INTRODUCTION
Schizophrenia is a chronic and serious mental illness, profoundly affecting patient’s emotions, thinking, and behavior. Despite the availability of various psychiatric services and effective treatment for schizophrenia, low adherence rate to the prescribed antipsychotics is a major cause of psychotic relapse. The overall non-adherence rate is about 50% for people with schizophrenia (Barkhof et al., 2012; Weiden et al., 1991; Young et al., 1986). Indeed, the average risk of relapse is 3.7 times greater in patients who were not adhering to the treatment compared with those who adhered (Fenton et al., 1997). Further compounding this problem is the inadequate clinical information on medications received by the patients and care-givers. Those from the low levels of education will normally search for people’s opinions or experiences, occasionally information from the internet of undetermined sources. This will influence the decision of the patients and may lead to patients choosing for inappropriate treatment or discontinue the medications by themselves (Hussainy et al., 2011). Furthermore, peoples with a psychiatric disorder have a lower quality of life because of the marginalization and discrimination from the community as well as disabilities due to the disease (Xiang et al., 2007).
In Malaysia, there is an increasing trend of people newly diagnosed with schizophrenia. The incidence of new cases is about 100/100,000 per year (Aziz, 2007). Comprehensive psychiatric services are available to people with schizophrenia in Malaysia. For instance, a home care service has been established in Hospital Bahagia Ulu Kinta, a government psychiatric hospital. It was formalized since the year 2002 which consist of multidisciplinary peoples, including the psychiatrist, medical officers, and nurses with ongoing improvements in line with the Mental Health Act 2001 and Mental Health Regulations 2010. The pharmacist was recruited to join the home care team in the year 2010 and plays a proactive role in conducting home medication review (HMR) program. The HMR program helps patients who are at risk of experiencing medication-related problems at home and ensure medication adherence of all the patients. Indeed, the World Health Organization (WHO) (1994) and the European Council (Council of Europe CoM, 2001) have stressed the importance of including pharmacists as an active member of the multidisciplinary HMR team with the aim of benefiting patients’ health, including those suffering from mental disorders (WHO, 2005). The development of the HMR program in 2004 and HMR protocol in 2011 is one of the advancements in the practice of pharmacy in Malaysia. However, little is known about the impact of the HMR program since its implementation in Malaysia particularly among people with schizophrenia.
This study was to evaluate the impact of pharmacist-led HMR program on medication adherence, knowledge toward antipsychotic drugs, and quality of life among people with schizophrenia.
METHODS
This observational, prospective longitudinal study was conducted from October 2012 to December 2013 in patient’s home at Kinta district, Perak, Malaysia. The study had granted ethics approval from the Medical Research and Ethics Committee, Ministry of Health Malaysia at 12 October 2012 in accordance to the local regulations which involves human subjects (ethical approval number: NMRR-12-691-13067). This study was carried out on people with schizophrenia under the care of home care team in Hospital Bahagia Ulu Kinta, Kinta district, Perak, Malaysia. The inclusion criteria were all the patients diagnosed with schizophrenia according to the Diagnostic and Statistical Manual of Mental Disorders IV (DSM-IV). The patients must have the minimum duration of illness of 1 year. The age of the patients must be between 18 and 60 years old. The patients were recruited by using convenient sampling method. Patients who are able to understand the purpose of the study and willing to give consent were recruited. Patients aged more than 60 were excluded because they are more susceptible to neuropsychiatric disorders, such as dementia, depression, and anxiety disorder. Those with severe schizophrenia and those in a manic phase or acute psychosis were excluded.
The sample size required for this study was calculated based on the formula for a comparison of two proportions (two-sided) (Bland et al., 2012). A total sample size of 110 home care patients was needed to be sufficient to detect a difference of 25% (Finley et al., 2002; Haynes et al., 2008) between groups of the patients judged to have adequate adherence with an 80% power and a 5% significance level. After considering the predicted drop-out rate of around 40%, a total of 153 patients were recruited.
Standardized data collection forms were used to collect data from patients during each visit. Medication adherence was evaluated by a validated medication adherence rating scale (MARS) (Thompson et al., 2000) and pill count method (Grymonpre et al., 1998). The percentage of doses taken is calculated based on the following formula (Grymonpre et al., 1998):
Patient’s knowledge of antipsychotics was assessed by a standardized validated questionnaire formulated by the researcher of this study. The questionnaire has gone through face and content validation by two experts from University Sciences Malaysia. Quality of life was measured by the Sheehan disability scale (SDS) (Sheehan et al., 1996). Permission to use the MARS and SDS in this study has been obtained from the authors of the scales.
The HMR program consisted of 6-month follow-up home visit by the pharmacist. One single pharmacist (the first author) performed all the HMRs throughout the study period. The interval between the visits within 6 months was in 1-, 3-, and 6-month gap period. After attaining patient’s written informed consent during the first visit, baseline information such as demographic data, medication adherence, knowledge of the medications, and quality of life were collected from the patient. Comprehensive medication review was given by the pharmacist for the first contact. The comprehensive medication review focused on the drug regimens of the individual patient, assessment on the possible drug-drug interaction, appropriateness of medication administration, and possible side effects. Additionally, medication review activities included medication counseling was provided to the patients based on the psychoeducation module established by Ministry of Health Malaysia (Family Health Department Division, 2001; Ministry of Health Malaysia, 2009).
During the second (post 1 month), third (post 3 months), and fourth HMR visit (post 6 months), the patients were assessed again regarding their adherence to the medications, knowledge of the medications, and quality of life. Comprehensive medication review was given again by the pharmacist during each visit. Patient’s current status, identified drug-related problems and monitoring results, intervention plans, changes in the patient’s medication list, allergies, and adverse drug reactions were addressed during each visit.
All the raw data were processed and entered into the Statistical Package for the Social Sciences, SPSS® program version 20.0 software. For demographic continuous variables, descriptive statistics such as mean, median, standard deviation, and interquartile range (IQR) were used. Mean and standard deviation was applied for continuous variables with a normal distribution. Median and IQR were presented for continuous variables without a normal distribution. Categorical variables were summarized in frequency and percentage. Normality of the data was tested by Kolmogorov–Smirnov test. As the results showed that the data were not normally distributed, Friedman analysis of variance (ANOVA) test was used to compare the difference of the outcome measures at baseline, 1-, 3-, and 6-month follow up. Regarding the comparisons within groups, follow-up post-hoc analysis was conducted by using Wilcoxon Signed-Rank test to determine the differences between the outcome measures at baseline and 1 month; baseline and 3 months; and baseline and 6-month follow up. As Wilcoxon Signed-Rank test was being used for several times, the Holm’s Sequential Bonferroni method was used to control Type l error for all the pair-wise comparisons. Statistical significance was set at a two-tailed p value of less than 0.05 for all the statistical analysis in this study.
RESULTS
Demographic data
Out of 478 patients, a total of 153 people with schizophrenia who met the inclusion criteria were enrolled in this study. Twenty patients did not complete the study due to withdraw consent, working, and readmitted to the hospital. There were 133 patients who had completed this study. The dropout rate for this study was 13.1%. The demographic characteristics of the patients are illustrated in Table 1.
Adherence to antipsychotics
The mean MARS score was 8.42 ± 1.40 at baseline. After 6 months, the mean MARS score showed that the patients’ adherence to medications was significantly improved from baseline (Fig. 1). The results also showed significant improvement in the mean MARS score between baseline and post 1 month, baseline and post 3 months, as well as baseline and post 6-month follow up (Table 2).
The pill count method had revealed that the mean percentage of prescribed medications taken by the patients had shown significant improvement with HMR program at 1, 3, and 6 months as compared to the baseline. The improvement was more prominent particularly between the 1-month follow up and baseline period. The mean percentage of the medication taken at the end of the study was 90.37% as compared to 56.68% at baseline (Table 2).
Knowledge of antipsychotics
The patients’ knowledge score had improved significantly with the HMR program. When comparing the baseline mean knowledge score with the mean scores at 1-, 3-, and 6-month follow up, the results showed significant improvements between all the comparisons pairs (Table 3).
At baseline, more than 80% of the patients answered correctly to the questions concerning the timing, method of administration, ability to identify the color and shape of each drug, and the storage of the medications. However, more than 50% of the patients were unable to tell the name, purpose, and the doses of the prescribed medications. Only 61.7% of them gave the correct answer about side effects. After 1 month of the HMR program, the patients’ knowledge about the indication, dosage, and possible side effects of each of their prescribed drug have highly improved. Approximately, 95% of the patients gave the correct answer for seven out of eight items of the medication knowledge score at the fourth visit (6-month follow up) (Table 4).
Quality of life
The three major domains in the SDS were used in the final analysis, which are the patient’s work, social life, and family life/home responsibilities. The three domains are summed into a single dimensional measure, ranges from 0 (unimpaired) to 30 (highly impaired). The analysis showed the baseline total mean SDS score of 5.32 ± 7.10 and reduced to 2.56 ± 4.41 after the fourth HMR visit. However, the statistical test showed no significant improvement for the total SDS score (Table 5).
The mean “work” component score at baseline, 1-, 3-, and 6-month follow up were at the mildly impaired category (0–3). The differences in the scores were not significant between the baseline, 1, 3, and 6 months of HMR follow up (Table 5).
The statistical analysis found no significant difference between the baseline and post 1-month follow up mean score of the “social” component of SDS. However, the mean score at baseline was significantly different from the post 3- and post 6-month follow up. This indicates that there was a significant improvement in the “social” component of the quality of life assessment at the third and fourth HMR visit (Table 5).
The mean scores for the “family” component of SDS scale were rated under the mildly impaired category (0–3) by the patients and the differences between the scores were significant at 1-, 3-, and 6-month follow up as compared to baseline. The decreasing trend of the score reflects that the patients have a better improvement for the “family” component of quality of life assessment (Table 5).
DISCUSSION
Adherence to antipsychotics
The patient’s medication adherence showed significant improvement at each HMR follow up as shown by the medication adherence measures (pill counts and MARS). This finding suggested that HMR program conducted by the pharmacist on people with schizophrenia has a positive impact on medication adherence. A similar result was observed in a preliminary study conducted in Malaysia (Mustapa et al., 2008) among diabetes mellitus and/or hypertension patients. The patient demonstrated better treatment adherence based on pill count with the adherence rate of 41.4% and 80.2%, respectively, at before and after the HMR conducted by the pharmacist (Mustapa et al., 2008). A previous randomized controlled study in Australia (Naunton and Peterson, 2003) on high-risk elderly patients who were aged 60 or above and having four or more prescribed medications had found similar findings. The study was focused on home-based follow up by the pharmacist and the patients showed significant improvement in medication adherence as compared to the control group (Naunton and Peterson, 2003). Besides, there are several studies which demonstrated a positive impact on patient’s medication adherence and management among elderly patients living in their homes after domiciliary medication review by the pharmacist (Begley et al., 1997; Lowe et al., 2000; Okuno et al., 1999; Raynor et al., 2000).
Pharmacist-led HMR program provides the opportunity for the pharmacist to interact with patients in their home and provide supports on medication adherence with the presence of a caregiver. A systematic review by Holland et al. (2008) specifically looking at the provision of HMR service to the elderly revealed a positive impact on medication adherence as well. The overall positive outcome may relate to the relationship established between the pharmacist and the patient in a home care setting. The HMR setting may allow the patients easier to discuss their medication adherence difficulties as compared to pharmacy service conducted in a busy outpatient pharmacy setting (Begley et al., 1997). This finding proves that the extended role of pharmacist to shift the service care to patient’s home is utmost important. However, there are limited studies on the impact of HMR service among people with schizophrenia. Therefore, the present study highlighted that pharmacist-led HMR can be targeted at people with schizophrenia whom medication adherence is a particular problem at home.
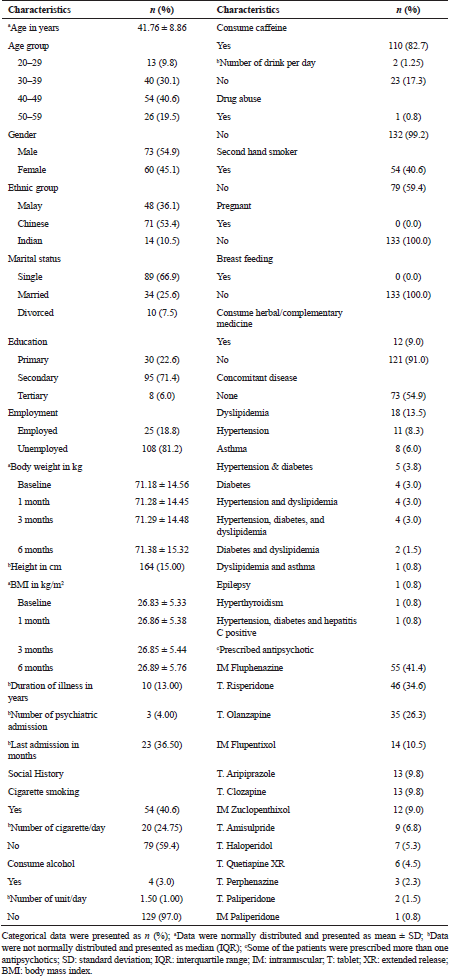 | Table 1. Demographic characteristics of the patients. [Click here to view] |
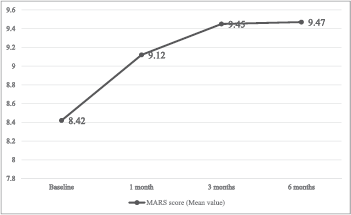 | Figure 1. Comparison of MARS score at baseline, 1-, 3-, and 6-month follow up. [Click here to view] |
Knowledge of antipsychotics
Inadequate or lack of knowledge about medications can pose a potential patient’s inability to take their medications accordingly. In this study, the medication knowledge of the patients improved significantly at each follow-up visit. The result ascertains the positive impact of pharmacist-led HMR in improving patients’ understanding of their treatment and this positive trend is similar in a systematic review by Holland et al. (2008) among elderly. A study by Begley et al. (1997) targeted on elderly also reported significant improvement in the knowledge score among the subjects after a domiciliary visit by the pharmacist. A study by Shaw et al. (2000) gave a contradictory finding that there was an improvement in total knowledge score in both control and intervention groups (home visit by community pharmacist after receiving pharmacy discharge plan from the hospital) among people with schizophrenia and the result was not significant difference between the intervention and control group. However, a higher knowledge score was observed in the intervention group.
This study showed a significant impact of HMR service on the patients’ knowledge of their medications particularly the indication and the proper dosage. The number of patients who answered correctly the indication of their medications was increased from 45.9% to 97.0%. This finding is identical with the reports from Lowe et al. (2000) (improved from 58.0% to 88.0%) and Raynor et al. (2000) (improved from 58.0% to 90.0%) for elderly patients at home. The improvement in knowledge about the dosage of the drug is crucial for patients to avoid the possibility of underdose which would affect the efficacy and the potential risk of overdose which may lead to toxicity (Raynor et al., 2000). Nevertheless, the patients’ knowledge on their drug name remained low. This finding was similar to the study conducted by Okuno et al. (1999) in Japan on elderly who received medication counseling from the pharmacist during a home visit. The possible reasons for this observation may be due to the concentration difficulties among the schizophrenia peoples (Keefe and Harvey, 2012; Shaw et al., 2000). Besides, the majority of the patients in the present study have studied up to secondary education level only. The low education level may limit their comprehension and ability to remember the drug name (Okuno et al., 1999).
Quality of life
The reduction of overall SDS score after 6 months of HMR follow up indicates improvement in the patients’ quality of life. Nevertheless, the statistical analysis showed no significant difference at each visit. This may be due to a relatively small number of patients included in the overall SDS score analysis. There were only 25 out of 133 patients (18.8%) who were employed and eligible to rate the three domains (work, social, and family) of the SDS. Previous studies from overseas also revealed that there was no significant impact on overall quality of life either on elderly or people with mentally ill after in-home pharmacist visit (Barker et al., 2012; Holland et al., 2005; Lenaghan et al., 2007; Sorensen et al., 2004). Barker et al. (2012) had highlighted no significant improvement in SF-36 scores between control and pharmacist-led home visit groups except for the physical functioning and mental health domains.
When analyzed by individual domain, there was a decreasing trend of the SDS score observed in “work”, “social,” and “family” components under the mildly impaired category (0–3) at each visit. This reflected that the patients were having recovery (Demyttenaere et al., 2001), better quality of life, and less health-related impairment in work, family, and social functioning. Nonetheless, the result for “work” component was not a significant difference at each time frame. This is because of the difficulty of the patients in getting a job and sustaining it. Besides, schizophrenia is a chronic disabling brain disorder which will affect the patient’s thoughts, emotions, and cognitive function. The deficiencies of these components can have great interferences on patient’s learning, work performance, and the ability to live independently (Keefe and Harvey, 2012). For patients who had achieved functional remission, ready and keen for work, they might not get an offer for employment due to the low acceptance and discrimination from the employer (Dahlan et al., 2014).
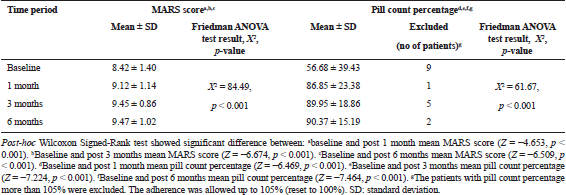 | Table 2. Comparison of MARS score and pill count percentage at baseline, 1-, 3-, and 6-month follow up. [Click here to view] |
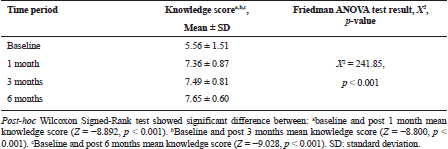 | Table 3. Comparison of medication knowledge score at baseline, 1-, 3-, and 6-month follow up. [Click here to view] |
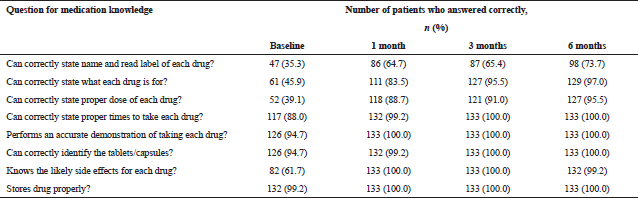 | Table 4. Number and percentage of patients who answered the medication knowledge questions correctly at baseline, 1-, 3-, and 6-month follow up. [Click here to view] |
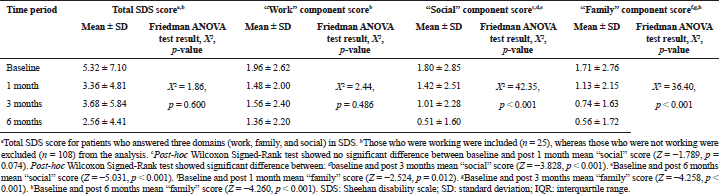 | Table 5. Comparison of SDS scores at baseline, 1-, 3-, and 6-month follow up. [Click here to view] |
The patients had a significant improvement for their quality of life in “family” component at each follow-up visit. The “social” component showed no significant improvement at 1 month follow-up but there was a significant improvement at the two subsequent visits. The result is in concordance with the study findings by Demyttenaere et al. (2001) which reported that the functioning improvement is ongoing over 6-month period. The improvement of the “social” component was more slowly as compared to other components. This might be due to the discrimination and stigmatization which caused them difficult to integrate into society in a short period of time (Chan and Yu, 2004).
LIMITATIONS
The present study was conducted without a control group. It is possible that a home visit itself has a positive effect on patients. Hence, the study design with lack of control group might result in positive findings, which might not have been as strong if a control group had been included.
CONCLUSION
Home medication review program conducted by the pharmacist has a positive impact on medication adherence, knowledge on antipsychotics, and quality of life among people with schizophrenia. This program should be implemented extensively throughout Malaysia in hospitals and clinics that provide psychiatric services for better patient’s care and quality of life.
ACKNOWLEDGMENTS
The authors would like to thank the Director of Health Malaysia for permission to publish this paper.
FINANCIAL SUPPORT
None.
CONFLICT OF INTEREST
Authors declare that there are no conflict of interest.
REFERENCES
Aziz SA. The first report of the National Mental Health Registry on schizophrenia. National Mental Health Registry, Department of Psychiatry and Mental Health, Hospital Kuala Lumpur, Kuala Lumpur, 2007 [Online]. Available via http://www.crc.gov.my/wp-content/uploads/documents/report/NMHR1stReport.pdf (Accessed 20 January 2015).
Barker A, Barlis P, Berlowitz D, Page K, Jackson B, Lim WK. Pharmacist directed home medication reviews in patients with chronic heart failure: a randomised clinical trial. Int J Cardiol, 2012; 159(2):139–43. CrossRef
Barkhof E, Meijer CJ, De Sonneville LM, Linszen DH, De Haan L. Interventions to improve adherence to antipsychotic medication in patients with schizophrenia—a review of the past decade. Eur Psychiatry, 2012; 27(1):9–18. CrossRef
Begley S, Livingstone C, Hodges N, Williamson V. Impact of domiciliary pharmacy visits on medication management in an elderly population. Int J Pharm Pract, 1997; 5(3):111–21. CrossRef
Bland JM, Butland BK, Peacock JL, Poloniecki J, Reid F, Sedgwick P. Statistic guide for research grant applicants. St George’s Hospital Medical School, London, UK, 2012 [Online]. Available via http://www-users.york.ac.uk/~mb55/guide/guide14.pdf (Accessed 20 January 2015).
Chan S, Yu IuW. Quality of life of clients with schizophrenia. J Adv Nurs, 2004; 45(1):72–83. CrossRef
Council of Europe CoM. Resolution ResAP (2001) 2 concerning the pharmacist's role in the framework of health security. Council of Europe, Strasbourg, 2001 [Online]. Available via https://wcd.coe.int/ViewDoc.jsp?id=193721&Site=CM (Accessed 20 January 2015).
Dahlan R, Midin M, Shah SA, Nik Jaafar NR, Abdul Rahman FN, Baharudin A, Das S, Sidi H. Functional remission and employment among patients with schizophrenia in Malaysia. Compr Psychiatry, 2014; 55(Suppl 1):S46–51. CrossRef
Demyttenaere K, Enzlin P, Dewe W, Boulanger B, De Bie J, De Troyer W, Mesters P. Compliance with antidepressants in a primary care setting, 2: the influence of gender and type of impairment. J Clin Psychiatry, 2001; 62(Suppl 22):34–7.
Family Health Department Division. Garispanduan pelaksanaan perkhidmatan pemulihan psikososial bagi pesakit mental di penjagaan kesihatan primer. Ministry of Health Malaysia, Kuala Lumpur, Malaysia, 2001.
Fenton WS, Blyler CR, Heinssen RK. Determinants of medication compliance in schizophrenia: empirical and clinical findings. Schizophr Bull, 1997; 23(4):637–51. CrossRef
Finley PR, Rens HR, Pont JT, Gess SL, Louie C, Bull SA, Bero LA. Impact of a collaborative pharmacy practice model on the treatment of depression in primary care. Am J Health Syst Pharm, 2002; 59(16):1518–26. CrossRef
Grymonpre RE, Didur CD, Montgomery PR, Sitar DS. Pill count, self report, and pharmacy claims data to measure medication adherence in the elderly. Ann Pharmacother, 1998; 32(7–8):749–54.
Haynes RB, Ackloo E, Sahota N, McDonald HP, Yao X. Interventions for enhancing medication adherence (review). Cochr Datab Syst Rev, 2008; 2:CD000011; doi: 10.1002/14651858.CD000011.pub3 CrossRef
Holland R, Desborough J, Goodyer L, Hall S, Wright D, Loke YK. Does pharmacist-led medication review help to reduce hospital admissions and deaths in older people? A systematic review and meta-analysis. Br J Clin Pharmacol, 2008; 65(3):303–16. CrossRef
Holland R, Lenaghan E, Harvey I, Smith R, Shepstone L, Lipp A, Christou M, Evans D, Hand C. Does home based medication review keep older people out of hospital? The HOMER randomised controlled trial. BMJ, 2005; 330(7486):293. CrossRef
Hussainy SY, Box M, Scholes S. Piloting the role of a pharmacist in a community palliative care multidisciplinary team: an Australian experience. BMC Palliat Care, 2011;10:16l doi: 10.1186/1472-684X-10-16 CrossRef
Keefe RS, Harvey PD. Cognitive impairment in Schizophrenia. Handb Exp Pharmacol, 2012; 213:11–37. CrossRef
Lenaghan E, Holland R, Brooks A. Home-based medication review in a high risk elderly population in primary care—the POLYMED randomised controlled trial. Age Ageing, 2007; 36(3):292–7. CrossRef
Lowe CJ, Raynor DK, Purvis J, Farrin A, Hudson J. Effects of a medicine review and education programme for older people in general practice. Br J Clin Pharmacol, 2000; 50(2):172–5. CrossRef
Ministry of Health Malaysia. Clinical practice guidelines: management of schizophrenia in adults. Ministry of Health Malaysia, Putrajaya, 2009 [Online]. Available via http://www.acadmed.org.my/index.cfm?&menuid=67 (Accessed 10 August 2015).
Mustapa MD, Wong YC, Thiruvanackan K. Improving patients' medication compliance and treatment outcome through Home Medication Review (HMR) conducted by pharmacists at primary health clinics in the state of Selangor. Paper presented at 5th National Pharmacy R&D Conference, Hospital Putrajaya, Putrajaya, Malaysia, July 28–30, 2008.
Naunton M, Peterson GM. Evaluation of home-based follow-up of high-risk elderly patients discharged from hospital. J Pharm Pract Res, 2003; 33(3):176–82. CrossRef
Okuno J, Yanagi H, Tomura S, Oka M, Hara S, Hirano C, Tsuchiya S. Compliance and medicartion knowledge among elderly Japanese home-care recipients. Eur J Clin Pharmacol, 1999; 55(2):145–9. CrossRef
Raynor DK, Nicolson M, Nunney J, Petty D, Vail A, Davies L. The development and evaluation of an extended adherence support programme by community pharmacists for elderly patients at home. Int J Pharm Pract, 2000; 8(3):157–64. CrossRef
Shaw H, Mackie CA, Sharkie I. Evaluation of effect of pharmacy discharge planning on medication problems experienced by discharged acute admission mental health patients. Int J Pharm Pract, 2000; 8(2):144–53. CrossRef
Sheehan DV, Harnett-Sheehan K, Raj BA. The measurement of disability. Int Clin Psychopharmacol, 1996; 11(Suppl 3):89–95. CrossRef
Sorensen L, Stokes JA, Purdie DM, Woodward M, Elliott R, Roberts MS. Medication reviews in the community: results of a randomized, controlled effectiveness trial. Br J Clin Pharmacol, 2004; 58(6):648–64. CrossRef
Thompson K, Kulkarni J, Sergejew AA. Reliability and validity of a new Medication Adherence Rating Scale (MARS) for the psychoses. Schizophr Res, 2000; 42(3):241–7. CrossRef
Weiden PJ, Dixon L, Frances A. Neuroleptic noncompliance in schizophrenia. In: Tamminga CA, Schulz SC (eds.). Schizophrenia research. Raven Press, New York, pp. 285–96, 1991.
World Health Organization. The role of the pharmacist in the health care system. World Health Organization, Geneva, Switzertland, 1994 [Online]. Available via http://apps.who.int/medicinedocs/pdf/h2995e/h2995e.pdf (Accessed 20 January 2015).
World Health Organization. Improving access and use of psychotropic medicines. World Health Organization, Geneva, Switzerland, 2005 [Online]. Available via http://www.who.int/mental_health/policy/services/10_improving%20access_WEB_07.pdf?ua=1 (Accessed 20 January 2015).
Xiang YT, Weng YZ, Leung CM, Tang WK, Ungvari GS. Quality of life of Chinese schizophrenia outpatients in Hong Kong: relationship to sociodemographic factors and symptomatology. Aust N Z J Psychiatry, 2007; 41(5):442–9. CrossRef
Young JL, Zonana HV, Shepler L. Medication noncompliance in schizophrenia: codification and update. Bull Am Acad Psychiatry Law, 1986; 14(2):105–22.