INTRODUCTION
Globally, immunization rates among adults dropping below the desired targets remain a significant public health concern. The rising threat of vaccine-preventable diseases and the underutilization of the immunization service in Malaysia remain a concern. According to the National Health and Morbidity Survey 2016, there were an increasing number of parents who chose not to vaccinate their children, with 637 cases in 2013 and 1,603 cases in 2016 (Panting, 2018) and with only 86.4% of children in Malaysia completing immunization coverage (Musa et al., 2019), which was below the recommended coverage rate of 92%–95% (Tannous et al., 2014). In addition, it was reported by the Ministry of Health (MoH) that the number of measles cases in Malaysia had risen from 195 cases in 2013 to 1,934 cases in 2018 and this showed about a 900% increase over 5 years (WHO, 2019). Various factors contributed to underutilized vaccination services in Malaysia, such as low awareness about vaccination and its benefits, concern about its side effects, and preference for alternative medicine (Wan Taib et al., 2017).
In 2019, the Malaysian Pharmaceutical Society (MPS) had proposed to include pharmacists to provide vaccination service in response to the failure to attain the target of the Measles Elimination Program in 2018. MPS believed that this action might help in expanding the public’s accessibility to get their vaccine shot (Soon, 2019) and combating vaccine hesitancy which had been listed by the World Health Organization (WHO) as one of the top 10 threats worldwide in 2019 (WHO, 2019). However, the request from MPS was disregarded by the Malaysian Medical Association (MMA), emphasizing that there had been more than enough highly trained and experienced personnel to provide the vaccination service and pharmacists were not as well trained to give injections which would otherwise increase patients’ risk of getting infections (Annuar, 2019).
In Malaysia, community pharmacists (CPs) are not certified healthcare providers in delivering vaccination services. However, they played an important role in educating the public on the importance of vaccination and might also get involved in reviewing patients’ history and screening for patients who required vaccination (Allela, 2018). Vaccination services in Malaysia are mainly delivered by doctors through government and private hospitals and primary health clinics.
Vaccination provided by CPs was not new; it has been practiced in many countries such as Australia, Canada, New Zealand, the Philippines, the United Kingdom, and the United States (Rosado et al., 2016). The literature showed that allowing CPs to become vaccinators contributed to various benefits such as improving the public’s accessibility to vaccination service (Gerges et al., 2018; Goad et al., 2013b; Papastergiou et al., 2014), improving vaccination coverage rate (Drozd et al., 2017; Hattingh et al., 2016; Isenor et al., 2018b; Loughlin et al., 2007; Schwerzmann et al., 2017; Usami et al., 2009; Wang et al., 2013), increasing the cost-effectiveness of vaccines (Prosser et al., 2008; Singhal and Zhang, 2014), raising the awareness toward the importance of vaccination and dispelling the myths about vaccination (Goad, 2013a; Papastergiou et al., 2014), providing patients with reminders to ensure they get the subsequent doses of vaccines (Warner et al., 2013), and establishing collaboration with physicians (Blake et al., 2003; Hurley et al., 2011; Hurley et al., 2014; Welch et al., 2005). From the perspective of the public, there is a high level of satisfaction toward such service provided by community pharmacies due to factors such as long operating hours, strategic location, less waiting time, and availability of appointment booking provided by community pharmacies, which enhances their accessibility and convenience (Goad et al., 2013b; Pilisuk et al., 2010; Poulose et al., 2015; Warner et al., 2013).
Community pharmacy-based vaccination services provided by CPs show numerous benefits including immunization education and provide a convenient and accessible option for the general public for receiving the immunization. There are many examples of CPs serving in these vaccinator roles with successful outcomes (Table 1).
It was unknown when such service would be implemented in Malaysia as authorizing CPs to become vaccinators was a controversial issue. Furthermore, CPs’ willingness to expand their practice had not been discovered in Malaysia.
This study aimed to investigate the CPs’ knowledge toward vaccination and their willingness to implement the community pharmacy-based vaccination service in Malaysia.
METHODOLOGY
Study design and setting
A cross-sectional study was conducted among CPs using a validated, self-administered questionnaire in the state of Selangor, Malaysia, from February to May 2020.
Participants and sample size calculation
A list of the total number of community pharmacies in the state of Selangor was retrieved from the website of the Pharmaceutical Service Division, MoH, Malaysia. There were 1,394 registered community pharmacies identified in the state of Selangor. We used Google Earth to locate pharmacies in 15 subdistricts and selected the community pharmacies based on ease of access to obtain a minimum of two community pharmacies from each subdistrict. Accordingly, there were a total of 427 community pharmacies spread across 15 subdistricts. According to an analysis report published by the MPS, the number of CPs who were practicing in Selangor and owned Type A licenses as of December 2018 was 910 (Tan, 2019). In this study, the sampling unit was CPs. Consequently, we invited only one pharmacist from pharmacies with more than one pharmacist. With a 5% margin of error, 95% confidence level, and 50% response distribution, the recommended sample size was 203 community pharmacies as calculated by the Raosoft calculator (Raosoft, 2004).
Inclusion and exclusion criteria
Only those pharmacists who met the inclusion criteria (Malaysian CP with Type A license practicing in Selangor, Malaysia, either as part-time, full-time or locum, and fully registered with the Malaysian Pharmacy Board) were enrolled. Both genders were included. Pharmacists who did not meet the inclusion criteria were excluded from this study.
Questionnaire development
The questionnaire was adopted from Edwards et al. (2015) and modified to suit the Malaysian population. The questionnaire consisted of 51 questions and was divided into 6 sections. In section A, pharmacists’ sociodemographics (gender, age, area of practice, highest pharmacy qualification, job title, years of practice, and pharmacy setting) were recorded. Section B was about the knowledge toward the vaccination. CPs were asked to select one option from “true,” “false,” and “don’t know” for each statement. Correct responses were scored as one (1) while incorrect and “don’t know” responses were scored as zero (0). The scores for each respondent were summed up. A score of 50% or less (scores of 6 or less) was categorized as having a low knowledge level toward vaccination, those who scored 51%–74% (scores of 7–10) were categorized as “moderate level,” and those who scored 75% and above (scores of 11 and above) were categorized as having a good knowledge level toward vaccination. Section C assessed CPs’ awareness toward community pharmacy-based vaccination programs in other countries. In section D, the attitude of CPs toward the implementation of a community pharmacy-based vaccination program in Malaysia was evaluated by using a 5-point Likert scale of “strongly agree” to “strongly disagree.” For positive statements, “strongly disagree,” “disagree,” “neutral,” “agree,” and “strongly agree” responses were given one (1), two (2), three (3), four (4), and five (5) marks, respectively. Reverse scoring was carried out to negative statements. A higher score indicated a better attitude toward the implementation of immunization services. Meanwhile, the last section, section E, also used a 5-point Likert scale to address the key perceived barriers according to the percentage of CPs agreeing on statements.
Reliability and validity of the questionnaire
A pilot study was conducted with 35 CPs before data collection. Cronbach’s alpha value obtained in the pilot test was 0.692, which was considered acceptable as it was very close to the recommended cutoff value of 0.7 (Taber, 2018).
The questionnaire used in this study was validated by nine CPs. The means of the item-content validity index (I-CVI) and scale-content validity index (S-CVI) were both found to be 0.91, and this result ensured the content validity of the questionnaire (Rodrigues et al., 2017).
Data collection
Community pharmacies were approached by the principal investigator who invited the pharmacists to participate in the study. Before filling out the questionnaire, respondents were provided with an information sheet and consent form. Self-administered paper-based questionnaires were distributed to CPs by using the drop-off and pick-up method and collected back after 2 weeks. Upon completion, the questionnaire was checked for any missed response. In the case where a missed response was detected, the participants were requested to fill in the missing response. Participation in this study was voluntary.
Data analysis
All data were analyzed descriptively and inferentially by using IBM Statistical Package for the Social Sciences (SPSS®) statistics for Windows, version 22.0. Independent t-test and one-way analysis of variance (ANOVA) test were used to analyze the differences between mean knowledge and attitude scores across various sociodemographics. Pearson’s correlation coefficient analysis was conducted to measure the relationship between knowledge and attitude score, and these correlations were categorized into weak (r = 0.10–0.29), moderate (r = 0.30–0.49), and strong (r = 0.5–1) correlations as suggested by Cohen et al (2002). A p-value of <0.05 was considered statistically significant.
Ethical approval
The study received ethical approval from the Research Management Centre, MAHSA University (RMC/EC22/2020). Written consent was taken from each respondent before participation in the study. Confidentiality and anonymity of all respondents were maintained as no names were mentioned in the questionnaires.
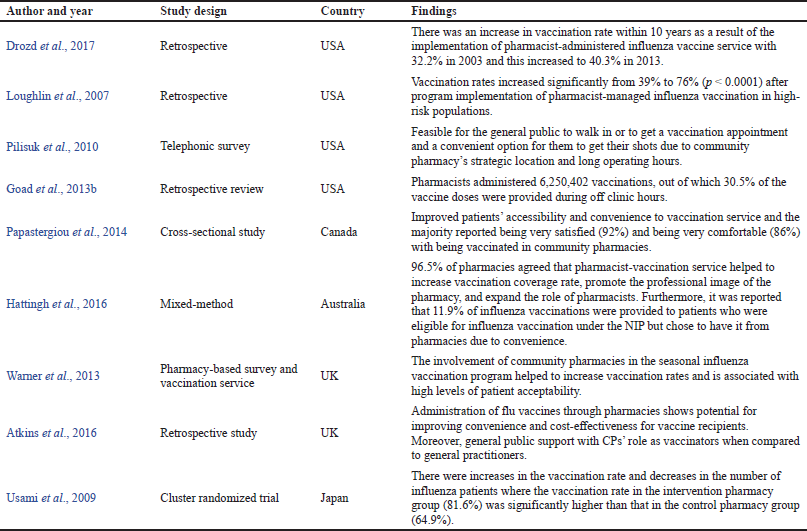 | Table 1. Benefits of community pharmacy-based vaccination: pharmacist as a vaccinator. [Click here to view] |
RESULTS
Sociodemographic data of the respondents
A total of 270 community pharmacies were approached. Only 218 pharmacists gave consent to participate in the study with a response rate of 80.7% (218/270). The majority of the respondents were female (n = 130; 59.6%) and Chinese (n = 151; 69.3%) with age between 20 and 29 years (n = 119; 54.6%). Most of them have bachelor’s degrees (n = 185; 84.9%) as the highest pharmacy qualification with a duration of experience of 1–5 years (n = 108; 49.5%). Most of the community pharmacies were chain pharmacies (n = 132; 60.6%), followed by independent retail pharmacies (n = 86; 39.4%). The summary of the sociodemographic data is presented in Table 2.
Awareness toward a community pharmacy-based vaccination program
More than half of the pharmacists (58.3%) were aware of MPS both proposing to involve pharmacists in delivering vaccination services and that CPs in some other countries were allowed and certified to administer vaccinations. When CPs were asked on which countries had their CPs certified in delivering vaccination that they were aware of, the United Kingdom had the highest responses (36.7%), followed by Australia (33.9%), the United States (33.5%), New Zealand (17.4%), Canada (14.7%), the Philippines (5.5%), and Japan (2.3%) (Table 3).
Attitude toward the implementation of a community pharmacy-based vaccination program
The majority of the CPs agreed that the proportion of the population receiving immunizations would increase if CPs were permitted and trained to provide vaccination (88.6%) and the accessibility of the public to immunization service would be improved (84.4%). However, it was found that more than half of the CPs (55.5%) disagreed that CPs have received an adequate amount of training and learning on vaccination topics during their pharmacy studies. There was a greater number of CPs (62.8%) who believed that CPs should be permitted to expand their practice (62.8%) and there should be formal certification (87.1%). In addition, 36.7% of the CPs had a neutral attitude regarding the administration of vaccines as an easily learned technical skill. Moreover, it was demonstrated that a majority of CPs (87.2%) believed that they required additional learning and training before they could administer vaccines safely. A favorable attitude was also shown as there was only a minority of CPs (6%) who disagreed that the public would feel comfortable if CPs were vaccinators. However, a majority of CPs (78.5%) were not confident that they would be comfortable in providing vaccination even if they did not receive additional training and education. There were almost equal numbers of CPs who either agreed (36.7%) or were neutral (35.8%) regarding the improvement of the relationship between CPs and other vaccine providers, such as physicians. In addition, more than half of the CPs expressed their willingness to provide vaccination to the public (69.3%) and believed that the benefits outweighed the drawbacks if CPs were permitted to provide vaccination (66.5%). Table 4 summarizes the responses on the attitude toward the implementation of a community pharmacy-based vaccination program.
 | Table 2. Sociodemographic data of the respondents (n = 218). [Click here to view] |
Perception toward the implementation of a community pharmacy-based vaccination program
Eight key perceived barriers were identified. The major perceived barrier was the inadequate level of training by CPs to administer vaccines (89.9%). Lack of support from the authorities (79.4%), resources cost (77.1%), the level of knowledge toward vaccination (76.6%), vaccination record practice (74.3%), the amount of time and effort for vaccination training and development (73.4%), concern for public’s safety (70.2%), and lack of support from other vaccine providers (69.3%) were also found to be the main perceived barriers. Table 5 summarizes the responses on the perceived barriers toward the implementation of a community pharmacy-based vaccination program.
 | Table 3. Responses to the awareness toward a community pharmacy-based vaccination program. [Click here to view] |
 | Table 4. Responses to the attitude toward the implementation of a community pharmacy-based vaccination program. [Click here to view] |
Knowledge toward vaccination and their attitude toward the implementation of a community pharmacy-based vaccination program
The findings from the current study show that half of the participating CPs (50%) in this study had a moderate level of knowledge toward vaccination. Furthermore, almost all the CPs (95.5%) had a good attitude toward the implementation of a community pharmacy-based vaccination program in Malaysia (Table 6).
Difference between sociodemographics with knowledge and attitude level
Based on Table 6, there was a significant difference in the knowledge score based on the highest pharmacy education (p = 0.01) where CPs with master’s degrees had a significantly higher knowledge level when compared to CPs with bachelor’s degrees. In addition to that, there was a significant difference in the attitude score based on the highest pharmacy education (p = 0.037) where CPs with master’s degrees had a significantly better attitude when compared to CPs with bachelor’s degrees.
Correlation between knowledge and attitude level
The attitude of CPs toward the implementation of a community pharmacy-based vaccination program was found to be weak but significantly positively correlated with their knowledge toward vaccination (r = 0.209, n = 218, p = 0.002) (Table 7).
DISCUSSION
Knowledge toward vaccination
This study assesses the CPs’ knowledge toward the vaccination and their attitude and perception in the implementation of vaccination service in community pharmacy. It has been reported that a low level of knowledge regarding immunization led to a reluctance to receive vaccination (Abdullah et al., 2016; Azhar et al., 2012; Panting, 2018). CPs’ knowledge on immunization was crucial as CPs had the task to educate the public regarding immunization, and a higher level of knowledge could help in facilitating this role and improving the immunization coverage of the nation (Della Polla et al., 2020). Studies have proved that educational intervention helped to improve public knowledge and change their perception toward vaccines (Awadh et al., 2014; Tony et al., 2014). This was supported by two studies, which revealed a positive correlation between knowledge level and intention to provide pharmacy-based vaccination service (Luthin et al., 2011; Ongpoy, 2017).
Attitude toward the implementation of a community pharmacy-based vaccination program
In our study, the majority of CPs (>80%) agreed that CPs could help in improving vaccination coverage and the public’s accessibility to get their vaccination. The literature had abundant data that proved that as vaccine providers CPs improved the vaccination coverage rate and the expanded accessibility toward vaccination, and this contributed to the increase in vaccination rate (Drozd et al., 2017; Isenor et al., 2018a; Loughlin et al., 2007; Schwerzmann et al., 2017; Usami et al., 2009; Wang et al., 2013). With the overloaded MoH’s public clinic, the public might seek places which were more convenient and accessible. Accessibility was the key determinant factor for patients to choose a community pharmacy as the site of vaccination, and this factor of convenience was reported in other studies (Gerges et al., 2018; Papastergiou et al., 2014).
The findings from the current study also revealed that more than half of the CPs disagreed that they had an adequate amount of education and training (55.5%) and they were well prepared for the provision of vaccination service (78.5%) which was in line with Edwards et al.’s (2015) study where 59% of their CPs responded the same way. Hence, to implement such service in Malaysia, CPs would need to be trained to become proficient in administering vaccination. Various immunization training programs had been implemented in Canada showing positive results as 97% of the participating pharmacists expressed more preparedness to provide such vaccination service (Edwards et al., 2015).
Moreover, this study showed a greater number of CPs (62.8%) believed that they should be permitted to expand their practice. This result was almost similar to Edwards et al. (2015) where 68% of their CPs responded the same way. The reason CPs looked for expanding their roles could be due to their existence in the community, the trust placed in them by the community, their communication skills, their experience in handling different types of patients, and their knowledge of preventive care (Alsabbagh et al., 2018). In addition, the majority of the CPs in our study was shown to be more neutral toward the idea that vaccination administration could be easily learned. The literature shows that CPs are capable of learning and providing safe vaccines administration. During a 2-month period of time, newly trained CPs had administered a total of 343 doses of vaccines, and no adverse events were reported (Ernst et al., 1997). From the perspective of patients, two studies had revealed that patients were satisfied with CPs’ injection technique (Papastergiou et al., 2014; Poulose et al., 2015).
There were almost equal numbers of CPs who either agreed (36.7%) or were neutral (35.8%) regarding the improvement of the relationship between CPs and other vaccine providers. One study had shown that most physicians agreed that it was helpful to have pharmacists share the role of vaccinators (Hurley et al., 2014). However, it was also found that GPs were less supportive with pharmacists taking on the role of vaccinators due to the concern of reduced healthcare quality, the safety of vaccine recipients, pharmacists’ financial losses (Atkins et al., 2016), and ineffective documentation (Orenstein and Schaffner, 2008).
In terms of willingness, 69.3% of the CPs in our study expressed their willingness to provide vaccination service if they were permitted to. This result was similar to a study conducted in Saudi Arabia where 55% of the CPs expressed their willingness to provide vaccination service and the remaining 45% of CPs expressed their concern about patients’ safety and their inadequate amount of training in vaccination practice (Balkhi et al., 2018). A study had found that CPs who participated in immunization-related educational programs expressed a greater willingness to provide immunization-related activities (Madhavan et al., 2001). As this study found a greater percentage of CPs with the willingness to provide vaccination (69.3%), it could be due to the current coronavirus disease 2019 (COVID-19) pandemic that, as the frontliners, CPs might feel that they had greater responsibility in contributing to public health.
The current study also found that the highest pharmacy education degree had a significant difference with the attitude of the CPs. Moreover, CPs’ knowledge toward vaccination had a significant positive correlation with their attitude in the implementation of community-based vaccination service. These results were in line with a previous study where a significant positive correlation with the level of preparedness to provide vaccination service and pharmacy education was found where those who completed the master’s or Ph.D. program expressed greater preparedness (Ongpoy, 2017). In addition, a similar positive correlation was also found between pharmacy students’ intention to provide pharmacy-based immunization service and their knowledge score (Luthin et al., 2011).
 | Table 5. Perceived barriers toward implementation of a community pharmacy-based vaccination program. [Click here to view] |
 | Table 6. Level of knowledge toward vaccination and their attitude toward the implementation of a community pharmacy-based vaccination program in Malaysia. [Click here to view] |
Perceived barriers toward implementation of community pharmacy-based vaccination program
Among the perceived barriers, the four most common barriers toward the vaccination services perceived by CPs were “inadequate level of training,” “lack of support from the authorities,” “resources cost,” and “lack of knowledge on vaccination topic.”
An inadequate level of training was perceived as an important barrier. The literature shows that CPs who did not undergo training were more likely to report a lack of training as a barrier (Kummer and Foushee, 2008) and there should be continuous training and education for implementing a community pharmacy-based vaccination program (Balkhi et al., 2018; Valiquette and Bédard, 2015).
Lack of support from the authorities was the second top perceived barrier (79.4%). MPS’s proposal to include pharmacists for the provision of vaccination service was not approved by MoH (Pearl, 2019). In 2016, FIP published a global report and pointed out that there were 13 countries that already had authorized CPs as vaccinators which included Argentina, Australia, Canada, Costa Rica, Denmark, Ireland, New Zealand, the Philippines, Portugal, South Africa, Switzerland, the UK, and the USA (Rosado et al., 2016). These countries had acknowledged the potential benefit of allowing pharmacists to provide vaccine service to the community.
Resources cost was the top third perceived barrier (77.1%). Several studies had identified lack of reimbursement as a barrier (Edwards et al., 2015; Hastings et al., 2017; Kamal et al., 2003; Kummer and Foushee, 2008; Westrick et al., 2018). This barrier can be addressed by adequate reimbursement. In the United States, pharmacists obtained reimbursement from Medicare under the current fee schedule (Hartzell, 2017), whereas, in Ontario, an amount of $7.50 would be reimbursed by the government for the administration cost of each vaccine injection (Ministry of Health, 2015).
 | Table 7. Differences between mean knowledge and attitude score across various sociodemographics and correlation with knowledge and attitude score (n = 218). [Click here to view] |
Lack of knowledge on vaccination topics was another perceived barrier (76.6%). The literature shows a positive correlation between knowledge level and CPs’ intention to provide vaccination service (Luthin et al., 2011; Ongpoy, 2017). Thus, this suggests knowledge level needs to be improved before implementing such service in Malaysia. Pharmacists in Saudi Arabia had not been granted the authority to administer vaccination; the majority of them (95.2%) reported that continuous professional education is an important factor for the implementation of CPs administered vaccination service (Balkhi et al., 2018).
Record practices associated with vaccination were perceived as barriers (74.3%). Documentation was an important component in the process of immunization. It was reported that a minority of pharmacists document the information following the vaccination process into the regional immunization registry (Westrick et al., 2018) and GPs were concerned with the probability of incomplete documentation of patient data by pharmacists (Atkins et al., 2016; MacDougall et al., 2016; Orenstein and Schaffner, 2008). The amount of time and effort associated with vaccination training was perceived as a barrier (73.4%). This perceived barrier was a concern to CPs as they were concerned about the lack of time for patient care after incorporating immunization practice, especially for chain pharmacies where there are a huge number of dispensing activities per day and the profitability depends on the prescription volume (Madhavan et al., 2001).
Concern for public safety was another main perceived barrier (70.2%). An association was found between the level of comfort in providing vaccination and the level of training (Akala and Powers, 2005); thus, training should be provided before CPs provide vaccination. The literature shows that CPs who were trained were capable of providing safe vaccine administration with only 3 cases of adverse events reported from 100,000 doses of vaccine administered (Capurso and Powers, 2006). Lack of support from other vaccine providers was perceived as a barrier (69.3%). In Malaysia, the proposal to include pharmacists as vaccinators was refused by MMA stating that pharmacists were not well trained (Annuar, 2019). A similar case was shown in Australia (Haggan, 2018) and Canada (MacDougall et al., 2016). The reduction of income sources was the reason for GPs’ opposition in the UK (Francis and Hinchliffe, 2010).
Study limitation
This study has some limitations. First, the study location was one of the limitations as this study was only conducted in 15 areas in Selangor; hence, the study design was a cross-sectional survey. Thus, the findings might be difficult to be generalized to all of Selangor’s CPs. Second, the COVID-19 pandemic had limited the data collection process, hence yielding a smaller number of respondents. Third, our study was conducted at a specified time. Last, bias from the respondents when answering the questionnaires was also possible due to their busy workload in the community pharmacy during the COVID-19 pandemic. Although the findings from this study did not represent the data of the whole country, it could serve as a baseline study for future larger studies to investigate CPs’ willingness and acceptability for the provision of community-based vaccination service before implementing such service in Malaysia.
CONCLUSION
The majority of the CPs had a moderate knowledge toward vaccination. Most of them had a positive attitude in the implementation of community-based immunization service which could help to improve the coverage rate of the nation, improving the public’s accessibility and resilience to the public health system. CPs can also provide additional services such as vaccination information, vaccination reminders, and identification of the high-risk group. Seven out of 10 CPs expressed their willingness to provide vaccination service. Government and policymakers may consider reforming the national immunization program (NIP) to include pharmacists as vaccination providers. The perceived barriers should be addressed before the expansion of CPs’ roles as vaccinators for successful vaccination services in Malaysia.
ACKNOWLEDGMENT
The authors would like to thank the community pharmacists who participated in this research and the authors who permitted them to use the questionnaire.
CONFLICT OF INTEREST
The authors declared no potential conflicts of interest.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to the conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agreed to be accountable for all aspects of the work. All the authors are eligible to be authors as per the International Committee of Medical Journal Editors (ICMJE) requirements/guidelines.
FUNDING
There is no funding to report.
ETHICAL APPROVALS
This study does not involve experiments on animals or human subjects.
DATA AVAILABILITY
All data generated and analyzed are included within this research article.
PUBLISHER’S NOTE
This journal remains neutral with regard to jurisdictional claims in published institutional affiliation.
REFERENCES
Abdullah AC, MZ NA, Rosliza AM. Practice of childhood immunizations among parents and their associated factors in Hulu Langat, Selangor, Malaysia. Int J Public Health Clin Sci, 2016; 3(6):94–104.
Akala FO, Powers MF. Understanding the perceptions and attitudes of pharmacy students on administering adult vaccines. J Pharm Technol, 2005; 21(5):254–7; http/doi.org/10.1177/875512250502100503 CrossRef
Allela OQB. Knowledge and attitude of immunization among IIUM pharmacy students. J Basic Clin Pharm, 2018; 8(October):65–9.
Alsabbagh MW, Wenger L, Raman-Wilms L, Schneider E, Church D, Waite N. Pharmacists as immunizers, their pharmacies and immunization services?: a survey of Ontario community pharmacists. Can Pharm J, 2018; 151(4):263–73; http/doi.org/10.1177/1715163518779095 CrossRef
Annuar A. ‘Counter-productive’ for pharmacists to administer vaccines, doctors’ body says, 2019. Available from https://www.malaymail.com/news/malaysia/2019/02/25/counter-productive-for-pharmacists-to-administer-vaccines-doctors-body-says/1726723 (Accessed 8 November 2019)
Atkins K, van Hoek AJ, Watson C, Baguelin M, Choga L, Patel A, Raj T, Jit M, Griffiths U. Seasonal influenza vaccination delivery through community pharmacists in England: evaluation of the London pilot. BMJ Open, 2016; 6(2):1–11; http/doi.org/10.1136/bmjopen-2015-009739 CrossRef
Awadh AI, Hassali MA, Al-Lela OQ, Bux SH, Elkalmi RM, Hadi H. Does an educational intervention improve parents ’ knowledge about immunization?? Experience from Malaysia. BMC Pediatr, 2014; 14(1):254; http/doi.org/10.1186/1471-2431-14-254 CrossRef
Azhar SS, Nirmal K, Nazarudin S, Rohaizat H, Noor AA, Rozita H. Factors influencing childhood immunization defaulters in Sabah, Malaysia. Int Med J Malaysia, 2012; 11(1):17–22. CrossRef
Balkhi B, Aljadhey H, Mahmoud MA, Alrasheed M, Pont LG, Mekonnen AB, Alhawassi TM. Readiness and willingness to provide immunization services: a survey of community pharmacists in Riyadh, Saudi Arabia. Safety Health, 2018; 4(1); http/doi.org/10.1186/s40886-018-0068-y CrossRef
Blake EW, Blair MM, Couchenour RL. Perceptions of pharmacists as providers of immunizations for adult patients. Pharmacotherapy, 2003; 23(2):248–54: http/doi.org/10.1592/phco.23.2.248.32083. CrossRef
Capurso KA, Powers MF. Barriers to implementing a pharmacist-run immunization service, as perceived by pharmacists, in a community pharmacy chain. J Pharm Technol, 2006; 22(2):91–4; http/doi.org/10.1177/875512250602200204 CrossRef
Cohen, J., Cohen, P., West, S.G., & Aiken, L.S. (2002). Applied Multiple Regression/Correlation Analysis for the Behavioral Sciences (3rd ed.). Routledge. https://doi.org/10.4324/9780203774441
Della Polla G, Napolitano F, Pelullo CP, De Simone C, Lambiase C, Angelillo IF. Investigating knowledge, attitudes, and practices regarding vaccinations of community pharmacists in Italy. Hum Vacc Immunother, 16(10):2422–28. https://doi.org/10.1080/21645515.2020.1720441 CrossRef
Drozd EM, Miller L, Johnsrud M. Impact of pharmacist immunization authority on seasonal influenza immunization rates across states. Clin Ther, 2017; 39(8):1563–80.e17; http/doi.org/10.1016/j.clinthera.2017.07.004 CrossRef
Edwards N, Gorman Corsten E, Kiberd M, Bowles S, Isenor J, Slayter K, McNeil S. Pharmacists as immunizers: a survey of community pharmacists’ willingness to administer adult immunizations. Int J Clin Pharm, 32015; 7(2):292–5; http/doi.org/10.1007/s11096-015-0073-8 CrossRef
Ernst ME, Chalstrom CV, Currie JD, Sorofman B. Implementation of a community pharmacy-based influenza vaccination program. J Am Pharm Assoc, 1997; 37(5):570–80; http/doi.org/10.1016/S1086-5802(16)30253-4 CrossRef
Francis M, Hinchliffe A. Vaccination services through community pharmacy: a literature review. Public Health Wales NHS Trust, Wales, UK, 2010.
Gerges S, Peter E, Bowles SK, Diamond S, Bucci LM, Resnick A, Taddio A. Pharmacists as vaccinators: an analysis of their experiences and perceptions of their new role. Hum Vacc Immunother, 2018; 14(2):471–7; http/doi.org/10.1080/21645515.2017.1403695 CrossRef
Goad JDM. The anti-vaccine movement: a pharmacist’s view. In: Chatterjee A (ed.). Vaccinophobia and vaccine controversies of the 21st century, Springer, New York, NY, 2013a. CrossRef
Goad JA, Taitel MS, Fensterheim LE, Cannon AE. Vaccinations administered during off-clinic hours at a national community pharmacy: implications for increasing patient access and convenience. Ann Fam Med, 2013b; 11(5):429–36; http/doi.org/10.1370/afm.1542 CrossRef
Haggan M. Ama vaccination attitude ‘infuriating,’ 2018. Available from https://ajp.com.au/news/ama-vaccination-attitude-infuriating/ (Accessed 17 June 2020)
Hartzell VA. Reimbursement for service of administering vaccines, from an independent pharmacy perspective, 2017. Available from https://www.pharmacytimes.com/publications/supplementals/2017/ImmunizationSupplementJune2017/reimbursement-for-service-of-administering-vaccines-from-an-independent-pharmacy-perspective (Accessed 18 June 2020)
Hastings TJ, Hohmann LA, McFarland SJ, Teeter BS, Westrick SC. Pharmacists’ attitudes and perceived barriers to human papillomavirus (hpv) vaccination services. Pharmacy, 2017; 5(4):45; http/doi.org/10.3390/pharmacy5030045 CrossRef
Hattingh HL, Sim TF, Parsons R, Czarniak P, Vickery A, Ayadurai S. Evaluation of the first pharmacist-administered vaccinations in Western Australia: a mixed-methods study. BMJ Open, 2016; 6(9):e011948; http/doi.org/10.1136/bmjopen-2016-011948 CrossRef
Hurley LP, Wortley P, Allison MA, O’Leary S, Daley MF, Babbel C, Crane LA, Stokley S, Beaty B, Dickinson LM, Kempe A. Seasonal influenza vaccination in adults: practice and attitudes about collaborative delivery with community vaccinators. Vaccine, 2011; 29(47):8649–55; http/doi.org/10.1016/j.vaccine.2011.08.126 CrossRef
Hurley LP, Bridges CB, Harpaz R, Allison MA, O’Leary ST, Crane LA, Brtnikova M, Stokley S, Beaty BL, Jimenez-Zambrano A, Ahmed F, Hales C, Kempe A. U.S. physicians’ perspective of adult vaccine delivery. Ann Intern Med, 2014; 160(3):161–71; http/doi.org/10.7326/M13-2332 CrossRef
Isenor JE, O’Reilly BA, Bowles SK. Evaluation of the impact of immunization policies, including the addition of pharmacists as immunizers, on influenza vaccination coverage in Nova Scotia, Canada?: 2006 to 2016. BMC Public Health, 2018a; 18(1):1–8; http/doi.org/10.1186/s12889-018-5697-x CrossRef
Isenor JE, Slayter KL, Halperin DM, Mcneil SA, Bowles SK. Pharmacists’ immunization experiences, beliefs, and attitudes in New Brunswick, Canada. Pharm Pract, 2018b; 16(4):1–7; http/doi.org/10.18549/PharmPract.2018.04.1310 CrossRef
Kamal KM, Madhavan SS, Maine LL. Pharmacy and immunization services: Pharmacists’ participation and impact. J Am Pharma Assoc, 2003; 43(4):470–82; http/doi.org/10.1331/154434503322226211 CrossRef
Kummer GL, Foushee LL. Description of the characteristics of pharmacist-based immunization services in North Carolina: results of a pharmacist survey. J Am Pharma Assoc, 2008; 48(6):744–51; http/doi.org/10.1331/JAPhA.2008.07080 CrossRef
Loughlin SM, Mortazavi A, Garey KW, Rice GK, Birtcher KK. Pharmacist-managed vaccination program increased influenza vaccination rates in cardiovascular patients enrolled in a secondary prevention lipid clinic. Pharmacotherapy, 2007; 27(5):729–33; http/doi.org/10.1592/phco.27.5.729 CrossRef
Luthin DR, King SR, Wensel TM, Rosser AN, Monk-Tutor MR. Relationship between pharmacy students’ knowledge about, attitudes toward, and intention to provide pharmacy-based immunization services. Curr Pharm Teach Learn, 2011; 3(3):171–7; http/doi.org/10.1016/j.cptl.2011.04.007 CrossRef
MacDougall D, Halperin BA, Isenor J, MacKinnon-Cameron D, Li L, McNeil SA, Langley JM, Halperin SA. Routine immunization of adults by pharmacists: attitudes and beliefs of the Canadian public and health care providers. Hum Vacc Immunother, 2016; 12(3):623–31; http/doi.org/10.1080/21645515.2015.1093714 CrossRef
Madhavan SS, Rosenbluth SA, Amonkar M, Borker RD, Richards T. Pharmacists and immunizations?: a national survey. J Am Pharma Assoc, 2001; 41(1):32–45; http/doi.org/10.1016/S1086-5802(16)31203-7 CrossRef
Ministry of Health. Pharmacist administration of publicly funded influenza vaccine and claims submission using the health network system, 2015. Available from http://www.health.gov.on.ca/en/pro/programs/drugs/opdp_eo/notices/eo_flu_mist_20151013.pdf
Musa AF, Soni T, Cheong XP, Nordin RB. Vaccine hesitancy among parents in Kuala Lumpur: a single center study. F1000Research, 2019; 8:1653; http/doi.org/10.12688/f1000research.20079.1 CrossRef
Ongpoy R. Level of Preparedness of the Filipino Pharmacists as Providers of immunizations for adult patients. ASIO J Pharm Herbal Med Res, 2017; 2(1):4–8.
Orenstein WA, Schaffner W. Lessons learned: role of influenza vaccine production, distribution, supply, and demand—What it means for the provider. Am J Med, 2008; 121(7 Suppl 2):S22–7; http/doi.org/10.1016/j.amjmed.2008.05.004 CrossRef
Panting AJ. Potential factors contributing to vaccine hesitancy among parents in malaysia?: an overview. Int J Health Sci Res, 2018; 8(7):360–5.
Papastergiou J, Folkins C, Li W, Zervas J. Community pharmacist–administered influenza immunization improves patient access to vaccination. Can Pharm J, 2014; 147(6):359–65; http/doi.org/10.1177/1715163514552557 CrossRef
Pearl L. Health minister studying pharmacists’ proposal to vaccinate, 2019. Available from https://twentytwo13.my/issues/health-minister-studying-pharmacists-proposal-to-vaccinate/ (Accessed 17 June 2020)
Pilisuk T, Goad J, Backer H. Vaccination delivery by chain pharmacies in California: Results of a 2007 survey. J Am Pharma Assoc, 2010; 50(2):134–9; http/doi.org/10.1331/JAPhA.2010.09168 CrossRef
Poulose S, Cheriyan E, Cheriyan R, Weeratunga D, Adham M. Pharmacist-administered influenza vaccine in a community pharmacy: a patient experience survey. Can Pharm J, 2015; 148(2):64–7; http/doi.org/10.1177/1715163515569344 CrossRef
Prosser LA, O’Brien MA, Molinari NA, Hohman KH, Nichol KL, Messonnier ML, Lieu TA. Non-traditional settings for influenza vaccination of adults?: costs and cost effectiveness. PharmacoEconomics, 2008; 26(2):163–78; http/doi.org/10.2165/00019053-200826020-00006 CrossRef
Raosoft. Raosoft, 2004. Available from http://www.raosoft.com/samplesize.html
Rodrigues IB, Adachi JD, Beattie KA, MacDermid JC. Development and validation of a new tool to measure the facilitators, barriers and preferences to exercise in people with osteoporosis. BMC Musculosk Disord, 2017; 18(1):1–9; http/doi.org/10.1186/s12891-017-1914-5 CrossRef
Rosado H, Bates I, Pyzik O, Pinto GBL. An overview of current pharmacy impact on immunisation A global report Colophon, 2016. International Pharmaceutical Federation, The Hague, Netherlands. Available from https://www.fip.org/files/fip/publications/FIP_report_on_Immunisation.pdf
Schwerzmann J, Graitcer SB, Jester B, Krahl D, Jernigan D, Bridges CB, Miller J. Evaluating the impact of pharmacies on pandemic influenza vaccine administration. Dis Med Public Health Prepared, 2017; 11(5):587–93; http/doi.org/10.1017/dmp.2017.1 CrossRef
Singhal PK, Zhang D. Costs of adult vaccination in medical settings and pharmacies: an observational study. J Manag Care Pharm, 2014; 20(9):930–6; http/doi.org/10.18553/jmcp.2014.20.9.930 CrossRef
Soon R. Make vaccinations mandatory, involve pharmacists, 2019. Available from https://specialty.mims.com/topic/mps--make-vaccinations-mandatory--involve-pharmacists (Accessed 8 November 2019)
Taber KS. The use of cronbach’s alpha when developing and reporting research instruments in science education. Res Sci Edu, 2018; 48(6):1273–96; http/doi.org/10.1007/s11165-016-9602-2 CrossRef
Tan ZS. Analysis report: distribution of poison license a holders and community pharmacies in Malaysia, 2019. Available from https://www.mps.org.my/newsmaster.cfm?&menuid=37&action=view&retrieveid=7732 (Accessed 8 November 2019)
Tannous LK, Barlow GM, Betcalfe NH. A short clinical review of vaccination against measles. J Royal Soc Med Open, 2014; 5(4):2054270414523408; http/doi.org/10.1177/2054270414523408 CrossRef
Tony I, Chou F, Lash DB, Malcolm B, Yousify L, Quach JY, Dong S, Yu J. Effects of a student pharmacist consultation on patient knowledge and attitudes about vaccines. J Am Pharm Assoc, 2014; 54(2):130–7; http/doi.org/10.1331/JAPhA.2014.13114 CrossRef
Usami T, Hashiguchi M, Kouhara T, Ishii A, Nagata T, Mochizuki M. Impact of community pharmacists advocating immunization on influenza vaccination rates among the elderly. Yakugaku Zasshi, 2009; 129(9):1063–8; http/doi.org/10.1248/yakushi.129.1063 CrossRef
Valiquette JR, Bédard P. Community pharmacists’ knowledge, beliefs and attitudes towards immunization in Quebec. Can J Public Health, 2015; 106(3):89–94; http/doi.org/10.17269/CJPH.106.4880 CrossRef
Warner JG, Portlock J, Smith J, Rutter P. Increasing seasonal influenza vaccination uptake using community pharmacies: experience from the Isle of Wight, England. Int J Pharm Pract, 2013; 21(6):362–7; http/doi.org/10.1111/ijpp.12037 CrossRef
Wan Taib WR, Yusoff NA, Tengku MA, Aryati A. Issues in vaccine hesitancy in Malaysia: a countering approach. J Biomed Clin Sci, 2017; 2(1)(June):42–6. Available from https://pdfs.semanticscholar.org/b8f8/56cdc7b650b24621b2698cf75dce6006c924.pdf
Wang J, Ford LJ, Uroza SF, Jaber N, Smith CT, Randolph R, Lane S, Foster SL. Effect of pharmacist intervention on herpes zoster vaccination in community pharmacies. J Am Pharma Assoc, 2013; 53(1):46–53; http/doi.org/10.1331/JAPhA.2013.12019 CrossRef
Welch AC, Ferreri SP, Blalock SJ, Caiola SM. North Carolina family practice physicians’ perceptions of pharmacists as vaccinators. J Am Pharma Assoc, 2005; 45(4):486–91; http/doi.org/10.1331/1544345054475414 CrossRef
Westrick SC, Patterson BJ, Kader MS, Rashid S, Buck PO, Rothholz MC. National survey of pharmacy-based immunization services. Vaccine, 2018; 36(37):5657–64; http/doi.org/10.1016/j.vaccine.2018.07.027 CrossRef
WHO. Measles—Western Pacific Region, 2019. WHO, Geneva, Switzerland. Available from https://www.who.int/csr/don/07-may-2019-measles-western-pacific-region/en/
World Health Organization. Ten threats to global health in 2019, 2019. World Health Organization, Geneva, Switzerland Available from https://www.who.int/emergencies/ten-threats-to-global-health-in-2019 (Accessed 8 November 2019)