e382; doi:10.1002/hsr2.382 CrossRef
Haque M, Islam S, Iqbal S, Urmi UL, Kamal ZM, Shuvo SA, Rahman A, Kamal M, Haque M, Jahan I, Islam Z, Hossain MM, Murshid ME, Sefah I, Kurdi A, Godman B. Availability and price changes of potential medicines and equipment for the prevention and treatment of COVID-19 among pharmacy and drug stores in Bangladesh; findings and implications. Bangladesh J Med Sci, 2020; 19:S36–50; doi:10.3329/bjms.v19i0.48106 CrossRef
Haque M, Islam S, Abubakar AR, Sani IH, Opanga S, Kamal ZM, Akter F, Godman B. Utilization and expenditure on long-acting insulin analogs among selected middle-income countries with high patient co-payment levels: findings and implications for the future. J Appl Pharm Sci, 2021a; 11(07):172–82; doi:10.7324/ JAPS.2021.110720
Haque M, Islam S, Kamal ZM, Akter F, Jahan I, Rahim MSA, Sultana N, Alam AM, Murshid ME, Halim-Khan MA, Deeba F, Bakar MA, Nahar S, Mozaffor M, Urmi UL, Saikat TR, Islam MZ, Haque M, Iqbal S, Hossain MM, Naher N, Allocati E, Godman B. Ongoing efforts to improve the management of patients with diabetes in Bangladesh and the implications. Hosp Pract, 2021b; 49(4):266–72; doi:10.1080/21548331.2021.1906083 CrossRef
Hartmann-Boyce J, Morris E, Goyder C, Kinton J, Perring J, Nunan D, Mahtani K, Buse JB, Del Prato S, Ji L, Roussel R, Khunti K. Diabetes and COVID-19: risks, management, and learnings from other national disasters. Diabetes Care, 2020; 43(8):1695–703; doi:10.2337/dc20-1192 CrossRef
Hasanato RM. Diagnostic efficacy of random albumin creatinine ratio for detection of micro and macro-albuminuria in type 2 diabetes mellitus. Saudi Med J, 2016; 37(3):268–73; doi:10.15537/smj.2016.3.13567 CrossRef
Health Improvement Scotland. SIGN 154—Pharmacological management of glycaemic control in people with type 2 diabetes. 2017. Available via https://www.sign.ac.uk/media/1090/sign154.pdf
Hoque S, Muttalib M, Islam MI, Happy TA. Evaluation of different HbA1c levels to assess the risk of peripheral neuropathy among type 2 diabetic patients along with other conventional risk factors. Bangladesh Med Res Counc Bull, 2017; 42(2):95e103. CrossRef
IDF. IDF diabetes atlas 2021. Available via https://diabetesatlas.org/idfawp/resource-files/2021/07/IDF_Atlas_10th_Edition_2021.pdf
Idowu AA, Ajose AO, Adedeji AT, Adegoke AO, Jimoh KA. Microalbuminuria, other markers of nephropathy and biochemical derangements in type 2 diabetes mellitus: relationships and determinants. Ghana Med J, 2017; 51(2):56–63.
Janapala RN, Jayaraj JS, Fathima N, Kashif T, Usman N, Dasari A, Jahan N, Sachmechi I. Continuous glucose monitoring versus self-monitoring of blood glucose in type 2 diabetes mellitus: a systematic review with meta-analysis. Cureus, 2019; 11(9):e5634; doi:10.7759/cureus.5634 CrossRef
Jelinek HF, Osman WM, Khandoker AH, Khalaf K, Lee S, Almahmeed W, Alsafar HS. Clinical profiles, comorbidities and complications of type 2 diabetes mellitus in patients from United Arab Emirates. BMJ Open Diabetes Res Care, 2017; 5(1):e000427; doi:10.1136/bmjdrc-2017-00042 CrossRef
Jellinger PS, Handelsman Y, Rosenblit PD, Bloomgarden ZT, Fonseca VA, Garber AJ, Grunberger G, Guerin CK, Bell DSH, Mechanick JI, Pessah-Pollack R, Wyne K, Smith D, Brinton EA, Fazio S, Davidson M. American Association of Clinical Endocrinologists and American College of Endocrinology guidelines for management of dyslipidemia and prevention of cardiovascular disease. Endocr Pract, 2017; 23(Suppl 2):1–87; doi:10.4158/EP171764.APPG CrossRef
Jennings HM, Morrison J, Akter K, Haghparast-Bidgoli H, King C, Ahmed N, Kuddus A, Shaha SK, Nahar T, Azad K, Fottrell E. Care-seeking and managing diabetes in rural Bangladesh: a mixed methods study. BMC Public Health, 2021; 21(1):1445; doi:10.1186/s12889-021-11395-3 CrossRef
Kaufman N. Internet and information technology use in treatment of diabetes. Int J Clin Pract Suppl, 2010; (166):41–6; doi:10.1111/j.1742-1241.2009.02277.x CrossRef
Kaur G, Lakshmi PVM, Rastogi A, Bhansali A, Jain S, Teerawattananon Y, Bano H, Prinja S. Diagnostic accuracy of tests for type 2 diabetes and prediabetes: a systematic review and meta-analysis. PLoS One, 2020; 15(11):e0242415; doi:10.1371/journal.pone.0242415 CrossRef
Kerkenbush NL, Lasome CE. The emerging role of electronic diaries in the management of diabetes mellitus. AACN Clin Issues, 2003; 14(3):371–8; doi:10.1097/00044067-200308000-00012 CrossRef
Khan AKA, Mahtab H, Ahmed T, Ashrafuzzaman S, Bhowmik B, Ahmed T, Afsana F, Ilondo M, Stevens D. Increasing diabetes healthcare capacity in Bangladesh through a distance learning project. J Diabetol, 2015; 6:1.
Khan JAM, Ahmed S, Evans TG. Catastrophic healthcare expenditure and poverty related to out-of-pocket payments for healthcare in Bangladesh-an estimation of financial risk protection of universal health coverage. Health Policy Plan, 2017; 32(8):1102–10; doi:10.1093/heapol/czx048. CrossRef
Kluge HHP, Wickramasinghe K, Rippin HL, Mendes R, Peters DH, Kontsevaya A, Breda J. Prevention and control of non-communicable diseases in the COVID-19 response. Lancet, 2020; 395(10238):1678–80; doi:10.1016/S0140-6736(20) 31067-9 CrossRef
Mardare I, Campbell SM, Meyer JC, Sefah IA, Massele A, Godman B. Enhancing choices regarding the administration of insulin among patients with diabetes across countries and implications for future care. Front Pharmacol, 2021. Available via https://www.frontiersin.org/articles/10.3389/fphar.2021.794363/abstract CrossRef
Maestre-Muñiz MM, Arias Á, Mata-Vázquez E, Martín-Toledano M, López-Larramona G, Ruiz-Chicote AM, Nieto-Sandoval B, Lucendo AJ. Long-term outcomes of patients with coronavirus disease 2019 at one year after hospital discharge. J Clin Med, 2021; 10(13):2945; doi:10.3390/jcm10132945 CrossRef
Manne-Goehler J, Geldsetzer P, Agoudavi K, Andall-Brereton G, Aryal KK, Bicaba BW, Bovet P, Brian G, Dorobantu M, Gathecha G, Singh Gurung M, Guwatudde D, Msaidie M, Houehanou C, Houinato D, Jorgensen JMA, Kagaruki GB, Karki KB, Labadarios D, Martins JS, Mayige MT, McClure RW, Mwalim O, Mwangi JK, Norov B, Quesnel-Crooks S, Silver BK, Sturua L, Tsabedze L, Wesseh CS, Stokes A, Marcus M, Ebert C, Davies JI, Vollmer S, Atun R, Bärnighausen TW, Jaacks LM. Health system performance for people with diabetes in 28 low- and middle-income countries: a cross-sectional study of nationally representative surveys. PLoS Med, 2019; 16(3):e1002751; doi:10.1371/journal.pmed.1002751 CrossRef
Mbui JM, Oluka MN, Guantai EM, Sinei KA, Achieng L, Baker A, Jande M, Massele A, Godman B. Prescription patterns and adequacy of blood pressure control among adult hypertensive patients in Kenya; findings and implications. Expert Rev Clin Pharmacol, 2017; 10(11):1263–71; doi:10.1080/17512433.2017.1371590 CrossRef
Mistry SK, Ali ARMM, Yadav UN, Ghimire S, Hossain MB, Das Shuvo S, Saha M, Sarwar S, Nirob MMH, Sekaran VC, Harris M. Older adults with non-communicable chronic conditions and their health care access amid COVID-19 pandemic in Bangladesh: findings from a cross-sectional study. PLoS One, 2021; 16(7):e0255534; doi:10.1371/journal.pone. 0255534 CrossRef
Mohseni M, Ahmadi S, Azami-Aghdash S, Mousavi Isfahani H, Moosavi A, Fardid M, Etemadi M, Ghazanfari F. Challenges of routine diabetes care during COVID-19 era: a systematic search and narrative review. Prim Care Diabetes, 2021; 15(6):918–22; doi:10.1016/j.pcd.2021.07.017 CrossRef
Moucheraud C, Lenz C, Latkovic M, Wirtz VJ. The costs of diabetes treatment in low- and middle-income countries: a systematic review. BMJ Glob Health, 2019; 4(1):e001258; doi:10.1136/bmjgh-2018-001258 CrossRef
Mwita JC, Francis JM, Omech B, Botsile E, Oyewo A, Mokgwathi M, Molefe-Baikai OJ, Godman B, Tshikuka JG. Glycaemic, blood pressure and low-density lipoprotein-cholesterol control among patients with diabetes mellitus in a specialised clinic in Botswana: a cross-sectional study. BMJ Open, 2019; 9(7):e026807; doi:10.1136/bmjopen-2018-026807 CrossRef
Mwita JC, Godman B, Esterhuizen TM. Statin prescription among patients with type 2 diabetes in Botswana: findings and implications. BMC Endocr Disord, 2020; 20(1):36; doi:10.1186/s12902-020-0516-7 CrossRef
Niaz Q, Godman B, Massele A, Campbell S, Kurdi A, Kagoya HR, Kibuule D. Validity of World Health Organisation prescribing indicators in Namibia’s primary healthcare: findings and implications. Int J Qual Health Care, 2019; 31(5):338–45; doi:10.1093/intqhc/mzy172 CrossRef
NICE. NICE recommended target blood glucose level ranges. 2018. Available via https://www.diabetes.co.uk/downloads/factsheets/bloodsugar.pdf (Accessed 4 January 2022).
NICE. Hypertension in adults: diagnosis and management (NG136). 2019. Available via https://www.nice.org.uk/guidance/ng136/resources/hypertension-in-adults-diagnosis-and-management-pdf-66141722710213
Norris KC, Smoyer KE, Rolland C, Van Der Vaart J, Grubb EB. Albuminuria, serum creatinine, and estimated glomerular filtration rate as predictors of cardio-renal outcomes in patients with type 2 diabetes mellitus and kidney disease: a systematic literature review. BMC Nephrol, 2018; 19(1):36; doi:10.1186/s12882-018-0821-9 CrossRef
Owolabi MO, Yaria JO, Daivadanam M, Makanjuola AI, Parker G, Oldenburg B, Vedanthan R, Norris S, Oguntoye AR, Osundina MA, Herasme O, Lakoh S, Ogunjimi LO, Abraham SE, Olowoyo P, Jenkins C, Feng W, Bayona H, Mohan S, Joshi R, Webster R, Kengne AP, Trofor A, Lotrean LM, Praveen D, Zafra-Tanaka JH, Lazo-Porras M, Bobrow K, Riddell MA, Makrilakis K, Manios Y, Ovbiagele B, COUNCIL Initiative. Gaps in guidelines for the management of diabetes in low- and middle-income versus high-income countries—a systematic review. Diabetes Care, 2018; 41(5):1097–105; doi:10.2337/dc17-1795 CrossRef
Park PH, Pastakia SD. Access to hemoglobin A1c in Rural Africa: a difficult reality with severe consequences. J Diabetes Res, 2018; 2018:6093595; doi:10.1155/2018/6093595 CrossRef
Perkovic V, Agarwal R, Fioretto P, Hemmelgarn BR, Levin A, Thomas MC, Wanner C, Kasiske BL, Wheeler DC, Groop PH, Conference Participants. Management of patients with diabetes and CKD: conclusions from a “Kidney Disease: improving Global Outcomes” (KDIGO) Controversies Conference. Kidney Int, 2016; 90(6):1175–83; doi:10.1016/j.kint.2016.09.010 CrossRef
Rahman MM, Zhang C, Swe KT, Rahman MS, Islam MR, Kamrujjaman M, Sultana P, Hassan MZ, Alam MS, Rahman MM. Disease-specific out-of-pocket healthcare expenditure in urban Bangladesh: a Bayesian analysis. PLoS One, 2020; 15(1):e0227565; doi:10.1371/journal. pone.0227565 CrossRef
Ranscombe P. How diabetes management is adapting amid the COVID-19 pandemic. Lancet Diabetes Endocrinol, 2020; 8(7):571; doi:10.1016/S2213-8587(20)30181-9 CrossRef
Rawal LB, Kanda K, Biswas T, Tanim MI, Poudel P, Renzaho AMN, Abdullah AS, Shariful Islam SM, Ahmed SM. Non-communicable disease (NCD) corners in public sector health facilities in Bangladesh: a qualitative study assessing challenges and opportunities for improving NCD services at the primary healthcare level. BMJ Open, 2019; 9(10):e029562; doi:10.1136/bmjopen-2019-029562 CrossRef
Rwegerera GM, Molefe-Baikai OJ, Masaka A, Shimwela M, Rivera YP, Oyewo TA, Godman, BB, Massele A, Habte D. Prevalence of chronic kidney disease using estimated glomerular filtration rate among diabetes patients attending a tertiary clinic in Botswana. Hosp Pract, 2018; 46(4):214–20; doi:10.1080/21548331.2018.1506674 CrossRef
Rwegerera GM, Masaka A, Pina-Rivera Y, Moshomo T, Gaenamong M, Godman B, Oyewo TA, Massele A, Habte D. Determinants of glycemic control among diabetes mellitus patients in a tertiary clinic in Gaborone, Botswana: findings and implications. Hosp Pract, 2019; 47(1):34–41; doi:10.1080/21548331.2018.1535977 CrossRef
Rwegerera GM, Shailemo DHP, Pina Rivera Y, Mokgosi KO, Bale P, Oyewo TA, Luis BD, Habte D, Godman B. Metabolic control and determinants among HIV-infected type 2 diabetes mellitus patients attending a tertiary clinic in Botswana. Diabetes Metab Syndr Obes, 2021; 14:85–97; doi:10.2147/DMSO.S28572 CrossRef
Sankar P, Ahmed WN, Mariam Koshy V, Jacob R, Sasidharan S. Effects of COVID-19 lockdown on type 2 diabetes, lifestyle and psychosocial health: a hospital-based cross-sectional survey from South India. Diabetes Metab Syndr, 2020; 14(6):1815–9; doi:10.1016/j.dsx.2020.09.005 CrossRef
Shariful Islam SM, Lechner A, Ferrari U, Laxy M, Seissler J, Brown J, Niessen LW, Holle R. Healthcare use and expenditure for diabetes in Bangladesh. BMJ Glob Health, 2017; 2(1):e000033; doi:10.1136/ bmjgh-2016-000033 CrossRef
Steenblock C, Schwarz PEH, Ludwig B, Linkermann A, Zimmet P, Kulebyakin K, Tkachuk VA, Markov AG, Lehnert H, de Angelis MH, Rietzsch H, Rodionov RN, Khunti K, Hopkins D, Birkenfeld AL, Boehm B, Holt RIG, Skyler JS, DeVries JH, Renard E, Eckel RH, Alberti KGMM, Geloneze B, Chan JC, Mbanya JC, Onyegbutulem HC, Ramachandran A, Basit A, Hassanein M, Bewick G, Spinas GA, Beuschlein F, Landgraf R, Rubino F, Mingrone G, Bornstein SR. COVID-19 and metabolic disease: mechanisms and clinical management. Lancet Diabetes Endocrinol, 2021; 9(11):786–98; doi:10.1016/S2213-8587(21)00244-8 CrossRef
Tewari A, Tewari V, Tewari J. Effect of COVID 19 lockdown on glycemic parameters in people with type 2 diabetes. J Family Med Prim Care, 2021; 10(7):2529–32; doi:10.4103/jfmpc.jfmpc_1896_20 CrossRef
Wang W, Lee ET, Howard BV, Fabsitz RR, Devereux RB, Welty TK. Fasting plasma glucose and hemoglobin A1c in identifying and predicting diabetes: the strong heart study. Diabetes Care, 2011; 34(2):363–8; doi:10.2337/dc10-1680 CrossRef
Wright LA, Hirsch IB. Metrics beyond hemoglobin A1C in diabetes management: time in range, hypoglycemia, and other parameters. Diabetes Technol Ther, 2017; 19(S2):S16–26; doi:10.1089/dia.2017.0029 CrossRef
Yokoyama H, Arakis, Honjo J, Okizaki S, Yamada D, Shudo R, Shimizu H, Sone H, Moriya T, Haneda M. Association between remission of macroalbuminuria and preservation of renal function in patients with type 2 diabetes with overt proteinuria. Diabetes Care, 2013; 36(10):3227–33; doi:10.2337/dc13-0281 CrossRef
Zhang P, Lopez R, Attaway AH, Georas SN, Khatri SB, Abi-Saleh S, Zein JG. Diabetes mellitus is associated with worse outcome in patients hospitalized for asthma. J Allergy Clin Immunol Pract, 2021; 9(4):1562–9.e1; doi:10.1016/j.jaip.2020.10.054 CrossRef