INTRODUCTION
Prevalence of metabolic obesity also termed as metabolic syndrome and insulin resistance (IR) is increasing drastically throughout the world, and it is most common in Asian adults. In India, 41% of the adult population with age >21 years are metabolically obese. Its prevalence increases with age (Ramachandran et al., 2003). The decreased ability of insulin to promote glucose utilization is called IR. The secretion and production of insulin, usually increased by pancreatic β-cells as a compensatory mechanism (hyperinsulinemia), but in that mechanism, glucose tolerance remains normal (Oliveira et al., 2004). A problem of overall health and its effects even on children and adolescents indicates the IR. The development of obesity as seen by the occurrence of co-morbidities and complications as a result of excess weight is a big concern for the clinician (Cook et al., 2003). A set of risk factors for cardiovascular disease (CVD) is represented by metabolic obesity or metabolic syndrome. The assessment of coronary artery disease (CAD) with respect to metabolic status and body mass index (BMI) is poorly studied. The identification of metabolic obesity risk factors may be helpful in prevention of cardiovascular diseases in the near future. In patients, the development and extent of coronary CAD are not uniform. At present, IR is a known etiology for directly predicting the occurrence of CAD (Reaven, 1997), but the status of IR has not been investigated in depth for the severity of CAD. A significant correlation between IR and severity of CAD can be used for the detection of high-risk individuals through a simple test. Identification of patients who are not candidates for angioplasty even with severe and extensive disease can be done easily. Hence, this study aims to analyze the relationship between IR measured by homeostatic model assessment for IR (HOMA-IR) and severity of CAD measured by SYNTAX score as demonstrated via a coronary angiogram (CAG). SYNTAX score is a well-established validated tool to measure the severity of CAD in patients with diabetes mellitus (DM).
METHODS AND MATERIALS USED
Study population
The study was a prospective cross-sectional observational study conducted from January 2016 to December 2017. A total of 532 patients with stable angina who had undergone CAG for the evaluation of CAD were recruited from a tertiary care center in South India. The sample size was calculated based on the power of the study and the proportions of the groups. The patients belonged to the age group of 25–80 years. Patients with a previous history of CAD and heart failure were excluded. Those with ongoing non-cardiac comorbidities, such as infectious diseases, chronic inflammatory disorders, and viral illnesses (retroviral, hepatitis B and C) and chronic kidney disease were also excluded from the study.
Ethical considerations
The study has obtained the approval from Kasturba Medical College-Institutional Ethics Committee (IEC) of Manipal Academy of Higher Education, Manipal, India, and informed consent form was collected from all the patients. Ethical approval number was KH-IEC 644/2015.
Diagnostic criteria
All the patients underwent a personal interview using a customized questionnaire that included data on smoking and physical activity, height and weight, and waist and hip circumference were measured to calculate BMI and waist-hip ratio (WHR), respectively. Anthropometric measurements were recorded before the patients underwent CAG. Details of medications, clinical history of DM, and hypertension were also recorded.
According to the NCEP-ATPIII criteria, metabolic obesity (metabolic syndrome) include five risk factors, i.e., serum Triglyceride level (>150 mg/dl), high-density lipid (HDL) levels (<40 mg/dl male, <50 mg/dl female), plasma glucose at at least 8 hours of fasting (>110 mg/dl), blood pressure (135/80 mmHg), and waist circumference (>102 for male, >88 for female). Those patients presented with three or more of the above-mentioned risk factors were considered as metabolically obese, otherwise metabolically healthy. Based on the Asia-Pacific criteria for obesity, a BMI >25 kg/m2 in patients was considered as phenotypical obese (Weisell, 2002).
Biochemical assessment
Blood samples of the patients were collected at baseline admission (before undergoing CAG). Fasting blood sugar (FBS), total cholesterol, and HDL cholesterol were measured using autoanalyzer, Hitachi P-800. Fasting insulin level was measured using another autoanalyzer (Roche Diagnostics, Basel, Switzerland), and sphygmomanometer was used to record the systolic blood pressure using mercury.
IR was measured by HOMA-IR computerized method, which has previously shown good correlation with a euglycemic clamp for use in cross-sectional studies. The severity of CAD was evaluated and SYNTAX Scoring method was used to calculate the same. SYNTAX Scoring was carried out by a team of cardiologists who were unaware of the other parameters recorded for each patient.
Statistical analysis
SPSS Software version 20.0 was used for statistical analysis (SPSS Inc., Chicago, Illinois). Demographic characteristics were presented using frequency and descriptive analysis. Association between the various study parameters was assessed using regression analysis (Odds ratio). Relationship between HOMA-IR and SYNTAX Score was assessed using correlation (with a 95% confidence interval). Statistically significance was considered at a p-value of less than 0.05.
RESULTS
The study population had a mean age of 57.58 ± 10.40 years out of which majority were males (69.4%). Out of the total 532 subjects, 51.3% were hypertensive, 14.5% were smokers, 29.1% consumed alcohol, 49.3% were metabolically obese, and 50% were phenotypically obese. CAG was done to confirm the diagnosis of CAD and to assess the SYNTAX score. Among all, 50.5% showed mild CAD in by CAG report and rest of patients had shown to have diseased vessels and underwent percutaneous transluminal coronay angioplasty. One hundred and six (19.9%) patients showed to have single vessel disease (SVD) followed by double vessed disease (DVD) in 77 (14.5%) patients. Laboratory investigations related to diagnosis of the disease and to rule out comorbidities were done and mentioned with socio-demographic data as shown in Table 1.
SYNTAX score in our study was defined as low risk (0–22) and high risk (>22) and scatter plot representing the association between CAD severity score and, IR is showed in Figure 1.
IR showed a positive correlation with the severity of CAD in metabolically obese subjects. It indicates that an increase in IR increases the severity of CAD in metabolically obese subjects (OR = 2.51, p = 0.048) (Table 2). Phenotypically obese population was not significantly correlated with IR in stable-angina patients (p = 0.08 with negative OR) (Table 3). Male gender is associated with high SYNTAX score, and it showed five-folds more severe heart attack in both metabolic and phenotypic obesity status (OR = 5.57, p ≤0.001 and OR = 5.13, p ≤ 0.001).
DISCUSSION
There are studies which have shown the association of IR with CAD in relation to diabetes (Mahabala et al., 2013), but this study has assessed the relationship between IR with severity of CAD in 532 patients in relation to metabolic and phenotypic obesity. This study showed a positive statistically significant (r = 2.5, p = 0.048) association between these parameters.
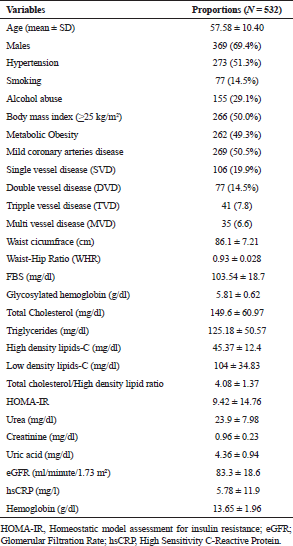 | Table 1. Socio-demographic and clinical characteristics of the study population. [Click here to view] |
A previously conducted study had shown that there is no association between IR with the severity of CAD in non-diabetic men (Kruszelnicka et al., 2013). Another study showed that patients with a higher level of IR had been associated with the more severe types of CAD (Graner et al., 2007).
Altered insulin signaling in endothelial cells can help in understanding an important mechanism for the increased likelihood of cardiovascular disease (Aziz and Wheatcroft, 2011). Endothelial dysfunction developed by alteration leads to the advancement of atherosclerosis along with the pro-inflammatory state generated by IR (Zornitzki et al., 2007). Although IR is known to be a part of the metabolic syndrome, the other clinical markers, such as index measurements of body-mass and truncal obesity, have low sensitivity and specificity in identifying IR (UKPDS Group, 1998).
All through the natural history of type 2 DM, IR has been the only component that has remained constant, with reference to metabolic syndrome. IR and its measurement by HOMA-IR method has remained unchanged even with the traditional treatment methods of type 2 DM during the many years of the UK prospective diabetes study (Wallace et al., 2004). All the other biochemical risk factors and anthropometric measurements change over a period with or without treatment. This unique feature of the IR along with its association with the severity of CAD can be used to identify the high-risk individual. A patient whose HOMA-IR is very high initially can develop severe coronary artery disease and may benefit in emergency and with specific and advanced diagnostic procedures and aggressive medical management.
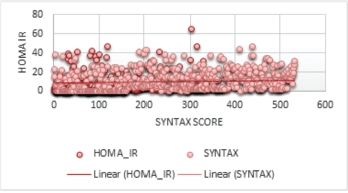 | Figure 1. Scatter plot showing a positive linear correlation between the severity of CAD (SYNTAX score) and homeostasis model assessment IR in the metabolically obese group. [Click here to view] |
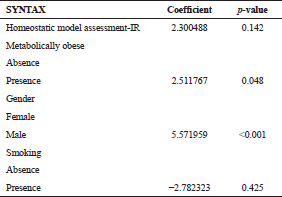 | Table 2. Association between HOMA IR and SYNTAX score in association to metabolic status. [Click here to view] |
Especially, in a resource-limited setting, HOMA-IR can aid the prediction of CAD and its severity with clinical relevance. Since the measurement of IR using HOMA can be performed easily, it has shown good correlation with euglycemic clamp method which is a reference standard method for measuring IR, and hence can be potentially used in routine clinical practice. Thus in the near future, we might be able to predict the severity of CAD using HOMA-IR and identification of patients who are not candidates for angioplasty even with severe and extensive disease can be done easily.
The limitation of this study is its cross-sectional design. HOMA measured IR can help us in assessing the long-term effect of risk factors in patients with CVD if it is compared with angiographic findings at the beginning of the disease.
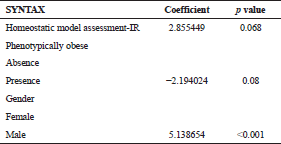 | Table 3. Association between HOMA IR and SYNTAX score in association to obesity status. [Click here to view] |
CONCLUSION
According to this study, an increase in IR increases the risk of severity of CAD in metabolically obese subjects but not in the case of phenotypically obese subjects. Hence, IR can be used to predict the severity of CAD in metabolically obese subjects only.
ABBREVIATIONS
| CVD | Cardiovascular diseases; |
| CAD | Coronary artery disease; |
| CAG | coronary angiogram; |
| IR | Insulin resistance; |
| HOMA | Homeostatic model assessment; |
| HDL | High density lipid; |
| DM | Diabetes mellitus; |
| FBS | Fasting blood sugar; |
| WHR | Waist-hip ratio; |
| BMI | Body mass index; |
| IEC | Institutional ethics committee. |
AUTHOR’S CONTRIBUTION
All authors have equally contributed to the research process and manuscript preparation.
FINANCIAL SUPPORT
None.
CONFLICTS OF INTEREST
Authors declare that there are no conflict of interest.
REFERENCES
Aziz A, Wheatcroft S. Insulin resistance in Type 2 diabetes and obesity: implications for endothelial function. Expert Rev Cardiovasc Ther, 2011; 9(4):403–7. CrossRef
Cook S, Weitzman M, Auinger P, Nguyen M, Dietz W. Prevalence of a metabolic syndrome phenotype in adolescents. Arch Pediatr Adolesc Med, 2003; 157(8):821. CrossRef
Graner M, Syvänne M, Kahri J, Nieminen M, Taskinen M. Insulin resistance as predictor of the angiographic severity and extent of coronary artery disease. Ann Med, 2007; 39(2):137–44. CrossRef
Kruszelnicka O, Surdacki A, Golay A. Differential associations of angiographic extent and severity of coronary artery disease with asymmetric dimethylarginine but not insulin resistance in non-diabetic men with stable angina: a cross-sectional study. Cardiovasc Diabetol, 2013; 12(1):145. CrossRef
Mahabala C, Srinivasan M, Manjrekar P, Unnikrishnan B, Ullal A, Kamath P, Kotekar M. Correlation of severity of coronary artery disease with insulin resistance. North Am J Med Sci, 2013; 5(10):611. CrossRef
Oliveira C, Mello M, Cintra I, Fisberg M. Obesidade e síndrome metabólica na infância e adolescência. Rev Nutr, 2004; 17(2):237–45. CrossRef
Ramachandran A, Snehalatha C, Satyavani K, Sivasankari S, Vijay V. Metabolic syndrome in urban Asian Indian adults—a population study using modified ATP III criteria. Diabetes Res Clin Pract, 2003; 60(3):199–204. CrossRef
Reaven G. Role of insulin resistance in human disease. Nutrition, 1997; 13(1):64. CrossRef
UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet, 1998; 352(9131):837–53. CrossRef
Wallace T, Levy J, Matthews D. Use and Abuse of HOMA Modeling. Diabetes Care, 2004; 27(6):1487–95. CrossRef
Weisell R. Body mass index as an indicator of obesity. Asia Pac J Clin Nutr, 2002; 11(s8):S681–4. CrossRef
Zornitzki T, Ayzenberg O, Gandelman G, Vered S, Yaskil E, Faraggi D, Caspi A, Goland S, Shvez O, Schattner A, Knobler H. Diabetes, but not the metabolic syndrome, predicts the severity and extent of coronary artery disease in women. QJM, 2007; 100(9):575–81. CrossRef