INTRODUCTION
Antenatal care (ANC) is of utmost importance for the safe delivery of newborns and mothers’ well-being (Bee et al., 2018; Mangwi Ayiasi et al., 2014; Phommachanh et al., 2019). ANC is defined as the care provided by skilled healthcare professionals to pregnant women and adolescent girls to ensure the best health conditions for both mother and baby during pregnancy (WHO, 2016). ANC reduces maternal and perinatal morbidity and mortality directly by detecting and treating pregnancy-related complications (Haftu et al., 2018; Tafere et al., 2018) and indirectly by identifying women and girls at increased risk of developing complications during labor and delivery (Konje et al., 2018; Lincetto et al., 2006; Tikmani et al., 2019). Pregnant mothers receive counseling through the ANC regarding childbirth, safety, and complications, which help expectant mothers decide whether to utilize skilled healthcare professional assistance throughout the delivery process (Ayele et al., 2019; McNellan et al., 2019). Furthermore, child delivery is a crucial determinant in maternal mortality (Ahinkorah et al., 2021; Cameron et al., 2019; Rosário et al., 2019). The place of delivery (healthcare institution or home) and the type of care a woman gets during childbirth determine pregnancy outcomes (Abebe et al., 2012). A study conducted in Sub-Saharan Africa demonstrated that the overall prevalence for healthcare facility delivery was 66%. The determinants of the place of delivery were country, age, place of residence, level of education, wealth status, marital status, partner’s educational level, number of ANC visits, utilization of a skilled ANC provider during delivery, distance to a health facility, listening to the radio, and watching television (Adde et al., 2020).
In a study conducted in Ethiopia (Abebe et al., 2012) regarding home deliveries, women who utilized home delivery services lacked knowledge about obstetrics care, delayed starting ANC follow-up, were illiterate, and stayed in rural areas. The process of labor, when conducted at home especially inducted by unskilled healthcare professionals, increases the possibility of complications that include maternal morbidity and mortality, such as postpartum hemorrhage, birth trauma, infection, and fistula (Roy and Shengelia, 2016). Hence, it is of topmost priority that women have timely access to skilled care during pregnancy, during childbirth, and postpartum (Institute of Medicine, 2003; Sebghati and Chandraharan, 2017). In addition, another study (Central Statistical Agency, 2011) revealed that essential causes of delay to access healthcare facilities are transportation problems (71%), followed by lack of money (68%) and distance to a healthcare facility (66%).
In Nepal, many mothers do not have the means for adequate antenatal visits; thus, home deliveries take place despite the risks involved (Mahato et al., 2017; Mahato et al., 2020; Pradhan et al., 2013). The most common reason (Dhakal et al., 2018) for home delivery was an easy and convenient environment (66.7%), and that for institutional delivery was safety (77.8%). It was reported that Bangladeshi mothers from rural areas were 46.9% less likely to have institutional deliveries than urban dwellers (Yaya et al., 2017). Also, older expectant mothers aged between 30 and 49 years had a 23.6% higher prevalence of institutional delivery service utilization than their younger counterparts (Yaya et al., 2017). Those with higher educational attainment were about twice as likely to deliver at a standard healthcare facility. In addition, wealth status was also a significant predictor of institutional delivery service use (Yaya et al., 2017). Reducing maternal mortality is the ultimate goal for good ANC (Bintabara and Basinda, 2021; Kyei-Nimakoh et al., 2016; McDonagh, 1996; Rwabilimbo et al., 2020), even in low-income countries such as Bangladesh and Nepal (Kumar et al., 2016). Berhan and Berhan (2014) studies linking the number of antenatal visits to the place of delivery were lacking. This study was conducted to determine whether the number of ANC visits influences delivery in these two countries.
MATERIALS AND METHODS
Data source and study settings
The study analyzed Bangladesh and Nepal’s 2019 Multiple Indicator Cluster Survey (MICS) dataset (MICS website: https://mics.unicef.org/surveys).
Study design
The MICS 2019 survey identified rural and urban areas in each district or province as the primary sampling strata, and the sample of households was selected in two stages. Within each stratum at the first sampling stage, a specified number of census enumeration areas (EAs) were selected systematically with probability proportional to the size. After listing households within the selected EAs, many families were systematically drawn into each primary sampling unit. Then, women aged 15–49 from each family chosen were interviewed.
Sampling selection and sample size
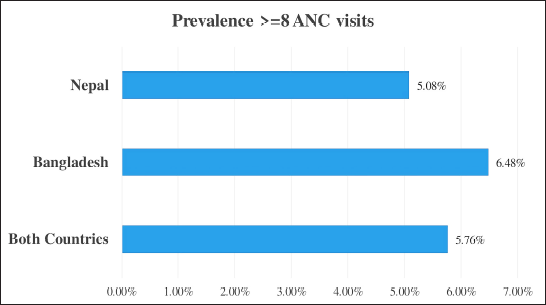
The sample for the Bangladesh and Nepal 2019 MICS was designed to provide approximations of several indicators from the situation of children and women from the national level comprising both urban and rural areas of these countries (GovBangladesh, 2019; GovNepal, 2019). The weighted sample size was 1,696 and 1,810 from Bangladesh and Nepal, respectively (Table 1).
Outcome variable
The outcome of this study was recorded from the variable place of delivery. The variable was coded as “home” and “institution.” “Home” was coded if the delivery took place in the respondent’s home or any other relative’s house, and “institution” was coded if the delivery took place anywhere besides home.
Predictor variables
The predictor variable (categorized into ≥4 visits and <4 visits and ≥8 visits and <8 visits) of this study was the number of prenatal care visits. The number of prenatal care visits was categorized into ≥4 and <4 visits, as well as ≥8 and <8 visits as per the guidance of the WHO (2016).
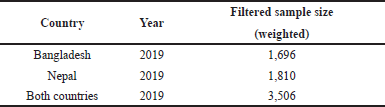 | Table 1. Weighted sample size obtained after filtration in each country. [Click here to view] |
Covariates
Age group (15–24, 25–34, and 35–49), media exposure (yes, no), residence (urban, rural), number of living children (1 or less, 2–3, and 4 or more), wealth index (poorest, more inadequate, middle, higher, and highest), and education level (no education, primary, secondary, and higher) were the variables selected as potential confounders from previous pieces of literature (Abebe et al., 2012; Adde et al., 2020; Awasthi et al., 2018; Belda and Gebremariam, 2016; Berhan and Berhan, 2014; Bishanga et al., 2018; Gebregziabhe et al., 2019; Gudu and Addo, 2017; Kebede et al., 2016; Kitui et al., 2013; Pandey et al., 2013).
Statistical analysis
Intially, the raw datasets were filtered through the data containing missing values; no response and data comprising human errors were challenging to resolve or interpret, predict, and covariates. Prevalence of institutional delivery in both the countries and the frequency of ≥4 ANC visits and ≥8 ANC visits were calculated. Binary logistic regression was run between the predictor and outcome variables (home, institution) to calculate the crude odds ratios for both countries. Furthermore, the binary logistic regression model was once more run between the predictor and outcome variables after controlling the covariates (age, education, wealth, media exposure, etc.) to calculate the adjusted odds ratios for both countries. Then the data of both the countries were pooled, and crude and adjusted odds ratios were calculated in the same manner from the pooled data. The Hosmer–Lemeshow goodness-of-fit test was performed to evaluate each model. All the analysis was done after incorporating the survey weight as well as the complex survey design. The whole study was done using software R version 4.0.2 and Microsoft Excel.
Ethical approval
The current study used publicly available data (secondary) sources that already received ethical approvals for the primary studies in each country and thus did not require further ethical approval. The ethical consent was taken from the respective participants.
RESULTS
Prevalence of institutional delivery and ANC visits in both countries
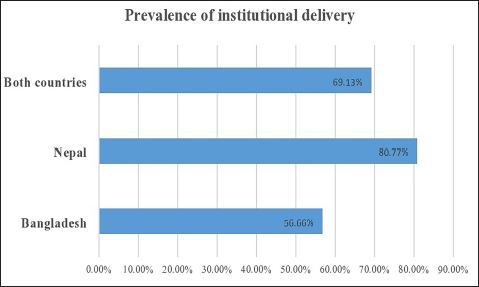
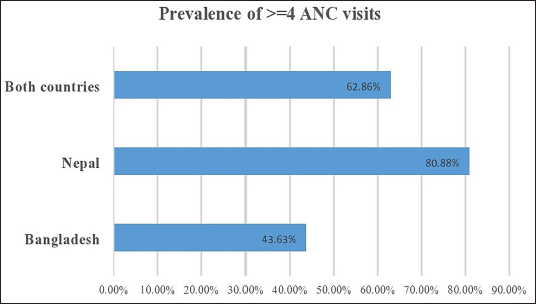
In the pooled data, the prevalence of institutional delivery is 69.13% (Fig. 1). The occurrence of institutional delivery is more prevalent in Nepal compared to Bangladesh. Similarly, the number of ≥4 ANC visits is higher in Nepal compared to Bangladesh. The overall prevalence of ≥4 ANC visits in the two countries is 62.86% (Fig. 2). Conversely, the bulk of ≥8 ANC visits is higher in Bangladesh than in Nepal (Fig. 3). In the pooled data, the prevalence of ≥8 ANC visits is only 5.76%.
Binary logistic regression model between ANC visits and place of delivery
In both countries, the binary logistic regression model suggests that women attending ≥4 visits are more likely to have institutional delivery (COR: 5.38, 95% CI:4.47–6.48), and similar results persisted (AOR: 4.16, 95% CI: 3.42–5.06) after controlling for the confounders age group, residence, education level, number of living children, wealth index, and media exposure. Similarly, in both the individual countries—Bangladesh (AOR: 2.76, 95% CI: 2.08–3.66) and Nepal (AOR: 3.14, 95% CI: 2.33–4.24)—women visiting ≥4 times are more likely to have institutional delivery compared to women visiting <4 times (Table 2). When categorizing the number of ANC visits according to the new guidelines of the WHO, similar results were obtained in individual countries and combinedly: women visiting ANC ≥8 times are more likely to have institutional delivery than the women visiting <8 times (Table 3).
 | Figure 1. Prevalence of institutional delivery. [Click here to view] |
 | Figure 2. Prevalence of four or more ANC visits. [Click here to view] |
 | Figure 3. Prevalence of eight or more ANC visits. [Click here to view] |
DISCUSSION
This study reports the prevalence of institutional delivery and ANC visits among women of childbearing age in Nepal and Bangladesh based on the data from the MICS. The study highlighted that the quality of ANC services influences women’s healthcare-seeking behavior, including delivery. Notably, the institutionalization of the eight or more ANC contact model remained low in both countries.
Prevalence of institutional delivery
The 2011 Bangladesh Demographic and Health Survey (BDHS) data showed that less than one-third of women reported institutional delivery (Yaya et al., 2017). Over the past few years, the country has achieved remarkable progress in utilizing maternal healthcare services. The 2017–2018 Bangladesh DHS (BDHS 2017–2018) findings showed that about half (49.4%) of all live births in the 3 years before the survey were delivered at a health facility (NIPORT and ICF, 2020). Our study revealed a higher prevalence (56.7%) of institutional delivery based on the Bangladesh MICS 2019.
The prevalence of institutional delivery in Nepal in this study was 80.77%. A similar prevalence rate of 83.7% was found in a cross-sectional survey among 245 mothers having children aged up to 2 years in the Kaski district of Nepal (Acharya and Pandey, 2015). The Nepal DHS in 2016 found a lower prevalence (57.5%) of institutional delivery than in our study based on the data on all live births in the country in the 5 years preceding the survey (Ministry of Health, 2017). Inconsistencies between the DHS and MICS results may have been attributed to differences in the reference periods used to measure coverage and the population covered (Amouzou et al., 2017).
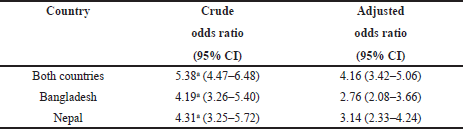 | Table 2. Crude odds ratio and adjusted odds ratio after controlling covariates between ANC visits and place of delivery. [Click here to view] |
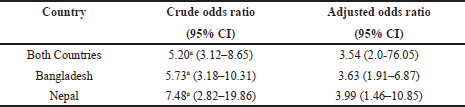 | Table 3. Crude odds ratio and adjusted odds ratio after controlling for the confounders between ANC visits and place of delivery according to the new guidelines of WHO. [Click here to view] |
Generally, the proportion of facility delivery is positively associated with the level of education and socioeconomic status (Yaya et al., 2017; Uddin et al., 2019). However, socioeconomic disparities in maternity care facilities affect people differently between the countries (Do et al., 2015). Based on the results of a comparative analysis of the data from surveillance sites in South Asia, it was found that the use of private sector maternity care facilities in Bangladesh was greater for better educated and wealthier women in Bangladesh. In Nepal, on the contrary, it was more common for less educated and poorer women to deliver at private sector facilities (Das et al., 2016).
Prevalence of ANC follow-ups
The proportion of women with four or more ANC visits in Bangladesh in this study (43.6%) was in line with the latest DHS in this country (47.9%) (NIPORT and ICF, 2020). Our research found a higher prevalence of women with four or more ANC visits in Nepal (80.9%) than the latest nationwide DHS (69.4%) (Acharya and Pandey, 2015). The latest WHO guidelines recommend ANC models with a minimum of eight visits (WHO, 2016). Evidence supports an association of the previously recommended four-visit focused ANC model, developed in the 1990s, with higher perinatal mortality than models that included at least eight visits (Dowswell et al., 2015). The updated recommendations were also influenced by evidence indicating improved pregnancy experience and safety during pregnancy through more contact between pregnant women and healthcare practitioners (Downe et al., 2016).
The new ANC model with eight or more visits has yet to be fully implemented in Bangladesh and Nepal. In our study, the coverage of eight or more ANC visits was low in Bangladesh (6.5%) and Nepal (5.1%), attributed to individual-, cultural-, and healthcare-related factors. A recent study from Nigeria reported that 17.4% of women had eight or more ANC visits based on the data from the latest national DHS (Ekholuenetale et al. 2020). The results of a study using the 2019 population-based data in Ghana found a much higher prevalence of eight and more ANC visits (41.9%) (Ekholuenetale et al., 2021). Improved infrastructures and overcoming hurdles such as lack of knowledge, long distances to health facilities, and extended hospital waiting time would bring ANC closer to women, specifically in the rural areas. These are required to improve the institutionalization of the eight or more ANC contact models in Bangladesh and Nepal (Acharya and Pandey, 2015; Sarker et al., 2020).
Factors associated with institutional delivery
This study aimed to understand better the underlying factors of institutional delivery to sustain the progress in its utilization in both countries. The factors contributing to the use of health services for delivery by women include their literacy and a higher level of education, higher socioeconomic status, working status, and urban residency (Agha and Williams; 2016; Fekadu et al., 2019; Mukherjee and Roy; 2020). One of the most effective approaches to increase the use of facility delivery services is ANC. ANC visits provide an opportunity for health promotion, ensuring that women better understand home delivery risks and are better adjusted to the healthcare facility environment (Fekadu et al., 2018). The frequency of ANC visits expresses the perceived need that plays a crucial role in utilizing facility delivery service (Nigusie et al., 2020).
Our results show that the number of ANC visits was positively associated with the prevalence of institutional delivery in Bangladesh and Nepal. The women who had completed four ANC visits had about three times higher odds of having facility delivery than those who completed fewer than four ANC visits. Compliance with the new WHO guidelines of completing eight ANC visits resulted in even higher odds of delivering at a health facility. Therefore, establishing contact with the health services during pregnancy motivates and enables women to use them for giving birth. Several studies revealed similar positive effects of ANC on institutional delivery (Devkota et al., 2020; Dixit et al., 2017; Ejigu et al., 2018; Fekadu et al., 2018; Yaya et al. 2017).
Strengths and Limitations
Although many studies assessed the role of ANC in the uptake of institutional delivery services, our study addressed the issue of the association of a specific component of ANC—the number of ANC visits—and facility delivery in two South Asian countries, Bangladesh and Nepal. Previous studies in different countries mostly used the data on ANC visits and delivery from the DHS. One of the limitations of this study is cross-sectional survey data, so the reported association between the frequency of ANC visits and the prevalence of institutional delivery may change in studies accounting for the temporal relationship between the variables. Moreover, our research could have been exposed to a recall bias due to the self-reported number of ANC visits. Nevertheless, we used a nationally representative large sample from the MICS that focuses on women who had given birth in the last 2 years preceding the survey. Thus, the possibility of recall bias is minimized within this period.
CONCLUSION
In this study, we have found that the quality of ANC services influences women’s healthcare-seeking behavior, including delivery. However, the institutionalization of the eight-or-more ANC contact model remained low in both countries, showing a perceived lack of need for institutional delivery among the women in both countries. The MICS data of both countries supported the association between the frequency of ANC visits and the prevalence of facility delivery services.
RECOMMENDATIONS
There is an urgent need to adopt and implement WHO’s new evidence-based global recommendation on ANC visits based on the country’s context and populations’ needs to decrease maternal and child mortality rates. Concerted efforts from relevant stakeholders should be implemented to improve ANC compliance. The ANC visits should incorporate behavioral interventions to support women’s intention to deliver at a health facility.
ARTICLE HIGHLIGHTS
ANC is an essential component of the reproductive health continuum that ensures safe delivery of babies and mothers’ wellbeing, including health promotion, screening and diagnosis, and disease prevention. It reduces maternal and perinatal morbidity and mortality.
- In low-income countries such as Bangladesh and Nepal, the quality of ANC provision, in general, remains inadequate.
- According to Bangladesh and Nepal’s 2019 MICS dataset, I. the occurrence of institutional delivery and ≥4 ANC visits are higher in Nepal compared to Bangladesh, II. in both countries, women attending ≥4 visits are more likely to have institutional delivery, and III. in both countries, women who had ≥4 ANC visits or ≥8 ANC visits are more likely to have institutional delivery than women who had <4 ANC visits or <8 ANC visits, respectively.
- The MICS data of both countries supported the association between the frequency of ANC visits and the prevalence of facility delivery services.
- There is an urgent need to adopt and implement WHO’s new evidence-based global recommendations on ANC visits based on the context of each country and populations’ needs to decrease maternal and child mortality rates.
ACKNOWLEDGMENT
The authors express their sincere gratitude to Ms. Faiza Binte Mozammel, Photographer and Editor, student of the Department of BBA, Independent University Bangladesh, Bashundhara, Dhaka, Bangladesh, for her kind effort and time regarding image editing.
CONFLICT OF INTERESTS
None.
AUTHORS’ CONTRIBUTIONS
All authors made significant contributions to the work reported, whether it is in the conception, study design, execution, acquisition of data, analysis, and interpretation or in all these areas; they took part in drafting, revising, or critically reviewing the article; gave final approval of the version to be published; agreed on the journal to which the article has been submitted; and agreed to be accountable for all aspects of the work, including any issues related to accuracy or integrity.
DISCLOSURE
The authors declare that they do not have any financial involvement or affiliations with any organization, association, or entity directly or indirectly with the subject matter or materials presented in this article. This includes honoraria, expert testimony, employment, ownership of stocks or options, patents or grants received or pending, or royalties.
DATA AVAILABILITY
The dataset used in this study is, without restrictions, available at https://mics.unicef.org/surveys. Nevertheless, admittance to the dataset necessitates registration and is granted only for authentic research motives.
REFERENCES
Abebe F, Berhane Y, Girma B. Factors associated with home delivery in Bahirdar, Ethiopia: a case-control study. BMC Res Notes, 2012; 5:653; doi: 10.1186/1756-0500-5-653 CrossRef
Acharya S, Pandey A. Place of delivery and newborn care practices in Kaski district: a cross-sectional study from Nepal. J Biomed Sciences, 2015; 1(2):6–11; doi: 10.3126/jbs.v1i2.11863 CrossRef
Adde KS, Dickson KS, Amu H. Prevalence and determinants of the place of delivery among reproductive-age women in sub–Saharan Africa. PLoS One, 2020; 15(12):1–14; doi: 10.1371/journal.pone.0244875 CrossRef
Agha S, Williams E. Quality of antenatal care and household wealth as determinants of institutional delivery in Pakistan: results of a cross-sectional household survey. Reprod Health, 2016; 13(1):84; doi: 10.1186/s12978-016-0201-5 CrossRef
Ahinkorah BO, Seidu AA, Agbaglo E, Adu C, Budu E, Hagan JE Jr, Schack T, Yaya S. Determinants of antenatal care and skilled birth attendance services utilization among childbearing women in Guinea: evidence from the 2018 Guinea Demographic and Health Survey data. BMC Pregnancy Childbirth, 2021; 21(1):2; doi: 10.1186/s12884-020-03489-4 CrossRef
Amouzou A, Mehra V, Carvajal-Aguirre L, Khan SM, Sitrin D, Vaz LM. Measuring postnatal care contacts for mothers and newborns: an analysis of data from the MICS and DHS surveys. J Glob Health, 2017; 7(2):020502; doi: 10.7189/jogh.07.020502 CrossRef
Awasthi MS, Awasthi KR, Thapa HS, Saud B, Pradhan S, Khatry RA. Utilization of antenatal care services in dalit communities in Gorkha, Nepal: a cross-sectional study. J Pregnancy, 2018; 2018:3467308; doi: 10.1155/2018/3467308 CrossRef
Ayele GS, Melku AT, Belda SS. Utilization of skilled birth attendant at birth and associated factors among women who gave birth in the last 24 months preceding the survey in Gura Dhamole Woreda, Bale zone, southeast Ethiopia. BMC Public Health, 2019; 19(1):1501; doi: 10.1186/s12889-019-7818-6 CrossRef
Bee M, Shiroor A, Hill Z. Neonatal care practices in sub-Saharan Africa: a systematic review of quantitative and qualitative data. J Health Popul Nutr, 2018; 37(1):9; doi: 10.1186/s41043-018-0141-5 CrossRef
Belda SS, Gebremariam MB. Birth preparedness, complication readiness, and other determinants of place of delivery among mothers in Goba District, Bale zone, southeast Ethiopia. BMC Pregnancy Childbirth, 2016; 16(1):1–12; doi: 10.1186/s12884-016-0837-8 CrossRef
Berhan Y, Berhan A. Antenatal care as a means of increasing birth in the health facility and reducing maternal mortality: a systematic review. Ethiop J Health Sci; 2014; 24 (Suppl 0):93–104; doi: 10.4314/ejhs.v24i0.9s CrossRef
Bintabara D, Basinda N. Twelve-year persistence of inequalities in antenatal care utilization among women in Tanzania: a decomposition analysis of population-based cross-sectional surveys. BMJ Open; 2021; 11(4):e040450; doi: 10.1136/bmjopen-2020-040450 CrossRef
Bishanga DR, Drake M, Kim YM, Mwanamsangu AH, Makuwani AM, Zoungrana J, Lemwayi R, Rijken MJ, Stekelenburg J. Factors associated with institutional delivery: findings from a cross-sectional study in Mara and Kagera regions in Tanzania. PLoS One, 2018; 13(12):e0209672; doi: 10.1371/journal.pone.0209672 CrossRef
Cameron L, Contreras Suarez D, Cornwell K. Understanding the determinants of maternal mortality: an observational study using the Indonesian Population Census. PLoS One; 2019; 14(6):e0217386; doi:10.1371/journal.pone.0217386 CrossRef
Central Statistical Agency. Demographic and Health Survey 2011. Addis Ababa, Ethiopia, 2013. Available via https://dhsprogram.com/pubs/pdf/FR255/FR255.pdf (Accessed 29 May 2021).
Das S, Alcock G, Azad K, Kuddus A, Manandhar DS, Shrestha BP, Nair N, Rath S, More NS, Saville N, Houweling TAJ, Osrin D. Institutional delivery in public and private sectors in South Asia: a comparative analysis of prospective data from four demographic surveillance sites. BMC Pregnancy Childbirth, 2016; 16:273; https://doi.org/10.1186/s12884-016-1069-7 CrossRef
Devkota B, Maskey J, Pandey AR, Karki D, Godwin P, Gartoulla P, Mehta S, Arval KK. Determinants of home delivery in Nepal – a disaggregated analysis of marginalized and non-marginalized women from the 2016 Nepal Demographic and Health Survey. PLoS One, 2020; 15(1): e0228440; doi: 10.1371/journal.pone.0228440 CrossRef
Dhakal P MS, Shrestha M MS, Baral D MS, Pathak S MD. Factors affecting the place of delivery among mothers residing in Jhorahat VDC, Morang, Nepal. Int J Community Based Nurs Midwifery, 2018; 6(1):2–11.
Dixit P, Khan J, Dwivedi LK, Gupta A. Dimensions of antenatal care service and the alacrity of mothers towards institutional delivery in South and South East Asia. PLoS One, 2017; 12(7):e0181793; doi: 10.1371/journal.pone.0181793 CrossRef
Do M, Soelaeman R, Hotchkiss DR. Explaining inequity in the use of institutional delivery services in selected countries. Matern Child Health J, 2015; 19:755–63; doi: 10.1007/s10995-014-1561-5 CrossRef
Downe S, Finlayson K, Tunçalp Ö, Gülmezoglu AM. Factors that influence the uptake of routine antenatal services by pregnant women: a qualitative evidence synthesis. Cochrane Database Syst Rev; 2016; 2016(10):CD012392; doi: 10.1002/14651858.CD012392 CrossRef
Dowswell T, Carroli G, Duley L, Gates S, Gülmezoglu AM, Khan-Neelofur D, Piaggio G. Alternative versus standard packages of antenatal care for low-risk pregnancy. Cochrane Database Syst Rev, 2015; 2015(7):CD000934; doi: 10.1002/14651858.CD000934.pub3 CrossRef
Ejigu Tafere T, Afework MF, Yalew AW. Antenatal care service quality increases the odds of utilizing institutional delivery in Bahir Dar city administration, North Western Ethiopia: a prospective follow-up study. PLoS One, 2018; 13(2):e0192428; doi: 10.1371/journal.pone.0192428 CrossRef
Ekholuenetale M, Benebo FO, Idebolo AF. Individual-, household-, and community-level factors associated with eight or more antenatal care contacts in Nigeria: evidence from Demographic and Health Survey. PLoS One, 2020; 15(9):e0239855; doi: 10.1371/journal.pone.0239855 CrossRef
Ekholuenetale M, Nzoputam CI, Barrow A. Prevalence and socioeconomic inequalities in eight or more antenatal care contacts in Ghana: findings from 2019 population-based data. Int J Women’s Health, 2021; 13: 349–60; doi: 10.2147/IJWH.S306302 CrossRef
Fekadu GA, Ambaw F, Kidanie SA. Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth, 2019; 19(1):64; doi: 10.1186/s12884-019-2216-8 CrossRef
Fekadu GA, Kassa GM, Berhe AK, Muche AA, Katiso NA. The effect of antenatal care on use of institutional delivery service and postnatal care in Ethiopia: a systematic review and meta-analysis. BMC Health Serv Res, 2018; 18(1):577; doi: 10.1186/s12913-018-3370-9 CrossRef
Gebregziabher NK, Zerav AY, Abtew YT, Kinfe TD, Abrha DT. Factors determining choice of place of delivery: analytical cross-sectional study of mothers in Akordet town, Eritrea. BMC Public Health, 2019; 19(1):1–11; doi: 10.1186/s12889-019-7253-8 CrossRef
Government of Nepal (GovNepal). National Planning Commission, Central Bureau of Statistics. United Nations Children’s Fund (UNICEF). Multiple indicator cluster survey. Key indicators. Nepal. Government of Nepal, 2019. Available via https://www.unicef.org/nepal/media/9076/file/NMICS_2019_-_Key_findings.pdf (Accessed 29 August 2021).
Government of the Peoples Republic of Bangladesh (GovBangladesh). Bangladesh Bureau of Statistics (BBS) and United Nations Children’s Fund (UNICEF) Bangladesh. Progotir Pathey, Bangladesh multiple indicator cluster survey 2019. Survey Findings Report, 2019. Bangladesh Bureau of Statistics (BBS), Dhaka, Bangladesh. Available via https://www.unicef.org/bangladesh/media/3281/file/Bangladesh%202019%20MICS%20Report_English.pdf (Accessed 29 August 2021).
Gudu W, Addo B. Factors associated with utilization of skilled service delivery among women in rural Northern Ghana: a cross-sectional study. BMC Pregnancy Childbirth, 2017; 17(1):1–10; doi: 10.1186/s12884-017-1344-2 CrossRef
Haftu A, Hagos H, Mehari MA, G/Her B. Pregnant women adherence level to antenatal care visit and its effect on perinatal outcome among mothers in Tigray Public Health institutions, 2017: cohort study. BMC Res Notes, 2018; 11(1):872; doi: 10.1186/s13104-018-3987-0 CrossRef
Institute of Medicine (US) Committee on Improving Birth Outcomes. Improving birth outcomes: meeting the challenge in the developing world. In: Bale JR, Stoll BJ, Lucas AO (eds.). Reducing maternal mortality and morbidity, National Academies Press, Washington, DC, pp 372, 2003. Available via https://www.ncbi.nlm.nih.gov/books/NBK222105/ (Accessed 19 June 2021).
Kebede A, Hassen K, Teklehaymanot AN. Factors associated with institutional delivery service utilization in Ethiopia. Int J Women’s Health. 2016; 8:463–75; doi: 10.2147/IJWH.S109498 CrossRef
Kitui J, Lewis S, Davey G. Factors influencing place of delivery for women in Kenya: an analysis of the Kenya demographic and health survey, 2008/2009. BMC Pregnancy Childbirth, 2013; 13:40; doi: 10.1186/1471-2393-13-40 CrossRef
Konje ET, Magoma MTN, Hatfield J, Kuhn S, Sauve RS, Dewey DM. Missed opportunities in antenatal care for improving the health of pregnant women and newborns in Geita district, Northwest Tanzania. BMC Pregnancy Childbirth, 2018; 18(1):394; doi: 10.1186/s12884-018-2014-8 CrossRef
Kumar S, Kumar N, Vivekadhish S. Millennium development goals (MDGs) to sustainable development goals (SDGs): addressing unfinished agenda and strengthening sustainable development and partnership. Indian J Community Med, 2016; 41(1):1–4; doi: 10.4103/0970-0218.170955 CrossRef
Kyei-Nimakoh M, Carolan-Olah M, McCann TV. Millennium development goal 5: progress and challenges in reducing maternal deaths in Ghana. BMC Pregnancy Childbirth, 2016; 16:51; doi: 10.1186/s12884-016-0840-0 CrossRef
Lincetto O, Mothebesoane-Anoh S, Gomez P, Munjanja S. Antenatal care. WHO Press, World Health Organization, Geneva, Switzerland, 2006. Available via https://www.who.int/pmnch/media/publications/aonsectionIII_2.pdf (Accessed 28 May 2021).
Mahato P, van Teijlingen E, Simkhada P, Angell C, Hundley V. Evaluation of a health promotion intervention associated with birthing centers in rural Nepal. PLoS One, 2020; 15(5):e0233607; doi: 10.1371/journal.pone.0233607 CrossRef
Mahato PK, van Teijlingen E, Simkhada P, Sheppard ZA, Silwal RC. Factors related to choice of place of birth in a district in Nepal. Sex Reprod Healthc, 2017; 13:91–6; doi: 10.1016/j.srhc.2017.07.002 CrossRef
Mangwi Ayiasi R, Kasasa S, Criel B, Garimoi Orach C, Kolsteren P. Is antenatal care preparing mothers to care for their newborns? A community-based cross-sectional study among lactating women in Masindi, Uganda. BMC Pregnancy Childbirth, 2014; 14:114; doi: 10.1186/1471-2393-14-114 CrossRef
McDonagh M. Is antenatal care effective in reducing maternal morbidity and mortality? Health Policy Plan, 1996; 11(1):1–15; doi: 10.1093/heapol/11.1.1 CrossRef
McNellan CR, Dansereau E, Wallace MCG, Colombara DV, Palmisano EB, Johanns CK, Schaefer A, Ríos-Zertuche D, Zúñiga-Brenes P, Hernandez B, Iriarte E, Mokdad AH. Antenatal care as a means to increase participation in the continuum of maternal and child healthcare: an analysis of the poorest regions of four Mesoamérican countries. BMC Pregnancy Childbirth, 2019; 19(1):66; doi: 10.1186/s12884-019-2207-9 CrossRef
Ministry of Health, Nepal, New ERA, ICF. Nepal Demographic and Health Survey 2016. Ministry of Health, Kathmandu, Nepal, 2017. Available via https://www.dhsprogram.com/pubs/pdf/fr336/fr336.pdf (Accessed 28 May 2021).
Mukherjee M, Roy MP. Factors determining institutional delivery in eastern part of India. Tzu Chi Med J, 2020; 32:171–4. CrossRef
National Institute of Population Research and Training (NIPORT), ICF. Bangladesh Demographic and Health Survey 2017-18. NIPORT and ICF, Dhaka, Bangladesh, and Rockville, MD, 2020. Available via https://dhsprogram.com/pubs/pdf/FR344/FR344.pdf (Accessed 28 May 2021).
Nigusie A, Azale T, Yitayal M. Institutional delivery service utilization and associated factors in Ethiopia: a systematic review and META-analysis. BMC Pregnancy Childbirth, 2020; 20:364; doi: 10.1186/s12884-020-03032-5 CrossRef
Pandey JP, Dhakal MR, Karki S, Poudel P, Pradhan MS. Maternal and child health in Nepal: the effects of caste, ethnicity, and regional identity: further analysis of the 2011 Nepal Demographic and Health Survey. Kathmandu, Nepal, 2013. Available via https://www.dhsprogram.com/pubs/pdf/FA73/FA73.pdf (Accessed 29 May 2021).
Phommachanh S, Essink DR, Jansen M, Broerse JEW, Wright P, Mayxay M. Improvement of quality of antenatal care (ANC) service provision at the public health facilities in Lao PDR: perspective and experiences of supply and demand sides. BMC Pregnancy Childbirth, 2019; 19(1):255; doi: 10.1186/s12884-019-2345-0 CrossRef
Pradhan PM, Bhattarai S, Paudel IS, Gaurav K, Pokharel PK. Factors contributing to antenatal care and delivery practices in Village Development Committees of Ilam district, Nepal. Kathmandu Univ Med J (KUMJ), 2013; 11(41):60–5; doi: 10.3126/kumj.v11i1.11029 CrossRef
Rosário EVN, Gomes MC, Brito M, Costa D. Determinants of maternal health care and birth outcome in the Dande Health and Demographic Surveillance System area, Angola. PLoS One, 2019; 14(8):e0221280; doi: 10.1371/journal.pone.0221280 CrossRef
Roy A, Shengelia L. An analysis on maternal healthcare situation in Bangladesh: a review. Divers Equal Health Care, 2016; 13:360–4. Available via https://diversityhealthcare.imedpub.com/an-analysis-on-maternal-healthcare-situation-inbangladesh-a-review.pdf (Accessed 19 June 2021). CrossRef
Rwabilimbo AG, Ahmed KY, Page A, Ogbo FA. Trends and factors associated with the utilization of antenatal care services during the Millennium Development Goals era in Tanzania. Trop Med Health, 2020; 48:38; doi: 10.1186/s41182-020-00226-7 CrossRef
Sarker BK, Rahman M, Rahman T, Rahman T, Khalil JJ, Hasan M, Rahman F, Ahmed A, Mitra DK, Mridha MK, Rahman A. Status of the WHO recommended timing and frequency of antenatal care visits in Northern Bangladesh. PLoS One, 2020; 15(11):e0241185; doi: 10.1371/journal.pone.0241185 CrossRef
Sebghati M, Chandraharan E. An update on the risk factors for and management of obstetric hemorrhage. Womens Health (Lond), 2017; 13(2):34–40; doi: 10.1177/1745505717716860 CrossRef
Tafere TE, Afework MF, Yalew AW. Providers adherence to essential contents of antenatal care services increases birth weight in Bahir Dar City Administration, north West Ethiopia: a prospective follow up study. Reprod Health, 2018; 15(1):163; doi: 10.1186/s12978-018-0610-8 CrossRef
Tikmani SS, Ali SA, Saleem S, Bann CM, Mwenechanya M, Carlo WA, Figueroa L, Garces AL, Krebs NF, Patel A, Hibberd PL, Goudar SS, Derman RJ, Aziz A, Marete I, Tenge C, Esamai F, Liechty E, Bucher S, Moore JL, McClure EM, Goldenberg RL. Trends of antenatal care during pregnancy in low- and middle-income countries: findings from the global network maternal and newborn health registry. Semin Perinatol, 2019; 43(5):297–307; doi: 10.1053/j.semperi.2019.03.020 CrossRef
Uddin J, Pulok MH, Johnson RB, Rana J, Baker E. Association between child marriage and institutional delivery care services use in Bangladesh: intersections between education and place of residence. Public Health, 2019; 171:6–14; doi: 10.1016/j.puhe.2019.03.014 CrossRef
World Health Organization. WHO recommendations on antenatal care for a positive pregnancy experience. WHO Press, WHO, Geneva, Switzerland, 2016. Available via https://apps.who.int/iris/bitstream/handle/10665/250796/9789241549912-eng.pdf;jsessionid=6F6AC4C545BE0C85C9C83014B2507C18?sequence=1 (Accessed 28 May 2021).
Yaya S, Bishwajit G, Ekholuenetale M. Factors associated with the utilization of institutional delivery services in Bangladesh. Plos One, 2017; 12(2):e0171573; doi: 10.1371/journal.pone.0171573 CrossRef