INTRODUCTION
An increase in systolic or diastolic blood pressure is called hypertension (HTN). According to JNC 8, systolic blood pressure greater than 140 mmHg and diastolic blood pressure greater than 90 mmHg is classified as HTN (James et al., 2014). HTN leads to many diseases mainly angina, ischemic attack, and stroke. Various complications arise because of HTN (Cubrilo-Turek, 2003; Reshma et al., 2012). Persons with high blood pressure are at a higher risk of developing cardiovascular diseases when compared to the general population (Fuchs and Whelton, 2020).
Increased blood pressure is a major risk factor, which is a reason for death across the world (Lawes et al., 2008). In 2000, one billion adults had HTN, and this will rise to 1.56 billion by the end of 2025 (Mills et al., 2016). Several studies have reported that the prevalence of HTN is rapidly increasing in developing countries (Singh et al., 2017).
Indian scenario of HTN
The overall prevalence of HTN in India is about 29.8% (33.8% - urban; 27.6% - rural). A systematic review reported that there is an increase in the prevalence of HTN in the rural and urban population (Anchala et al., 2014).
Even though non-pharmacological therapies are efficient in reducing blood pressure, people usually do not follow it regularly. Also, majority of the people have high BP, despite non-pharmacological therapy. In these situations, pharmacological therapy would be appropriate (Gupta and Guptha, 2010).
There is a great variation in the prevalence of HTN between developed countries and developing countries. It has been greatly increased in the urban and rural population, especially in India, and the rate is more in urban population (Das et al., 2005). Different studies have reported varying proportions of uncontrolled HTN in adults in India (23.4%–89%) (Gupta et al., 2012; Nagappa et al., 2018; Sumit et al., 2012). But the geriatric population is more prone to be affected by HTN. Men are more affected when compared to women. There is a positive correlation between their age and HTN. Timely and rational management of HTN is essential to reduce the complications of HTN (Lionakis et al., 2012). Uncontrolled HTN leads to various complications, and the incidence of stroke (57%) and coronary artery disease (CAD)-related deaths (24%) are more with uncontrolled HTN (Ramakrishnan et al., 2019).
Several guidelines for HTN are available around the world. For example, the International Society of HTN Global HTN Practice Guidelines, Eighth Report of the Joint National Committee (JNC 8) guidelines, Canadian recommendations for the management of HTN, and the British HTN Society guidelines for HTN management (Hernandez-Vila, 2015). The JNC 8 guidelines provide a stepwise algorithm for the therapeutic management. This guideline algorithm provides easy understanding at a glance. It also directs and assists the physicians during their therapeutic approach. The guidelines’ main goal is to achieve the target blood pressure and hence to reduce the complications. But still there are variations in the choice of antihypertensives among different guidelines (Arshad et al., 2021). According to the JNC 8 guidelines, the initial drugs of choice for HTN are angiotensin-converting enzyme inhibitors (ACEIs), angiotensin-receptor blockers (ARB), thiazide diuretics, and calcium channel blockers (CCBs) (James et al., 2014).
The patient’s demographic and clinical characteristics should be thoroughly assessed by the physicians, before determining effective treatment. The practice patterns of physicians must adhere to the guidelines for effective outcome of therapy (Buang et al., 2019). The practice pattern and the attitude of physicians also play a major role in the effective management of HTN. In routine practice, the choice of antihypertensives is usually neglected (Burnier and Egan, 2019). There is strong evidence that irrational antihypertensive prescription will lead to increased healthcare costs to both individual patients and society as a whole. Hence, it is essential to study the prescription pattern and its adherence to the guidelines to minimize the cost and to prevent irrational prescribing (Jain et al., 2015). Special care must be taken especially for the geriatric population since they are a high-risk population group.
A study on prescribing patterns of antihypertensives in geriatric patients was conducted and it reported that that the most commonly prescribed drug classes involved were CCBs, followed by angiotensin II receptor antagonists (Mohd et al., 2012). The authors also added that this practice had a positive impact on controlling blood pressure. Prescribing patterns of antihypertensive drugs in the geriatric population in tertiary care hospital was studied and the most commonly prescribed monotherapy was CCBs (amlodipine), followed by ARBs (telmisartan) (Philip et al., 2016). There were very few studies analyzing the prescribing pattern of antihypertensives in geriatric patients. Moreover, studies which compare the same with the JNC 8 treatment guidelines were lacking.
Hence, this study was conducted with the objective of assessing the current prescribing pattern of antihypertensives in the geriatric population and to compare the prescription pattern with the JNC 8 guidelines.
MATERIALS AND METHODS
A prospective observational study was conducted in the general medicine unit of a tertiary care hospital, for 5 months. Convenience sampling technique was used to select the study sample. The sample size was calculated based on the number of patients visiting the general medicine unit of the hospital during the 5-month study period, considering a dropout of 20%. Ethical approval was obtained from Institutional Ethics Committee, Vels University, before conducting this study (IEC/2019/I/15). Patients of either sex above 65 years, diagnosed as hypertensive as per the JNC 8 guidelines, and patients receiving or prescribed with antihypertensive drugs were included. The patients who were not willing to participate in the study were excluded. Four hundred patients were included in the study. The demographics of the patients, clinical and laboratory findings, and the therapeutic details were collected.
Data collection
The patients who visited the outpatient department of the general medicine unit, who were diagnosed to be hypertensive, were reviewed. The hypertensive patients who met the inclusion criteria were included in the study. The blood pressure at the time of inclusion in the study was taken. The patients’ demographic characteristics, their antihypertensive medication prescribed and its characteristics (name of medication, class, dose, and frequency), and socio-demographic status were also documented in a data collection form designed for the study. The antihypertensive medications used to treat the patients were then analyzed and compared with the JNC 8 treatment guidelines. The guidelines clearly explain the initial choice of drugs for HTN, treatment choice for various comorbidities, and the agents of choice in each class of medications. The drugs prescribed for the study population were compared with the guidelines based on the drugs of choice, dose, frequency, and comorbidities.
Data analysis
Data were entered and analyzed by Statistical Package for the Social Sciences version 21.0 and expressed as number and percentage.
RESULTS AND DISCUSSION
Our study aimed at finding out the anti-HTN prescription patterns, comparing it with the standard treatment guidelines (JNC 8) and the extent of deviation, comparing the medications used in the treatment of HTN.
Four hundred patients were included for the study. With regard to the demographic data, majority of our study population were male, most patients were from 66 to 70 years, many had normal body mass index (BMI), majority had a family history of HTN, most of the elderly were smokers and alcoholics, and majority were of stage-II HTN.
There was an increase in males (53%) compared to females (47%). Other studies revealed the same results (Chandra et al., 2019; Mohd et al., 2012; Philip et al., 2016; Sharma et al., 2018). Majority were in the age group of 66–70 years (87%). This was similar to another study (Mohd et al., 2012).
Of the 400 patients evaluated, 252 (63%) patients were found with normal BMI, 96 (24%) patients were obese, and 52 (13%) patients were underweight. 85% (40% male and 45% female) of the patients had a family history of HTN. In this study, 76 (19%) patients were smokers and 136 (34%) patients were smokers + alcoholics.
Hypertensive patients were categorized based on the JNC 8 as depicted in Table 1. Of the 400 patients evaluated, 240 (60%) patients were in stage II. This was in contrast to another study in which majority of the patients were in pre-hypertensive stage (Pavani et al., 2012). This could be due to variations in the study site and study population.
The most commonly prescribed drug classification was CCBs (88%), followed by beta blockers (BBs) (65%) (Table 2). This was in accordance with the study conducted by Mohd et al. (2012), in which the commonly prescribed drug was CCBs, whereas the second commonly prescribed drug was ARBs.
Table 3 depicts the drugs prescribed based on the age group. CCBs (88%) were found to be most prescribed drugs for all the age groups.
Among the CCB, amlodipine 5–10 mg was the most prescribed drug. These results are comparable with other study results (Almas et al., 2011; Datta and Sharma, 2010; Datta, 2011; Neal et al., 2000). Atenolol was commonly prescribed among BB, enalapril among ACEI, and hydrochlorothiazide (HCTZ) among thiazide diuretics.
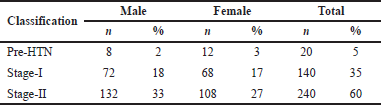 | Table 1. Stages of HTN based on JNC 8 guidelines. [Click here to view] |
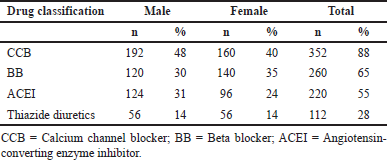 | Table 2. Drugs prescribed based on gender. [Click here to view] |
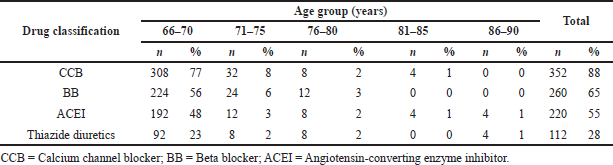 | Table 3. Drugs prescribed based on age group. [Click here to view] |
Monotherapy was prescribed for 2% of the patients, dual therapy for 78%, triple therapy for 15%, and quadruple therapy for 5% of the patients. Amlodipine was the only monotherapy prescribed. Among the dual therapy, atenolol + amlodipine was commonly prescribed. This was not in accordance with other studies (Datta, 2011; Datta and Sharma, 2010) in which diuretics was used in combination with other agents. The study population, the study site, and the prescribing physician change the results considerably. Atenolol + HCTZ + amlodipine were commonly prescribed among the triple therapy and atenolol + HCTZ + amlodipine + enalapril among the quadruple therapy (Table 4). Males were commonly prescribed with combination drug therapy than females.
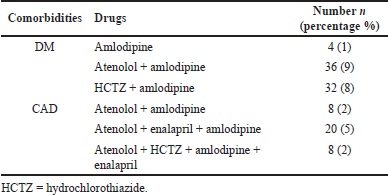
Anti-HTN prescribing patterns were classified into HTN with comorbidities (27%) and HTN without comorbidities (73%). This was similar to the study conducted by Philip et al. (2016). The use of antihypertensive drugs in HTN with comorbidities is summarized in Table 5.
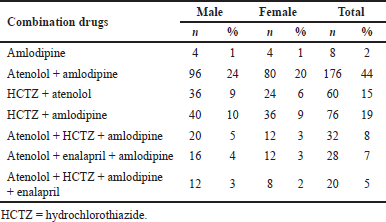 | Table 4. Various drug combinations prescribed based on gender. [Click here to view] |
 | Table 5. Use of antihypertensive drugs for HTN with comorbidities. [Click here to view] |
Diabetes mellitus (DM) was the common comorbidity found in majority of the population. This was similar to a study conducted by Mohd et al. (2012).
According to the JNC 8 guidelines, the initial drugs of choice for HTN are ACEI, ARBs, thiazide diuretic, or CCBs. Our study population was prescribed commonly with CCBs, which was in accordance with the JNC 8 treatment algorithm. The second most commonly prescribed drug was BBs in our study, but BBs were not a preferred therapy according to the guidelines (James et al., 2014).
Among the CCBs, amlodipine was the mostly prescribed drug, atenolol among BBs, enalapril among ACEIs, and hydrochlorothiazide among thiazide diuretics. CCBs and diuretics were prescribed according to the JNC 8 guidelines, whereas among ACEIs, the agents of choice were lisinopril, benazepril, fosinopril, quinapril, ramipril, and trandolapril. Among BBs, the agents of choice were metoprolol, nebivolol, propranolol, carvedilol, bisoprolol, and labetalol (Nguyen et al., 2012).
With regard to comorbidities, according to the JNC 8 guidelines, the treatment of choice for diabetes was ACEI/ARBs, CCBs, and diuretics. But in our study, CCBs, BBs, and diuretics were given. This is similar to the study conducted by Philip et al. (2016), in which amlodipine, a CCB was commonly prescribed. ACEIs were not prescribed and BBs which was not mentioned in the algorithm was prescribed. The treatment of choice for CAD, according to the JNC 8 guidelines, was ACEI, BB, diuretic, and CCB. The same was prescribed in our study also and in another study (Kaiser et al., 2014). There was no deviation in the dose or frequency from the guidelines.
Overall, BBs were prescribed for 260 patients, in combination therapy for patients with or without comorbidities. Also among the BBs, metoprolol was the choice of drug as per the JNC 8. But in our study, atenolol was commonly prescribed among BBs, which was not in accordance with the JNC 8 guidelines. There was 27.5% deviation from the JNC 8 guidelines. The reason for this deviation could be that this study was conducted in a government hospital, where drugs were given free of cost. Drugs with lesser costs would have been preferred in this hospital.
Limitations of the study
Since this was a prospective observational study, the clinical outcome could not be assessed. Moreover, since this study was carried out in a government hospital, where drugs were given free of cost, the healthcare cost assessment was not carried out.
Future directions
- Multicentric studies should be conducted in a large population.
- Follow-up should be carried out to assess the clinical outcome.
- Healthcare costs should be analyzed.
CONCLUSION
Our study population was prescribed mostly with dual drug therapy combination in which BBs and CCBs were mostly used. But according to the JNC 8 guidelines, BBs are not among the initial recommended drug classes. The treatment pattern in hypertensive patients was deviated, which can lead to other complications. Optimizing the treatment pattern in accordance with standard treatment guidelines will decrease the risk of complications. But other factors, like patient’s preference and side effects, may have an influence on the selection of drugs.
ACKNOWLEDGMENTS
The author thanks the patients who willingly participated in the study.
AUTHOR CONTRIBUTIONS
All authors made substantial contributions to conception and design, acquisition of data, or analysis and interpretation of data; took part in drafting the article or revising it critically for important intellectual content; agreed to submit to the current journal; gave final approval of the version to be published; and agree to be accountable for all aspects of the work. All the authors are eligible to be an author as per the international committee of medical journal editors (ICMJE) requirements/guidelines.
AVAILABILITY OF DATA AND MATERIALS
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
CONFLICT OF INTEREST
The authors do not have any conflicts of interest.
FUNDING
None.
REFERENCES
Almas A, Salik RI, Ehtamam A, Khan AH. Spectrum of antihypertensive therapy in south Asians at a tertiary care hospital in Pakistan. BMC Res Notes, 2011; 4:318. CrossRef
Anchala R, Kannuri NK, Pant H, Khan H, Franco OH, Di Angelantonio E, Prabhakaran D. Hypertension in India: a systematic review and meta-analysis of prevalence, awareness, and control of hypertension. J Hypertens, 2014; 32(6):1170–7. CrossRef
Arshad V, Samad Z, Das J, Almas A, Rashid N, Virani SS, Bloomfield GS, Jafar TH, Ahmed B. Prescribing patterns of antihypertensive medications in low- and middle-income countries: a systematic review. Asia Pac J Public Health, 2021; 33(1):14–22. CrossRef
Buang NFB, Rahman NAA, Haque M. Knowledge, attitude and practice regarding hypertension among residents in a housing area in Selangor, Malaysia. Med Pharm Rep, 2019; 92(2):145–52. CrossRef
Burnier M, Egan BM. Adherence in Hypertension. A review of prevalence, risk factors, impact, and management. Circ Res, 2019; 124(7):1124–40. CrossRef
Chandra S, Ubale A, Bhosle D, Jayabhaye D, Kaur S. A study of prescription pattern of the pharmacotherapy of patients of hypertension at a tertiary care hospital, Aurangabad, Maharashtra, India. Int J Basic Clin Pharmacol, 2019; 8:1599–604. CrossRef
Cubrilo-Turek M. Hypertension and coronary heart disease. EJIFCC, 2003; 14(2):67–73.
Das SK, Sanyal K, Basu A. Study of urban community survey in India: growing trend of high prevalence of hypertension in a developing country. Int J Med Sci, 2005; 2(2):70–8. CrossRef
Datta S. Use of antihypertensives in patients having associated renal parenchymal disorders: cross sectional prescription pattern study in a tertiary care hospital. Int J Pharm Sci Drug Res, 2011; 3(3):256–9.
Datta S, Sharma C. Prescribing pattern of antihypertensives in patients having comorbid ischemic heart disease: study in a tertiary care hospital. J Pharm Res, 2010; 3(9):2142–4.
Fuchs FD, Whelton PK. High blood pressure and cardiovascular disease. Hypertension, 2020; 75(2):285–92. CrossRef
Gupta R, Guptha S. Strategies for initial management of hypertension. Indian J Med Res, 2010; 132(5):531–42.
Gupta R, Guptha S, Sharma KK, Gupta A, Deedwania P. Regional variations in cardiovascular risk factors in India: India heart watch. World J Cardiol, 2012; 4:112–20. CrossRef
Hernandez-Vila E. A review of the JNC 8 blood pressure guideline. Tex Heart Inst J, 2015; 42(3):226–8. CrossRef
Jain S, Upadhyaya P, Goyal J, Kumar A, Jain P, Seth V, Moghe VV. A systematic review of prescription pattern monitoring studies and their effectiveness in promoting rational use of medicines. Perspect Clin Res, 2015; 6(2):86–90. CrossRef
James PA, Oparil S, Carter BL, Cushman WC, Dennison-Himmelfarb C, Handler J, Lackland DT, LeFevre ML, MacKenzie TD, Ogedegbe O, Smith SC, Svetkey LP, Taler SJ, Townsend RR, Wright JT, Narva AS, Ortiz E. 2014 Evidence-based guideline for the management of high blood pressure in adults: report from the panel members appointed to the eighth joint national committee (JNC 8). JAMA, 2014; 311(5):507–20. CrossRef
Kaiser EA, Lotze U, Schäfer HH. Increasing complexity: which drug class to choose for treatment of hypertension in the elderly? Clin Interv Aging, 2014; 9:459–75. CrossRef
Lawes CMM, Vander Hoorn S, Rodgers A. International society of hypertension. Global burden of blood-pressure-related disease, 2001. Lancet, 2008; 371(9623):1513–8. CrossRef
Lionakis N, Mendrinos D, Sanidas E, Favatas G, Georgopoulou M. Hypertension in the elderly. World J Cardiol, 2012; 4(5):135–47. CrossRef
Mills KT, Bundy JD, Kelly TN, Reed JE, Kearney PM, Reynolds K, Chen J, He J. Global disparities of hypertension prevalence and control: a systematic analysis of population-based studies from 90 countries. Circulation, 2016; 134(6):441–50. CrossRef
Mohd AH, Mateti UV, Konuru V, Parmar MY, Kunduru BR. A study on prescribing patterns of antihypertensives in geriatric patients. Perspect Clin Res, 2012; 3(4):139–42. CrossRef
Nagappa B, Thekkur P, Majella MG, Nair D, Ramaswamy G, Chinnakali P. Failure to achieve goal blood pressure and its associated factors among hypertensive patients registered in a primary health centre in South India. J Family Med Prim Care. 2018; 7:81–6. CrossRef
Neal B, MacMahon S, Chapman N. Effects of ACE inhibitors, calcium antagonists, and other blood-pressure lowering drugs: Results of prospectively designed overviews of randomised trials. Blood pressure lowering treatment trialists’ collaboration. Lancet, 2000; 356(9246):1955–64. CrossRef
Nguyen QT, Anderson SR, Sanders L, Nguyen LD. Managing hypertension in the elderly: a common chronic disease with increasing age. Am Health Drug Benefits, 2012; 5(3):146–53.
Pavani V, Manasa C, Ramya KT, Mihir YP, Nalini M. Study of prescribing patterns of antihypertensive drugs. Int J Pharm Bio Sci, 2012; 2(2):317–27.
Philip R, Drisyamol KA, Mathew M, Reddy VLT, Mahesh NM, Krishnamurthy MS. Prescribing patterns of antihypertensive drugs in geriatric population in tertiary care hospital. Int J Pharmacol Res, 2016; 6(3):114–9.
Ramakrishnan S, Zachariah G, Gupta K, Shivkumar Rao J, Mohanan PP, Venugopal K, Sateesh S, Sethi R, Jain D, Bardolei N, Mani K, Kakar TS, Kidambi B, Bhushan S, Verma SK, Bhargava B, Roy A, Kothari SS, Gupta R, Bansal S, Sood S, Nath RK, Tyagi S, Gupta MD, Girish MP, Kalra IPS, Wander GS, Gupta S, Mandal S, Senguttuvan NB, Subramanyam G, Roy D, Datta S, Ganguly K, Routray SN, Mishra SS, Singh BP, Bharti BB, Das MK, Kumar S, Goswami KC, Bahl VK, Chandra S, Banerjee A, Guha S, Deb PK, Chopra HK, Deedwania P, Seth A, CSI-Great India BP Campaign Investigators. Prevalence of hypertension among Indian adults: results from the great India blood pressure survey. Indian Heart J, 2019; 71(4):309–13. CrossRef
Reshma SR, Narendranath S, Somashekar HS, Keerthi SJ, Halemani SS, Kumar MN. Prescribing pattern of antihypertensives in geriatric and non geriatric individuals – a comparative study. Int J Pharm Bio Sci, 2012; 3(2):320–26.
Sharma A, Badwal TK, Gupta V, Rathore MS, Chhabra M, Gaur A. Drug utilization study on hypertensive patients and assessment of medication adherence to Jnc-8 guidelines in North Indian Tertiary Care Hospital: a cross-sectional study. Adv Res Gastroenterol Hepatol, 2018; 9(1):555751. CrossRef
Singh S, Shankar R, Singh GP. Prevalence and associated risk factors of hypertension: a cross-sectional study in Urban Varanasi. Int J Hypertens, 2017; 2017:5491838. CrossRef
Sumit B, Umesh S, Mamta S, Jyoti K, Prakash B. Prevalence, awareness, treatment and control of hypertension among the people above 15 years in rural area Nagpur Maharashtra – a cross sectional study. Natl J Community Med, 2012; 3:213–7.