INTRODUCTION
Chronic diseases such as diabetes and hypertension are noncommunicable diseases that have a high prevalence in Indonesia. Based on the Indonesian Basic Health Data (Riskesdas) in 2018, the prevalence of diabetes increased to 10.9% from 2.1% in 2013, whereas the prevalence of hypertension increased to 34.1% from 25.8% in 2013 (Ministry of Health Republic of Indonesia, 2013; 2018). Both diabetes and hypertension can worsen the functions of other organs, such as the heart, kidneys, eyes, and nerves if not managed properly. Hypertension is a major risk factor for other cardiovascular diseases (20%–25%) (Hussain et al., 2016), and around 28% of deaths in Indonesia are caused by cardiovascular disease (WHO, 2015). Diabetes itself also has become a contributor to death, being present as a factor in 3% of all the cases of death in Indonesia (WHO, 2015).
The Chronic Disease Management Program (Prolanis) has been run by the Indonesian Health Insurance Agency since 2014, managing patients with chronic diseases such as type 2 diabetes and hypertension (BPJS Kesehatan, 2014). Treatment approaches for diabetes and hypertension aim to control the patients’ blood sugar and blood pressure. In the Prolanis program, patients receive medical consultations, education, and periodic home visits from health professionals in primary healthcare facilities. The patients in the Prolanis program are expected to achieve an optimal quality of life (QOL) and avoid the emergence of disease complications (BPJS Kesehatan, 2014). The measurement of QOL in chronic patients is important because patients with conditions such as diabetes and hypertension usually have a lower QOL score when compared with those without such diseases (Bardage and Isacson, 2001; Manjunath et al., 2014). However, to the best of our knowledge, the measurement of health outcomes related to the QOL in the Prolanis patients has never been done before.
The health-related QOL (HRQOL) has become an important indicator in assessing the outcomes of health interventions in addition to clinical outcomes (Fitzpatrick et al., 1992). HRQOL can provide information about a persons’ health condition as a whole because it considered both the physical and mental conditions and their respective impacts on the QOL (Palermo et al., 2008). HRQOL is even considered by some as the ultimate goal of health intervention (Rubin and Peyrot, 1999).
In chronic diseases, instruments that can be used to measure the QOL include both the generic and specific instruments. Specific instruments are used for a particular disease or disease condition and thus are narrower in scope, such as the pediatric QOL (PedsQol) instrument for pediatric patients and the Functional Living Index-Cancer instrument for cancer patients (Fitzpatrick et al., 1992). In comparison, generic instruments can be used in broader conditions and can be used to compare different disease conditions. One example of a generic instrument is the five-dimension EuroQol (EQ) questionnaire created by the EuroQol group, which has been deployed through translation in many countries around the world (EuroQol Goup, 2017). The advantage of this questionnaire is that it only has five questions and is easily understood by respondents. The EQ instrument has two versions: the three-level EQ-5D (EQ-5D-3L) and the five-level EQ-5D (EQ-5D-5L). Both the EQ5D3L and EQ5D5L questionnaires have been translated into Indonesian. However, the questionnaire that has a value set in the population currently in Indonesia is the EQ-5D-5L (Purba et al., 2017). The previous research efforts to measure HRQOL in Indonesia have used the value sets from Malaysia, Thailand, or Singapore, which is a less ideal scenario (Endarti et al., 2015; Kristina et al., 2015; Purba et al., 2017; Setiawan et al., 2018).
HRQOL measurement in the Prolanis patients using the EQ-5D instrument would be very useful, providing important information and helping to conduct an economic evaluation for purposes such as a cost–utility analysis. The research output could also be used to compare the results of the Prolanis patients with other disease outcomes or those of similar patients not in the management disease program and may push health professionals conducting Prolanis to improve their services. Therefore, this study aimed to evaluate HRQOL in Prolanis patients in Purwokerto, Indonesia, using the EQ-5D-5L instrument.
METHODS
Study design and participants
A descriptive, cross-sectional study design was used to assess the HRQOL of the Prolanis patients. Patients who were registered in the Prolanis program at six community health centers in Purwokerto Regency, Indonesia, from April to June 2018 were included in this study; those who did not complete the questionnaire were excluded from the final analysis.
The community health centers represented the primary care locations where the Prolanis program has taken place, with a total population of 394 diabetic patients and 723 hypertensive patients. We calculated the minimum sample size using a 95% confidence level and a 5% accepted margin of error, determining a minimum sample size for diabetes of 195 and that for hypertension of 252. A convenient sampling was performed in the study setting. All patients participated in this survey signed the information and consent forms. An ethical approval was acquired from the Medical and Health Research Ethics Committee, Faculty of Medicine, Gadjah Mada University, Indonesia (reference no. KE/FK/0294/EC/2018).
Data collection and analysis
Face-to-face interviews were conducted to obtain the HRQOL data and patient characteristics. The collected patient characteristics included age, gender, education level, employment status, diagnosis, and duration of illness. HRQOL was evaluated using the Indonesian version of the EQ-5D-5L instrument. The Indonesian version of the EQ-5D-5L instrument was obtained through the EuroQol Group (2017). The EQ-5D-5L translation was obtained through a structured translation procedure (Rabin et al., 2014) and has been demonstrated from previous studies as a valid and reliable questionnaire for use in Indonesia (Purba et al., 2018; Setiawan et al., 2018). This instrument consists of two parts: the EQ descriptive system and the EQ visual analog scale (EQ-VAS). The utility (EQ-5D-5L index score) value was calculated by Indonesia’s value set (Purba et al., 2017). The utility values generally range from zero points (death) to one point (perfect health). The utility value is calculated by subtracting the perfect health status (one point) with the value of disutility due to illness and treatment (utility = 1 − disutility).
A descriptive analysis was used to depict the patient characteristics and HRQOL with regard to utility scores, VAS, and patients’ responses in each dimension. Rubin and Peyrot (1999) indicated that demographic and socioeconomic data might affect the EQ-5D score. Therefore, a statistical analysis was performed to identify the differences in the study characteristics as well as variations in the EQ-5D utility index between diabetes and hypertension. The normality test using the Kolmogorov–Smirnov approach revealed that all parameters were not normally distributed (p = 0.001), so a nonparametric test was implemented. The Mann–Whitney U test was used for the variables of gender, age, work status, and duration of illness, whereas the Kruskal–Wallis H test was applied for education level. We used the p-value of less than 0.05 to indicate a statistical significance at a 95% confidence interval.
RESULTS AND DISCUSSION
In total, 622 questionnaires were distributed. Six were ultimately excluded due to incompleteness, resulting in 616 patients completing the survey, including 267 with diabetes and 349 with hypertension. The mean ± standard deviation (SD) ages of patients were 60.99 ± 8.64 and 63.96 ± 9.66 years for patients with diabetes and hypertension, respectively. Most of the patients were female (69.80%), unemployed (83.61%), and who had a lower education level (i.e., did not complete junior high school, 61.85%). The mean ± SD duration of illness was 5.49 ± 5.54 years for diabetes and 5.54 ± 6.42 years for hypertension (Table 1).
To the best of our knowledge, this study is the first to use the EQ-5D-5L Indonesia value set to assess the HRQOL of the Prolanis patients in Indonesia. The results of this study demonstrated that hypertensive patients have HRQOL scores that are slightly higher than those of diabetic patients although the statistical difference in this case was not significant (Table 2). These findings are congruent with a study from China which evaluated the HRQOL of patients with four kinds of chronic disease, where it was reported that the mean score for hypertension (0.882, standard error: 0.207) was higher than that for cancer, diabetes (0.874, standard error: 0.198), and heart disease (Xu et al., 2017). Similar results have been shared by other studies, in that it was reported that the mean EQ-5D score in diabetes was 0.87 and that for hypertensive patients was 0.92 (SD: 0.17) (Choi et al., 2011; Zhang et al., 2017). However, a study from Korea presented a scenario for HRQOL score where diabetes (0.82) had a higher score than that of hypertension (0.81) to a degree that was better than any of the comorbid disease groups (Chin et al., 2014). This difference, however, might be due to the study being performed in different population than the present investigation.
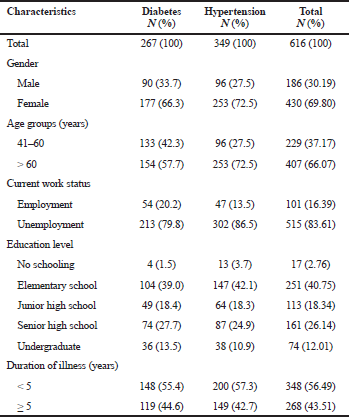 | Table 1. Demographic characteristics of the study participants. [Click here to view] |
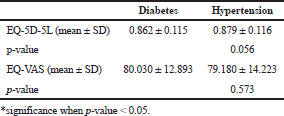 | Table 2. Study sample descriptive characteristics of EQ-5D-5L. [Click here to view] |
The utility score ranges from zero points (death or worse than death) to one point (perfect health). In this research, the mean score of the utility of the Prolanis patients was categorized as relatively high when compared with the results of other studies involving chronic disease patients, where, in general, patients with hypertension or diabetes tended to have a lower QOL score than nonhypertensive or nondiabetic patients. Some studies showed a lower utility score in diabetic patients (mean ± SD: 0.74 ± 0.27) (Redekop et al., 2002), worsening mean EQ-5D score in patients with diabetes after 5 years (mean ± SD: from 0.798 ± 0.174 to 0.767 ± 0.186; p-value 0.001) (Grandy and Fox, 2012), and a much lower HRQOL score for hypertension (mean ± SD: 0.467 ± 0.284), as they used the value set from the United Kingdom population (Saleem et al., 2014). This was confirmed by a meta-analysis of observational studies, which suggested hypertensive patients to have a lower QOL (Trevisol et al., 2011).
When considering other studies evaluating the HRQOL in chronic disease management patients, the results show a higher score than a primary care-based disease management study performed in Chicago, wherein the mean score of diabetic patients was 0.826 (standard error of the mean: 0.027), and in a medical assistant-based care management with high-risk patient including diabetes, a mean ± SD score of 0.64 ± 0.22 was observed (Freund et al., 2016; Ose et al., 2009). However, we found that a systematic review evaluating the difference of self-management versus usual care of patients with chronic conditions showed that there was no difference (p = 0.08) (Franek, 2013).
The EQ-5D health states of diabetic and hypertensive patients suggested that the most frequently reported problems were pain/discomfort followed by anxiety/depression, whereas the least common problem was in the domain of self-care and usual activity (Table 3). A study comparing the HRQOL in diabetic patients showed that anxiety/depression was the problem most reported from patients who otherwise were without complications (Redekop et al., 2002). This differed from a study wherein pain/discomfort (40.2%) and mobility (35.5%) were the most frequent problems reported among diabetic patients (Choi et al., 2011) and a study in China where 50.9%–54.3% of chronic patients reported that they had no problem in the domain of pain/discomfort (Xu et al., 2017). Conversely, a similar result was presented in a study, wherein 29.1% of hypertensive patients indicated that they had no problem with self-care and usual activity (Saleem et al., 2014). Another study in Cyprus reported that anxiety/depression was the most frequent dimension causing problems in hypertensive patients (27.6%), whereas the majority reported no problem in the self-care dimension (97.7%–98.7%) and the usual activity domain (93.4%–97.2%) (Theodorou et al., 2011). The results suggest that healthcare professionals in Prolanis should offer more attention to diabetic and hypertensive patients, especially in the areas of pain and depression management.
Comparisons of the EQ-5D-5L scores with each characteristic are shown in Table 4. Among five characteristics, a significant difference in the HRQOL score was only revealed in relation to the employment status of diabetic patients (p = 0.016). Male gender, younger age, employed status, and a shorter duration of illness tended to correlate with higher HRQOL scores. A lower educational level in diabetes was also found to have a higher score. Meanwhile, the opposite trend was present among hypertensive patients, where those with higher educational levels tended to report higher HRQOL scores.
This study showed that work status was the only significant characteristic associated with HRQOL score in diabetic patients. Redekop et al. (2002) noted that older age, female sex, insulin therapy, obesity, and complications were associated with a lower HRQOL (Redekop et al., 2002). Another study in Nepal found that increasing age, marital status, and educational status were strongly associated with the QOL of hypertensive patients in a physical component summary though the study used the Short Form-36 questionnaire as the instrument (Bhandari et al., 2016). A study in Korea presented that age, household income, marital status, and employment status were significantly different between the diabetic and nondiabetic patients (Choi et al., 2011). Significantly the lower values of HRQOL were demonstrated in a study in correlation with female sex, smoking, and the absence of higher education in patients with chronic conditions in the United Kingdom (Heyworth et al., 2009). A study in China stated that male gender, young age, and higher education promoted a higher EQ-5D score (Xu et al., 2017). A study conducted in Pakistan showed that education, income, and locality were significantly related with HRQOL score in hypertensive patients (Saleem et al., 2014). The difference between such and the results in our study might be because the treatments that patients receive from the Prolanis program are similar. The attendance rate at every meeting was also relatively high. The characteristics of patients with regard to disease severity were also similar, where only a limited number of patients reported complications. We can conclude that the EQ-5D scores among the patients were relatively high when compared with other studies.
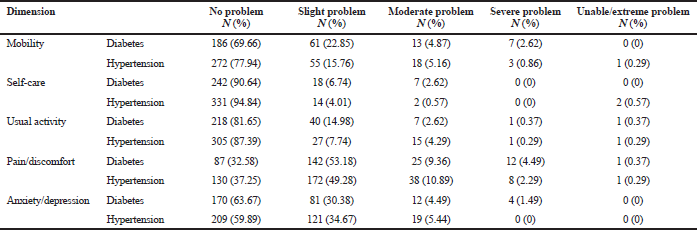 | Table 3. Patients’ responses to the EQ-5D-5L descriptive system in each dimension. [Click here to view] |
 | Table 4. Distribution of the EQ-5D-5L score among patients with different characteristics. [Click here to view] |
The limitations of this study were that older age and education level of the patient can affect the interpretation of the EQ-VAS score, where the majority of participants found difficulties while reading the scale and indicating their health states on it. The participants were selected by convenient sampling, and even though the cohort size is fairly large, generalizations should be made with caution. Further study deploying cost–utility analyses of the data of the Prolanis program should be conducted or comparisons with non-Prolanis patients should be made to evaluate HRQOL differences between the groups.
CONCLUSION
This study determined that the HRQOL of patients receiving chronic disease management was relatively high. The most frequent health problems reported were pain/discomfort and anxiety/depression. Health professionals in the Prolanis program should pay more attention to pain and depression management where warranted to increase the QOL of patients.
ACKNOWLEDGMENTS
This study was funded by a grant from Universitas Jenderal Soedirman. We thank to our students: Alan Faridi, Kintyas Asokawati, and Siti Sarah Chandriani for collecting the data. The authors report no conflicts of interest for this work.
REFERENCES
Bardage C, Isacson DGL. Hypertension and health-related quality of life: an epidemiological study in Sweden. J Clin Epidemiol 2001; 54(2):172–81. CrossRef
Bhandari N, Bhusal BR, Takma KC, Lawot I. Quality of life of patient with hypertension in Kathmandu. Int J Nurs Sci 2016; 3(4):379–84. CrossRef
BPJS Kesehatan. Panduan Praktis PROLANIS Program Pengelolaan Penyakit Kronis, 2014. [ONLINE]. Available via https://bpjs-kesehatan.go.id/bpjs/dmdocuments/06-PROLANIS.pdf (Accessed 27 November 2017).
Chin YR, Lee IS, Lee HY. Effects of hypertension, diabetes, and/or cardiovascular disease on health-related quality of life in elderly Korean individuals: a population-based cross-sectional survey. Asian Nurs Res (Korean Soc Nurs Sci) 2014; 8(4):267–73. CrossRef
Choi YJ, Lee MS, An SY, Kim TH, Han SJ, Kim HJ, Chung YS, Lee KW, Kim DJ. The relationship between diabetes mellitus and health-related quality of life in Korean adults: the fourth Korea national health and nutrition examination survey (2007–2009). Diabetes Metab J 2011; 35(6):587–94. CrossRef
Endarti D, Riewpaiboon A, Thavorncharoensap M, Praditsitthikorn N, Hutubessy R, Kristina SA. Evaluation of health-related quality of life among patients with cervical cancer in Indonesia. Asian Pac J Cancer Prev 2015; 16(8):3345–50. CrossRef
EuroQol Goup. EQ-5D-5L, 2017. [ONLINE]. Available via https://euroqol.org/eq-5d-instruments/eq-5d-5l-about/ (Accessed 27 November 2017).
Fitzpatrick R, Fletcher A, Gore S, Jones D, Spiegelhalter D, Cox D. Quality of life measures in health care. I: Applications and issues in assessment. BMJ 1992; 305(6861):1074–7. CrossRef
Franek J. Self-management support interventions for persons with chronic disease: an evidence-based analysis. Ont Health Technol Assess Ser 2013; 13(9):1–60.
Freund T, Peters-Klimm F, Boyd CM, Mahler C, Gensichen J, Erler A, Beyer M, Gondan M, Rochon J, Gerlach FM, Szecsenyi J. Medical assistant–based care management for high-Risk patients in small primary care practices: a cluster randomized clinical trial medical assistant–based care management in small primary care practices. Ann Intern Med 2016; 164(5):323–30. CrossRef
Grandy S, Fox KM. Change in health status (EQ-5D) over 5 years among individuals with and without type 2 diabetes mellitus in the SHIELD longitudinal study. Health Qual Life Outcomes 2012; 10(1):99. CrossRef
Heyworth ITM, Hazell ML, Linehan MF, Frank TL. How do common chronic conditions affect health-related quality of life? Br J Gen Pr 2009; 59(568):e353–8. CrossRef
Hussain MA, Al Mamun A, Peters SAE, Woodward M, Huxley RR. The burden of cardiovascular disease attributable to major modifiable risk factors in Indonesia. J Epidemiol 2016; 26(10):515–21. CrossRef
Kristina SA, Endarti D, Widayanti AW, Widiastuti M. Health-related quality of life among smokers in Yogyakarta Province, Indonesia. Int J Pharm Clin Res 2015; 8(1):95–9.
Manjunath K, Christopher P, Gopichandran V, Rakesh PS, George K, Prasad JH. Quality of life of a patient with type 2 diabetes: a cross-sectional study in Rural South India. J Fam Med Prim care 2014; 3(4):396. CrossRef
Ministry of Health Republic of Indonesia. Laporan Nasional Riskesdas 2018, Ministry of Health Republic of Indonesia, Jakarta, Indonesia, 2018.
Ministry of Health Republic of Indonesia. Riset Kesehatan Dasar 2013, Ministry of Health Republic of Indonesia, Jakarta, Indonesia, 2013.
Ose D, Wensing M, Szecsenyi J, Joos S, Hermann K, Miksch A. Impact of primary care–based disease management on the health-related quality of life in patients with type 2 diabetes and comorbidity. Diabetes Care 2009; 32(9):1594–6. CrossRef
Palermo TM, Long AC, Lewandowski AS, Drotar D, Quittner AL, Walker LS. Evidence-based assessment of health-related quality of life and functional impairment in pediatric psychology. J Pediatr Psychol 2008; 33(9):983–96. CrossRef
Purba FD, Hunfeld JAM, Iskandarsyah A, Fitriana TS, Sadarjoen SS, Ramos-Goñi JM, Passchier J, Busschbach JJ. The Indonesian EQ-5D-5L value set. Pharmacoeconomics 2017; 35(11):1153–65. CrossRef
Purba FD, Hunfeld JAM, Iskandarsyah A, Fitriana TS, Sadarjoen SS, Passchier J, Busschbach JJ. Quality of life of the Indonesian general population: test-retest reliability and population norms of the EQ-5D-5L and WHOQOL-BREF. PLoS One 2018;13(5). CrossRef
Rabin R, Gudex C, Selai C, Herdman M. From translation to version management: a history and review of methods for the cultural adaptation of the euroqol five-dimensional questionnaire. Value Heal 2014;17(1):70–6. CrossRef
Redekop WK, Koopmanschap MA, Stolk RP, Rutten GEHM, Wolffenbuttel BHR, Niessen LW. Health-related quality of life and treatment satisfaction in Dutch patients with type 2 diabetes. Diabetes Care 2002; 25(3):458–63. CrossRef
Rubin RR, Peyrot M. Quality of life and diabetes. Diabetes Metab Res Rev 1999; 15(3):205–18. CrossRef
Saleem F, Hassali MA, Shafie AA. A cross-sectional assessment of health-related quality of life (HRQoL) among hypertensive patients in Pakistan. Heal Expect 2014; 17(3):388–95. CrossRef
Setiawan D, Dusafitri A, Galistiani GF, van Asselt ADI, Postma MJ. Health-related quality of life of patients with HPV-related cancers in Indonesia. Value Heal Reg Issues 2018; 15:63–9. CrossRef
Theodorou M, Kaitelidou D, Galanis P, Middleton N, Theodorou P, Stafylas P, Siskou O, Maniadakis N. Quality of life measurement in patients with hypertension in Cyprus. Hell J Cardiol 2011; 52(5):407–15.
Trevisol DJ, Moreira LB, Kerkhoff A, Fuchs SC, Fuchs FD. Health-related quality of life and hypertension: a systematic review and meta-analysis of observational studies. J Hypertens 2011; 29(2):179–88. CrossRef
WHO. Global health observaroty data, Indonesia country profile 2015, 2015. [ONLINE]. Available via http://www.who.int/gho/countries/idn/country_profiles/en/ (Accessed 29 November 2017).
Xu RH, Cheung AWL, Wong EL-Y. Examining the health-related quality of life using EQ-5D-5L in patients with four kinds of chronic diseases from specialist outpatient clinics in Hong Kong SAR, China. Patient Prefer Adherence 2017; 11:1565. CrossRef
Zhang L, Guo X, Zhang J, Chen X, Zhou C, Ge D, Qian Y. Health-related quality of life among adults with and without hypertension: a population-based survey using EQ-5D in Shandong, China. Sci Rep 2017; 7(1):14960. CrossRef