INTRODUCTION
Drug utilization study is the most important and challenging process in the geriatric population. According to the World Health Organization (WHO), drug utilization study was defined as the promotion, distribution, prescription, and utilization of medications in a community, with special emphasis on the resulting medical, societal, and financial significances (Capellà, 1993; Shalini et al., 2010; World Health Organization (WHO), 1993)
According to the UN, the definition of older persons is those people whose age is 60 years and above (World Health Organization (WHO), 2014). In 2017, the world people aged 60 years or above were 962 million, more than double and as large as that in 1980; with 382 million elderly people in the world, it is expected to increase by twofold again by 2050 and is estimated to be nearly 2.1 billion. In 2017, over two-third of the world’s elderly people lived in developing countries. Between 2017 and 2050, the number of persons aged 60 years or above in the developing world is estimated to be more than twofold, from 652 million to 1.7 billion (United Nations, 2017). The number of elderly people will be increased, which is the highest and fastest in the developing regions. Asia has the largest number of elderly people, and Africa is facing the biggest proportionate growth (United Nations, 2018).
The drug prescriber plays a serious part in identifying drug use within the community and prescribing medication for geriatric patients is a complex and challenging process. Drug prescribing has become an essential public health concern worldwide. Elderly patients have impaired pharmacokinetics and pharmacodynamics functions because of aging and there is a significant change in their physiological state. Awareness of age-associated physiological alterations, i.e., slow response time and reduced balance, will make patients and caregivers aware of the risks, make informed choices, and possibly avoid falls and adverse effects of medication. Decisions to prescribe medication are based on the aim of care, problem, and risks (Corsonello et al., 2010; Duraković and Vitezić, 2013; Jaul and Barron, 2017). The functions and composition of the human body need adjustments to drug choice and dosage because of age-related alterations of the geriatric population (Turnheim, 2003). Improving drug therapy is an important aspect for geriatric patients because the most important and common medical intervention in the elderly is drug therapy (Chung, 2014; Penge and Crome 2014). The process of prescribing medication for the geriatric population needs proper decision, so that when a drug is ordered, selecting the best medication and deciding a dosage and schedule properly for the physiologic status of elderly patients is given attention. Many drugs should be used with special care because of age-associated alterations in pharmacokinetics (i.e., absorption, distribution, metabolism, and excretion) and pharmacodynamics (the physiologic properties of the medication) (Blanda, 2006; Duraković and Vitezić, 2013).
Old age is related with increased incidence of different chronic illnesses that often lead to the use of complex drug regimens (Corsonello et al., 2010). The drug utilization study gives insight into various features of drug use and prescribing, such as a way of use, quality of usage, factors of use, and results of drug usage (Kanwal and Zaka, 2018). The skill to prescribe drugs is rationally affected by several sorts of working environment. The two main vital elements are sufficient supply of essential medicines and obtaining rational information about the medications, but without these elements it is challenging for health personnel to function successfully (World Health Organization (WHO), 1993). Essential drugs are those drugs that satisfy the priority healthcare needs of the people and are chosen with regard to disease occurrence and public health significance, proof of clinical efficiency and safety, and reasonable costs and cost-effectiveness, which are expected to be accessible within the healthcare system always in sufficient amounts, in the suitable dosage forms, with guaranteed quality, and at an expense the person or the community can buy (Bansal and Purohit, 2013). Aging presents several difficulties for the governments, the public, and elderly people themselves, which need urgent policy reactions, in addition to anticipatory policy actions to organize countries for meeting these difficulties (Dugarova, 2017).
Ethiopia has a national drug policy intended to ensure that the government shall deliver sufficient supply of drugs that are important for prevention, therapy, diagnosis, rehabilitation, and mitigation of diseases affecting the country’s population. To achieve this, Ethiopia prepared a national list of essential drug lists (EDLs) that leads the choice of all health service workers for choosing and utilizing the most required drugs at each level of the healthcare system and at all times with reasonable cost. The supply was conducted by government drug prescribers who prescribe drugs from the EDL that is available within healthcare facilities in adequate and affordable costs (Food, Medicine and Health Care Administration and Control Authority (FMHACA), 2014).
Ethical consideration
Ethical approval was obtained from Ethical Review Board of Sharda University IRB, as well as from the Ethical Clearance Committee of Addis Ababa City Administration Health Bureau’s health research and emergency management core process (HREM ERC). After approval from the ethics committee, the letter of permission was submitted to each health facility subsequently before data collection. Then, permission was obtained from the health facility’s medical director and store manager of the pharmacy department to collect data. At the time of data collection, the confidentiality of the elderly patients was maintained. All elderly patients’ related information was not released to anyone (PHREM ERC, public health research and emergency management core process).
MATERIALS AND METHODS
Cross-sectional methods of the study were used, prescribing patterns were assessed retrospectively, and prospective methods were used to evaluate the health facilities. Five healthcare facilities were randomly chosen and data were collected from April 20 to August 20, 2019. The World Health Organization recommends a drug prescribing pattern that includes those involving cross-sectional studies whenever possible and retrospective data collection over the past year should be used (World Health Organization (WHO), 1993). Patients aged ≥60 years of either sex who visited the outpatient department from July 2017 to June 2018 were included the study, involving 1,200 geriatric outpatient prescriptions/encounters who were randomly chosen from the outpatient pharmacy previously kept at every facility.
Study area
The study was conducted in the outpatient pharmacy departments of selected governmental health centers (HC) and one general hospital of Addis Ababa. Addis Ababa is the capital city of Ethiopia and lies on 9 latitudes and 38 degrees east longitude, found within the central part of Ethiopia, and covers an area of 530 km2 (53,000 ha). The total number of residents was 3,041,002 million persons (Andarge, 2016). Ethiopia’s healthcare system service is structured into a three-tier system: primary hospital, HC, and health post. The primary health care unit covers HCs and five health posts (HPs). A primary level hospital serves inpatient and outpatient services to an average people of 100,000 people; furthermore, it provides emergency surgical care and functions as a referral center for HCs under its catchment sites, which paramedical health professionals and nurses use as a practical training center. A general hospital serves inpatient and outpatient to a mean of 1,000,000 people. Medical professionals treat various kinds of illnesses. HCs gives curative, promotive, preventive, and rehabilitative ambulatory services, and have a basic laboratory and pharmacy facilities. HCs function as a referral site for HPs and provide services for 15,000–25,000 people (Mann et al., 2016).
Data collection and management
The data were collected from Ethiopia from selected health facilities by using the WHO’s drug utilization study core indicators for drug prescribing study and facility assessment core indicators for facility assessment. Necessary information was collected from the encounter and filed properly in a format, and daily the formats were checked for accuracy by two researchers who conducted the study before they were sent for analysis.
Prescriptions dispensed to geriatric outpatients were included in this study. However, the study excluded inpatient prescriptions. For this study, 1,200 geriatric patient prescriptions were randomly selected retrospectively from prescriptions written for a 1-year period during systematic random sampling. Equal proportions were taken from five outpatient pharmacy units: 200 prescriptions from each HC and 400 prescriptions from one general hospital based on patient load. The necessary data were collected by the researcher and one pharmacist from every healthcare facility. The objectives of the study, sampling procedure, and the methods to collect data from encounters using the form were explained by the principal investigator to pharmacists.
Each prescription was assessed according to the WHO’s core prescribing indicators. Prospectively, the five selected health facilities observations were carried out and assessed by core facility indicators that are accessibility of a copy of EDL formulary, standard treatment guideline (STG), reference books, international guidelines, and accessibility of key essential drugs during data collection.
The specific information required to assess the prescribing measures were recorded for every elderly patient’s prescription and entered directly into a normal prescribing indicator sheet. Based on the WHO’s drug prescribing core indicators and facility core indicators, which include the mean number of drugs per prescription, the percentage of prescriptions with generic name medications prescribed, antibiotics, injections and prescribed drugs from the EDL were calculated and the results were used to evaluate the prescribing pattern. Facility assessments were made by observing, availability of the copy of EDL, formulary, STG, reference books, international guidelines, and accessibility of key essential drugs.
The results were calculated as follows:
- The mean number of medicines prescribed per encounter was calculated as:
- Facility indicators were used to check the availability of the copy of EDL, formulary, STG, and reference books within the facility.
Data analysis
All collected data prior to analysis were cleaned and coded. By means of the Statistical Packages for Social Sciences version 20, the collected data were entered and analysis was conducted. The results were expressed as actual numbers, means, frequency, percentages, and were present using tables. The interpretations of the finding were conducted according to the standard value of the WHO’s prescribing and facility core indicators.
RESULTS AND DISCUSSION
A total of 1,200 geriatric patient prescriptions were evaluated for 4 months from April 20 to August 20, 2019, from the selected five health facilities of outpatient pharmacy. The encounters were assessed by using the WHO’s drug use study guidelines using core indicators, and 1,200 geriatric patients’ encounters were selected from the health facilities. Analysis was carried out by means of core indicators.
Patient characteristics
The mean age of the geriatric patients was 67.5 years and the age structure of the study population revealed that 363 (30.3%) patients were in the age group of 60–64 years, 358 (29.8%) were aged 65–69 years, 219 (18.3%) were aged 70–74 years, 150 (12.5%) were aged 75–79 years, 68 (5.7%) were aged 80–84 years, 33 (2.8%) were aged 85–89 years, and 9 (0.8%) were aged >90 years old. From these 1,200 patients, 535(44.6%) were male and 665(55.4%) were female (Table 1)
Evaluation by WHO’s prescribing indicators
The mean number of drugs per encounter showed as 2.67, 2.28, 2.2, 2.35, and 2.51 in Akaki Health Center (AKHC), Arada Health Center (ARHC), Shiromeda Health Centre (SMHC), Tekilhaymanot Health Centre (TKHC), and Tirunesh Beijing General Hospital (TBHL), respectively, and the encounter with the highest number of medicines had seven drugs. The percentage of medicines ordered by generic name within the five healthcare facilities was 436 (81.95%), 399 (87.69%), 373 (86.34%), 412 (87.85%), and 919 (91.62%) in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively. The percentage of prescription with antibiotics was 118 (59%), 97 (48.5%), 92 (46%), 114 (57%), and 111(27.75%) in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively. The percentage of medicines prescribed injection was 33 (16.5%), 42 (21%), 68 (34%), 40 (20%), and 65 (16.25%) in AKHC, ARHC, SMHC, TKHC and TBHL, respectively. The percentage of drugs from the Ethiopian EDL prescribed was 407 (76.5%), 399 (87.69%), 373 (86.34%), 411 (87.63%), and 918 (91.53%) in AKHC, ARHC, SMHC, TKHC and TBHL, respectively (Table 2).
.png) | Table 1. Distribution of geriatric patients by age group and sex selected in the five health facilities outpatient pharmacies in Addis Ababa, Ethiopia, 2019. [Click here to view] |
Healthcare facility assessment
At the time of data collection, a prospective survey was undertaken by observing accessibility of key essential medicines, accessibility of a copy of EDL, STGs, copy of formulary, reference books, and international guidelines of the American Society of Geriatrics 2015 BEERS criterion for drug prescribing in elderly. In our study, the finding was that 5 (100%) had a copy of the Ethiopian EDL, 4 (80%) had a copy of STG, 4 (80%) had a copy of the drug formulary, 2 (40%) had reference books, and none of the facilities had international guidelines, like the BEERS criteria used to improve drug prescribing practices for geriatric patients to decrease or prevent potential risks and complications. Our findings showed that the percentage of accessibility of key essential medicines for AKHC, ARHC, SMHC, TKHC, and TBHL were 12 (92.3%), 13 (100%), 10 (76.9%), 12 (92.3%), and 13 (100%), respectively (Table 3).
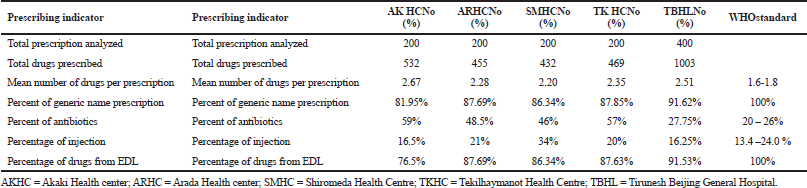 | Table 2. Drug prescribing indicators in the five outpatient department health facilities in Addis Ababa, Ethiopia, 2019. [Click here to view] |
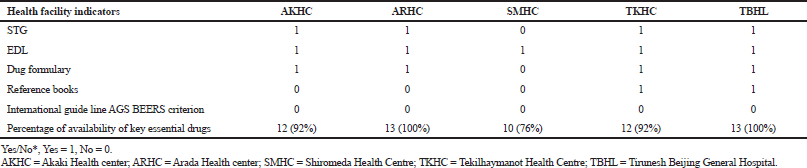 | Table 3. Healthcare facility assessment by indicators in the selected healthcare facilities of Addis Ababa, Ethiopia, 2019. [Click here to view] |
DISCUSSION
The WHO established tools for the assessment of core prescribing indicators which is used to observe the level of polypharmacy, the ability to prescribe medicines by generic name, percentage of antibiotics and injections medicines uses, and the level of prescribing practice from the essential medicine list or formulary in addition core facility indicators developed (World Health Organization (WHO), 1993).
The prescribing patterns of drugs reflect the clinical decision of the prescribers. In our study, the mean number of medicines per prescription was 2.67, 2.28, 2.2, 2.35, and 2.51 in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively, which was somewhat higher than the WHO’s standards and lesser than results from Indian and Ethiopian studies, where the mean number of medicines per encounter was 5.51 and 5.1, respectively, which show polypharmacy and is greater than our findings (Oumer, 2017; Sharma et al., 2013). In one of the assessment of geriatric patients in India, the result was 7.02 (Nandagopal et al., 2017). The encounter with the maximum number of medicines in our study had seven, whereas a similar study had a higher number (Bhaveshaikh et al., 2017).
The percentage of medicines prescribed by generic name within the five healthcare facilities was 436 (81.95%), 399 (87.69%), 373 (86.34%), 412 (87.85%), and 919 (91.62%) in AKHC, ARHC, SHHC, TKHC, and Tirunesh Beijing Hospital (TBHL), respectively. The values were larger than a study conducted in India (15, 3.25%) (Nandagopal et al., 2017). The study result of ARHC, Shiromeda Health Centre (SMHC), TKHC, and Tirunesh Beijing Hospital (TBHL) was 399 (87.69%), 373 (86.34%), 412 (87.85%), and 919 (91.62%), respectively, which is greater than the same study carried out in Ethiopia where the result was 85.7% (Oumer, 2017). Among the five health facilities, the result of AKHC 436 (81.95%) was less than the WHO’s standard, which is 100%.
The percentage of encounter with antibiotics was 118 (59%), 97 (48.5%), 92 (46%), 114 (57%), and 111 (27.75%) in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively. In all the four facilitates, the results deviate from the WHO’s standards; in general, the misuse of antibiotics is the main cause of bacterial resistance. Only TBHL (111, 27.75%) is within the normal range (Aslam et al., 2018), which fits the standard and is greater than the study in India, which was 21.6% (Abraham et al., 2015). .The finding of our study was somehow better than a study conducted in Ethiopia, which was 63.5% (Oumer, 2017) and the results in the four facilities were 118 (59%), 97 (48.5%), 92 (46%), and 114 (57%) in AKHC, ARHC, SMHC, and TBHL, respectively, which were greater than a study conducted in India, which was 128 (41.8%) (Pradhan et al., 2016). The main cause for the occurrence of antibiotics resistance is antibiotics overprescribing (Worku and Tewahido, 2018). One of the major leading causes for antimicrobial resistance is the misuse of antimicrobials either by patients or healthcare professionals (Chokshi et al., 2019; Rattanaumpawan et al., 2019). Antimicrobial resistance is a worldwide public health problem that has speeded up the overuse of antibiotics at a global level. It is the cause of severe infections, complications, extended hospital stays, and increased death rate (Llor and Bjerrum, 2019).
Prescriptions with injections ordered were 33 (16.5%), 42 (21%), 68 (34%), 40 (20%), and 65 (16.25%) in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively. The five healthcare facilities used injection drugs in a similar way mentioned in the WHO’s standard that is encouragable, except in TKHC in which 68 (34%) prescribed. However, other studies, in Saudi Arabia, reported lower than our finding, which was 28.45% (Gupta et al., 2016), on the other hand, and higher figures were reported in India, 92.57%, (Singh, 2017) in Ethiopia 355 (59.16%) (Sisay et al., 2017), and another study in India which was 220 (73.57%) (Varghese et al., 2015). The use of injection drugs has drawbacks, like sepsis, and the danger of tissue toxicity from local irritation, risk of thrombophlebitis, expensive, and unable to correct the mistake after injection; therefore, WHO’s standard was limited to less than 10% of the prescription which ought to contain 1 or more injections (Cyriac and James, 2014; World Health Organization (WHO), 1993). Many injections around the world are unnecessary and often unsafe. Unsafe injections put lives at risk and every year cause 1.67 million hepatitis B infections, up to 315,120 hepatitis C infections, and up to 33,877 human immunodeficiency virus infections (Pépin et al., 2014). In one study, the injectable usage was 0.15%, which is a very lower percent than our study (Nishandar et al., 2017).
In our study, majority of the medicines prescribed from the Ethiopian EDL were 407 (76.5%), 399 (87.69%), 373 (86.34%), 411 (87.63%), and 918 (91.53%) in AKHC, ARHC, SMHC, TKHC, and TBHL, respectively. EDL is related to the standard rate of 100%, but in other studies done in India (66.3%) (Kashyap et al., 2016) and only 35% of drugs were prescribed from the EDL (Pradhan et al., 2016).
The WHO recommended that 100% of drugs have to be prescribed by generic name; on the other hand, drug prescribing by generic name has advantages. Generic medicines are duplication of brand name medicines which have similar dosage, proposed use, effects, side effects, method of administration, risks, safety, and strength equally as brand medicine, or the pharmacological results for both are identical generic drugs are essential medicine that permit better availability to healthcare for every cases and sold with low-cost (Hague, 2017). Ordering generic medicines benefits to cost reduction since it is inexpensive options, no delay of production since the chemist can distribute a wider variety of alternate supplies, relatively than being inadequate to one that cannot be kept (Dunne et al., 2013). In Ethiopia, the drug policy encourages drug prescribers to prescribe drugs from EDL as known that all EDLs are generic drugs which are accessible the most required drugs at all level of the healthcare system any time with reasonable price as the supply to the health facilities are done by government. Those drugs are available within health facilities in adequate and affordable costs so patients can get medicines with low cost (Food, Medicine and Health Care Administration and Control Authority (FMHACA), 2014).
The result of this study revealed that 5 (100%) of healthcare facilities had a copy (EDL), 4 (80%) had a copy of STG for HC, 4 (80%) had a copy of drug formulary, 2 (40%) had reference books, and none of the facilities had international guidelines. The percentage of availability of key essential drugs for AKHC, ARHC, SMHC, TKHC, and TBHL were 12 (92.3%), 13 (100%), 10 (76.9%), 12 (92.3%), and 13 (100%), respectively. In a similar study conducted in Ethiopia among four hospitals, the results showed that only quarter of or 1 (25 %) hospital had a copy of (EDL) and 1 (25 %) had STG, and drug formulary. The availability of key medicines in hospitals was 65.7%, which is lower than the finding in our study (Gidebo et al., 2016). In our study, 2 (40% ) had reference books and none of the facilities had International guidelines, but other studies conducted in eight health facilities the results showed that only 6 (75%) of the health facilities had EDL, 7 (87.5%) had STG, and 6 (75%) had a copy of the drug formulary; however, there was no important reading resources (Nigussie, 2014). In our finding, the percentage of accessibility of key essential medicines for AKHC, ARHC, SMHHC, TKHC, and TBHL were 12 (92.3%), 13 (100%), 10 (76.9%), 12 (92.3%), and 13 (100%), respectively. In one study conducted in south India, the percentage of key drugs available was 88%, which is somewhat similar to our finding (Prasad et al., 2015). A, Similar study conducted in southwest Ethiopia in four facilities showed that only half or 50% of healthcare facilities had both EDL and STG for HC, and only one-fourth or 25% had a copy of the drug formulary, but others had no important reading resources (Angamo et al., 2011). The research done in India had no EDL available in the health facilities. Only there were three key essential drugs (20%), which is lower than our finding (Parveen et al., 2016).
CONCLUSION
The method of prescribing in relation to the generic name, prescribing drugs from EDL, and polypharmacy was near-optimal to the standard WHO requirements. However, there is a need to improve the pattern of prescribing antibiotics and injection medicines, availability of key essential medicine in stock, and availability and use of international guidelines, like AGS BEERS Criteria, which is a guide for decisions about what drugs to use in geriatric patients. The findings may give due attention to geriatric patients to prevent and control drug prescribing related to complications, polypharmacy, antibiotic resistances, disability, and unnecessary hospital admissions, which may improve accessibility of essential medicines and international guidelines in healthcare facilities of Addis Ababa, Ethiopia. Information collected by our study can be used by investigators and policymakers in the future as baseline. All health facilities assessed in this study were not aware of the use of BEERS criteria; the possible reasons include in Ethiopia drug prescribing is conducted by either physicians (GPs) or other professionals who are not specialized in geriatric medicine so that they are not aware of this guideline.
RECOMMENDATIONS
Depending on our findings the following recommendations were made:
- Establishment of geriatrics medicine curriculum and implementation to medical schools that develop and implement the basic science and clinical curriculum constituents on aging with national level and opening of residency program training in geriatrics.
- Addis Ababa Health Bureau has to prepare and provide training for drug prescribers dealing with geriatric patients to offer appropriate geriatric care.
- Distribute and follow health guidelines by distributing BEERS Criteria to the health facilities in order to decrease drug-related drawback, unnecessary hospitalization, and mortality in geriatric patients.
- Improve availability of key essential medicines in stock and the pattern of prescribing antibiotics and injection medicines,
- Availability and use of international guidelines, such as AGS BEERS Criteria, should be a guide for decisions about what drugs to use in geriatric patients.
ACKNOWLEDGMENTS
Authors would like to thank the Addis Ababa City Administration Health Bureau and staff of the health centers and hospitals for allowing us to carry out the research in their facilities.
CONFLICT OF INTEREST
Authors declared that they do not have any conflicts of interest.
FUNDING
None.
AUTHORS’ CONTRIBUTIONS
All authors made significant contributions in planning, implementing, and investigating of the study and to develop this manuscript. WL conceptualized and designed the study along with MI and VS. WL coordinated the data collection, along with EL.WL conducted the statistical analyses along with EL. WL wrote the manuscript. EL and MI reviewed the article and all authors agreed on its last version.
REFERENCES
Abraham F, Varughese G, Mathew JC, John PM, Sam GK. Drug utilization pattern among geriatric patients in a tertiary care teaching Hospital. Asian J Pharm Clin Res, 2015; 8(6):191–4.
Andarge A. Health facilities distribution mapping in Addis Ababa. Debre Markos University, Debre Markos, Ethiopia, vol. 16(3), 2016.
Angamo MT, Wabe NT, Raju NJ. Assessment of patterns of drug use by using world health organization’s prescribing, patient care, and health facility indicators in selected health facilities in southwest Ethiopia. J Appl Pharm Sci, 2011; 1(7):62–6.
Aslam B, Wang W, Arshad MI, Khurshid M, Muzammil S, Rasool MH, Baloch Z. Antibiotic resistance: a rundown of a global crisis. Infect Drug Resist, 2018; 11:1645–58. CrossRef
Bansal D, Purohit VK. Accessibility and use of essential medicines in health care: current progress and challenges in India. J Pharmacol Pharmacother, 2013; 4(1):13–8. CrossRef
Bhaveshaikh N, Sukumaran S, Vyas U. Drug prescribing patterns in elderly patients in a tertiary level hospital. Int J Basic Clin Pharmacol, 2017; 6(4):759–64. CrossRef
Blanda MP. Pharmacologic issues in geriatric emergency medicine. Emerg Med Clin North Am, 2006; 24(2):449–65. CrossRef
Capellà D. Descriptive tools and analysis. Drug utilization studies. Methods Uses, 1993; WHO Regional Publications, European Series, No. 45, 55-78. Available via http://www.euro. who.int/_data/assets/pdf_file/0011/156782/euro_series_45.pdf
Chokshi A, Sifri Z, Cennimo D, Horng H. Global contributors to antibiotic resistance. J Glob Infect Dis, 2019; 11(1):36–42. CrossRef
Chung JY. Geriatric clinical pharmacology and clinical trials in the elderly. Transl Clin Pharmacol, 2014; 22(2):64–9. CrossRef
Corsonello A, Pedone C, Incalzi, R. Age related pharmacokinetic and pharmacodynamic changes and related risk of adverse drug reactions. Curr Med Chem, 2010; 17(6):571–84. CrossRef
Cyriac JM, James E. Switch over from intravenous to oral therapy: a concise overview. J Pharmacol Pharmacother, 2014; 5(2):83–7. CrossRef
Dugarova E. Ageing, older persons and the 2030 agenda for sustainable development. United Nations Publications, New York, NY, 2017.
Dunne S, Shannon B, Dunne C, Cullen, W. A review of the differences and similarities between generic drugs and their originator counterparts, including economic benefits associated with usage of generic medicines, using Ireland as a case study. BMC Pharmacol Toxicol, 2013; 14:1–19. CrossRef
Duraković Z, Vitezić, D. Pharmacodynamics and pharmacokinetics in the elderly. Period Biol, 2013; 115(4):517–20.
Food, Medicine and Health Care Administration and Control Authority (FMHACA). National essential medicine list. 5th edition, Food, Medicine and Health Care Administration and Control Authority (FMHACA), Addis Ababa, Ethiopia, p 132, 2014. Available via http://apps.who.int/medicinedocs/documents/s22351en/s22351en.pdf
Gidebo KD, Summoro TS, Kanche ZZ, Woticha EW. Assessment of drug use patterns in terms of the WHO patient-care and facility indicators at four hospitals in Southern Ethiopia: a cross-sectional study. BMC Health Serv Res, 2016; 16(1):1–8. CrossRef
Gupta N, Safhi MM, Sumaily JMY, Nayeem M, Hussain M, Agarwal M, Siddiqui AH. A study on the prescription pattern of drugs in Jazan general hospital, KSA. Afr J Pharm Pharmacol, 2016; 10(1):7–13. CrossRef
Hague M. Generic medicine and prescribing: a quick assessment. Adv Hum Biol, 2017; 7:101–8. CrossRef
Jaul E, Barron J. Age-related diseases and clinical and public health implications for the 85 years old and over population. Front Public Health, 2017; 5:335. CrossRef
Kanwal H and Zaka M: Drug utilization pattern in geriatrics a review. Wjpps, 2018; 7(1):203–06.
Kashyap M, D’cruz S, Sachdev A, Tiwari P. Drug use patterns among Indian elderly outpatients. J Indian Acad Geriatr, 2016; 12:5–9.
Llor C, Bjerrum L. Antimicrobial resistance: risk associated with antibiotic over use and initiatives to reduce the problem. Ther Adv Drug Saf, 2019; 5(6):229–41. CrossRef
Mann C, Dessie E, Adugna M, Berman P, Chan HTH. Measuring efficiency of public health centers in Ethiopia. 2016. Available via https://cdn1.sph.harvard.edu/wp-content/uploads/sites/2031/2017/01/Health-Center-Efficiency-Analysis-Report-Ethiopia-FINAL.pdf.
Nandagopal A, Koneru A, Rahman A, Pasha K, Ali KY. Assessment of rational drug prescribing pattern in geriatric patients in Hyderabad metropolitan. Indian J Pharm Pract, 2017; 10(3):174–8. CrossRef
Nigussie WD. Assessment of the degree of adherence to health facility indicators related to rational drug use in Selected Health Facilities of Amhara Region, Northwest Ethiopia. Int J Pharmacol Sci Res, 2014; 5(04):171–8.
Nishandar TB, Kale AS, Pise HN. Drug utilization pattern in geriatric patients attending outpatient department at rural tertiary care hospital in Maharashtra. Asian J Pharmacol Clin Res, 2017; 10(2):10–2. CrossRef
Oumer S. Irrational use of medications among elderly patients in an Ethiopian referral hospital. Afr J Pharm Pharmacol, 2017; 11(15):191–4. CrossRef
Parveen Z, Gupta S, Kumar D, Hussain S. Drug utilization pattern using WHO prescribing, patient care, and health facility indicators in a primary and secondary health care facility. Natl J Physiol Pharm Pharmacol, 2016; 6(3):182–6. CrossRef
Penge J, Crome P. Appropriate prescribing in older people. Rev Clin Gerontol, 2014; 24(1):58–77. CrossRef
Pépin J, Chakra CNA, Pépin E, Nault V, Valiquette L. Evolution of the global burden of viral infections from unsafe medical injections, 2000-2010. PLoS One, 2014; 9(6):1–8. CrossRef
Pradhan S, Panda A, Panigrahy SR. Analysis of drug utilization pattern in elderly in an outpatient department using who indicators : a cross sectional study. Res J Pharm Biol Chem Sci, 2016; 7(6):2628–33.
Prasad PS, Rudra JT, Vasanthi P, Sushitha U, Sadiq MJ, Narayana G. Assessment of drug use pattern using World Health Organization core drug use indicators at Secondary Care Referral Hospital of South India. CHRISMED J Health Res, 2015; 2(3):223. CrossRef
Rattanaumpawan P, Chuenchom N, Thamlikitkul V. Perception, attitude, knowledge and learning style preference on challenges of antimicrobial resistance and antimicrobial overuse among first year doctors in training and final year medical students. Antimicrob Resist Infect Control, 2019; 8:142. CrossRef
Shalini S, Ravichandran V, Bk M, Sk D, Saraswathi R. Drug utilization studies an overview. Int J Pharm Sci Nanotechnol, 2010; 3(1):803–10. CrossRef
Sharma N, Advani U, Parakh R, Bansal, A. Screening of prescriptions in geriatric population in a tertiary care teaching hospital in north India. J Phytopharmacology, 2013; 2(5):38–45.
Singh GN. To assess the drug utilization pattern and to analyze pharmacoeconomics for geriatrics in-patient in medicine department of tertiary care teaching hospital. J Pharm Pharm Sci, 2017; 9(12):276–82. CrossRef
Sisay M, Abdela J, Kano Z, Araya M, Chemdi M, Fiseha A. Drug prescribing and dispensing practices in tertiary care hospital of eastern Ethiopia: evaluation with World Health Organization Core prescribing and patient care indicators. Clin Exp Pharmacol, 2017; 07(03):1–8. CrossRef
Turnheim, K. When drug therapy gets old: pharmacokinetics and pharmacodynamics in the elderly. Exp Gerontol, 2003; 38(8):843–53. CrossRef
United Nations. International Day of Older Persons - 1 October. 2018. Available via https://www.soroptimistinternational.org/international-day-of-older-persons-2/%0Ahttp://www.un.org/en/events/olderpersonsday/background.shtml (Accessed 10 July 2019).
United Nations. World Population Prospects revision. 2017 Available via https://population.un.org/wpp/Publications/Files/WPP2017_DataBooklet.pdf (Accessed 14 June 2019).
Varghese GH, Alexander H, Tom NR, Philip PT, Kumar TRA, Sivakumar T. Assessment of patterns of drug utilization evaluation by who prescribing indicators among special population in a tertiary care teaching hospital in Tamilnadu. IJPBS, 2015; 5(4):40–8.
Worku F, Tewahido D. Retrospective assessment of antibiotics prescribing at public primary healthcare facilities in Addis Ababa, Ethiopia. Interdiscip Perspect Infect Dis, 2018; 2018(2):1–9. CrossRef
World Health Organisation (WHO). Definition of an older or elderly person. Health statistics and information systems: definition of an older or elderly person. World Health Organization (WHO), Geneva, Switzerland, pp 17–9, 2014.
World Health Organization (WHO). How to investigate drug use in health facilities: selected health use indicators. World Health Organization (WHO), Geneva, Switzerland, 1993.