INTRODUCTION
Notwithstanding the advancement in modern medicines and health technologies, the use of traditional health supplement products (HSPs) still prevails particularly among patients with chronic diseases. HSP is defined as any manufactured dietary supplement product, including supplement to the diet, and contains one or more dietary ingredients, such as vitamins, minerals, herbs or other botanicals, amino acids, and other substances or their constituents, consumed for general well-being (Abdulla et al., 2019; Gardiner et al., 2008). HSPs must be marketed in various dosage forms, such as tablet, capsule, powder, and liquid formulation (Zubrova et al., 2020). A recent study revealed that 42% of preoperative patients in the Czech Republic were consuming dietary supplements (Zubrova et al., 2020). Meanwhile, approximately 43% of Australian adults were found to have consumed at least one dietary supplement product in the past 14 days (O’Brien et al., 2017).
In 2017, the sales of HSPs achieved USD 128 billion globally (Baltazar-Martins et al., 2019). The sales of HSPs in Malaysia was rapidly growing from USD 488 million in 2014 to USD 730 million in 2019 (Lim, 2020). Meanwhile, the expenditure recorded on HSP use in the United States was USD 36.7 billion in 2014, and USD 2 billion and USD 2.6 billion were specifically on supplements for weight loss and muscle building, respectively, in 2015 (Austin et al., 2017). Indeed, the use of HSPs was found among elderly people who consumed various prescription medications for multiple comorbid conditions (Bailey et al., 2010), as well as in children and adolescents (Liu et al., 2019; Mohammadbeigi et al., 2020; Namazi et al., 2019). The monthly prevalence of HSP utilization was recorded as 65.3% among Iranian female high school students (Mohammadbeigi et al., 2020), whereas 20.4% of primary school students in Hunan, China, were found to have used dietary supplements (Liu et al., 2019).
Zooming to Malaysia, HSPs are gaining a high level of public acceptance. According to the national health and morbidity survey conducted in 2003 and 2014 throughout Malaysia, there was an increase in the use of HSPs among adults (Institute for Public Health, 2014). The prevalence of vitamins and mineral supplements usage had increased from 23.94% in 2003 to 28.05% in 2014. Besides, a more drastic increment was found in the prevalence of food supplement utilization between 2003 (24.79%) and 2014 (34.02%) (Institute for Public Health, 2014). Vitamin C, multivitamins, calcium, and vitamin B complex were the most commonly used vitamin and mineral supplements in Malaysia. Conversely, the most popular food supplements among Malaysian were fish oil, royal jelly, spirulina, and collagen (Institute for Public Health, 2014).
The majority of Malaysian consumers were single supplement users and most of them were living in urban areas. The main reasons for HSP use were to improve the general well-being and to act as an energy booster (Institute for Public Health, 2014). The consumption of HSPs among adolescences was higher than that among adults in Malaysia (Sien et al., 2014). The usage of vitamin and mineral supplements among adolescences was 54.1%, while the food supplement intake was 40.2% (Sien et al., 2014). Considering the use of herbal remedies for health maintenance among the population in Malaysia, a previous study revealed that the prevalence was as high as 29.6% (Siti et al., 2009). Besides, the prevalence of Malaysian most commonly used herb-based application, beauty, and hygiene products for health problems was 23.6% (Siti et al., 2009). Besides, a recent survey among Malay women in Malaysia found that 55.5% of them used herbs for general health and specific women problems (Tengku Mohamad et al., 2019).
All the HSPs marketed in Malaysia need to be registered with the National Pharmaceutical Regulatory Agency with a compulsory security label and registration number on the outer packaging (National Pharmaceutical Regulatory Division, 2020). Nevertheless, previous studies revealed that substandard and falsified unregistered HSPs were found in the market (National Pharmaceutical Regulatory Division, 2020; Ting et al., 2018b). These products are possibly adulterated with pharmaceutical substances which could produce the desired pharmacological action and outcome (Ting et al., 2018b). According to the adulterated product samples analyzed by the Sarawak Pharmacy Enforcement Branch from 2015 to 2017, adulterated traditional products were found to be the highest (58.7%), followed by food products (33.3%) and supplements (8.0%) (Sarawak Pharmacy Enforcement Branch, 2018). Steroids remain the highest adulterants found in all the samples, with a percentage of 32.2%, followed by sex stimulants, non-steroidal anti-inflammatory drugs (NSAIDs), and others. Furthermore, most (66.2%) of the adulterated samples were originated from Malaysia (Sarawak Pharmacy Enforcement Branch, 2018). Inappropriate and long-term use of such pharmaceutical substances could lead to catastrophic and unwanted side effects and interactions. Therefore, it is essential for consumers to ensure the product safety by checking the product registration status before use.
Many studies have been conducted to explore factors influencing the use of HSPs, but there were variations in the study findings. Generally, factors influencing the use of HSPs were found to be and are not limited to gender, age, ethnic, marital status, education level, body mass index, physical activity, smoking, medical history, and income (Aziz and Tey, 2009; Mohammadbeigi et al., 2020; O’Brien et al., 2017). These variations are specifically based on the study population, as different populations would have different cultures, lifestyle, and beliefs. Hence, there is a need to explore factors that would influence the use of HSPs particularly among patients in rural areas of Sarawak, East Malaysia. The population in Sarawak is unique because of its diverse native ethnic groups, for instance, the Bidayuh, Iban, and Melanau. In the urban areas of Sarawak, the prevalence of herbal medicine use was 25% based on a previous study (Lee et al., 2007). Nevertheless, there is limited newer research on the prevalence of HSP utilization among the Malaysian population. Additionally, previous studies in Malaysia did not properly address the prevalence of concomitant use of prescribed medicines and HSPs, as well as the practices, perceptions, and factors which lead to the use of HSPs among the rural population. Therefore, the primary objective of this study is to assess the prevalence of HSP use among patients with chronic illnesses from the rural areas of Sarawak. Additionally, the commonly used HSPs among these populations were assessed. This study also explores the practices and perceptions of the patients toward HSP. The association between socio-demographic characteristics of patients and the use of HSPs was assessed as well. Currently there are no established Malaysian guidelines on the concomitant use of HSPs and prescribed medicines, however, this study’s findings will help in the development of such guidelines.
METHODS
This was a multicenter cross-sectional study conducted from June to August 2018 in the outpatient pharmacy of seven districts’ nonspecialist government hospitals in Sarawak, namely Hospital Saratok, Hospital Bau, Hospital Kanowit, Hospital Marudi, Hospital Dalat, Hospital Betong, and Hospital Daro. This study was approved by the Medical Research and Ethics Committee, Ministry of Health Malaysia (approval number NMRR-17-943-35773). The sample size was calculated based on the primary objective of the study by using a sample size formula from the prevalence study. Based on the previous prevalence of HSPs used among the Malaysian population of around 30% (Institute for Public Health, 2014), a total number of 323 patients would provide a representative sample size with 95% confidence interval and 5% margin of error.
Convenience sampling was used in the recruitment of patients. Patients with chronic diseases who consumed three or more prescribed medicines were included. Patients who actively consumed HSPs were assessed on their practices and perceptions of HSP use. The inclusion criteria for HSPs were those which demonstrated pharmacologic action used to produce a therapeutic effect or those that do not have a documented pharmacologic action which can affect the absorption, metabolism, and disposition of other drugs (Gardiner et al., 2006). Any patient who declined the consent was excluded.
A data collection form was developed based on the objectives of the study using information from a literature review. The data collection form consisted of four parts. The first part was the patient demographic data. Part two was a questionnaire to assess the prevalence of use, practices, and perceptions of patients toward HSPs. Meanwhile, parts three and four assessed the patient’s current use of prescribed medicines and HSPs, respectively. The data collection form had gone through face and content validation by two experts (academicians from the School of Pharmaceutical Sciences, Universiti Sains Malaysia) and three practicing senior clinical pharmacists with at least 5 years of working experience in the government hospital. Briefing, training sessions, and pretesting were conducted with all the data collectors prior to the data collection. The data collectors in this study were the pharmacists from the respective hospitals involved in this study. Subsequently, a pilot study was conducted with 32 patients, with eight patients each from Hospital Marudi, Hospital Betong, Hospital Daro, and Hospital Dalat. With the collected data, the internal consistency of the questionnaire in the data collection form was tested with Cronbach’s alpha, and the results were 0.825 for questions that explored the practices of HSPs and 0.780 for questions that focused on patient’s perception of HSPs.
The patients who collected medications from the outpatient pharmacy department of the selected hospitals were screened by the data collectors. Those who fulfilled the inclusion criteria were selected and called to the counseling room. The objectives of the study were explained and the patients were asked for consent to participate in the study. Subsequently, the data collection form was distributed through face-to-face interviews with the patients. In order to reduce recall bias, this study only included the HSPs mentioned by the patients which they were actively using. Explanations were given by the data collectors by using layman’s term so that the patients would understand the definition of HSPs in this study. Actively used HSP was defined as HSPs that were currently consumed by the patients. The patients were requested to bring along their HSPs for identification if they cannot recall the products’ names. The data collection form was filled in by the data collectors. Additionally, patients’ cell phone numbers were recorded. Hence, information that was missed out during the interview was obtained later through telephone calls or during the next medication collection date.
The data were entered into the Statistical Package for the Social Sciences SPSS® version 21.0 for analysis. Descriptive statistics were used to report the demographic data, prevalence, practices, and perceptions of the patients toward HSPs. The common HSPs used and their indications were tabulated. Bivariate logistic regression was used to explore the association of all the socio-demographic data with the use of HSPs.
RESULTS
Patients’ demographic
A total of 364 patients were approached to participate in the present study. Nine patients who refused to participate and another five patients with missing data were excluded. The remaining 350 patients participated in this study. The mean age and body mass index of the respondents were 55.6 ± 11.7 years and 25.60 ± 4.95 kg/m2, respectively. Slightly more than half (56.0%) of the respondents were female. The ethnicity of the majority (32.3%) of the respondents was Iban, and most (54.6%) of the respondents’ education levels were lower than secondary school. The respondents were mostly nonsmokers (73.1%) and nonalcohol drinkers (72.0%). The majority of them (41.1%) were physically active with more than three times of physical activity per week. Considering the socio-demographics, about half (49.4%) of them have a monthly household income of less than RM 830 (USD 199.44). Most of the respondents were diagnosed with hypertension (86.9%), diabetes mellitus (52.9%), and dyslipidemia (34.3%) (see Table 1).
 | Table 1. Demographic characteristics of patients. [Click here to view] |
Patients’ practices of HSP
A total of 150 respondents (42.9%) have experience in consuming HSPs. However, the prevalence of active HSP users was 24.0% (n = 84). Among the active users, the majority (41.7%; n = 35) were from the high household income group, while 28.6% (n = 24) and 29.8% (n = 25), respectively, were from moderate- and low-income groups. The 150 respondents were investigated on their practices of HSP. Around half (51.4%) of the respondents have experience in consuming prescribed medicines together with HSPs immediately prior to or after their prescribed medicines consumption without any intentional time spacing. When specifically assessing the current active HSP users, 64.3% (n = 54) of them have always used HSPs concomitantly with prescribed medicines. Nevertheless, approximately half (52.0%) of the respondents indicated that they never consult doctors or pharmacists before consuming any HSP. Besides, 54.0% of the respondents never informed doctors or pharmacists about their use of HSPs. The majority of respondents (72.0%) never check the product registration status before using HSPs. Most of the respondents claimed that they never (75.3%) change the regime of the prescribed medicines because of HSP use, and 56.7% followed the dosage regime instruction of the HSP use (see Table 2).
Patients’ perceptions of HSP
All the respondents (n = 350) were assessed on their perceptions of HSP. Only 24.3% of the respondents perceived all HSPs marketed in Sarawak as safe to be consumed. Similarly, only 27.5% of respondents believed that all HSPs sold in Sarawak have approval from the Ministry of Health Malaysia. The majority of respondents expressed agreement that it is necessary to consult doctors or pharmacists before using any HSP (82.0%) and be informed about the concomitant use of HSPs and prescribed medicines (80.3%). In addition, the respondents also mostly agreed (83.7%) upon the importance of following the instruction of doctors or pharmacists on the use of HSPs (see Table 3).
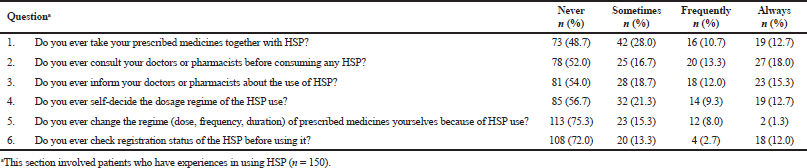 | Table 2. Practices of the use of HSPs. [Click here to view] |
 | Table 3. Perceptions of HSPs. [Click here to view] |
Factors influencing HSP consumption
When assessing the contributing factors to HSP consumption, the patient’s gender, age, body mass index, ethnicity, education level, smoking status, alcohol consumption status, physical activity, household income, and number of comorbidity diseases were initially tested by single logistic regression. The results showed that education level, smoking status, and monthly household income were statistically significantly associated with the use of HSPs. These three factors were subsequently tested in multivariate analyses and only income of the family significantly influenced the use of HSPs. Higher household income significantly led to a greater usage of HSPs. Patients with a monthly household income of more than RM 2000.00 (USD 480.59) were significantly more likely to consume HSPs as compared to the low-income group with a monthly income of RM 830.00 (USD 199.44) or less (adjusted odds ratio: 4.23; 95% CI: 2.31–7.76; p < 0.001). Those with a monthly income ranging from more than RM 830.00 (USD 199.44) to RM 2000.00 (USD 480.59) were also significantly more prone to use HSPs than the low-income group (adjusted odds ratio: 2.06; 95% CI: 1.10–3.86; p < 0.001).
HSPs consumed by the patients
The products commonly consumed by a total of 84 active HSP users are listed in Table 4. The majority (83.3%, n = 70) of them were single HSP users, while nine (10.7%) of the users consumed two products. There were only four (4.8%) HSP users who consumed three products and only one (1.2%) user who consumed four products. The mean number of HSPs used by active users was found to be 1.25 ± 0.59. The most commonly used HSP was fish oil (with vitamin E), vitamin C (with bioflavonoids), and glucosamine (with a combination of other active ingredients).
 | Table 4. HSP use and its expected medicine purpose. [Click here to view] |
DISCUSSION
The response rate in this study was 96.2% and managed to achieve the targeted sample size. Most of the respondents (69.4%) were the non-Malay native population in Sarawak and the distribution was in accordance with the demographic characteristic of the Sarawak native population for which the majorities were Iban, Bidayuh, and Melanau (Nelson et al., 2016). This was contrasted with similar studies conducted in West Malaysia which involved mainly the ethnic groups of Malay, Chinese, and Indian (Baharom et al., 2016; Ching et al., 2013). Besides, the respondents generally have lower education level and household income as compared to a previous study in Malaysia which involved urban (Lee et al., 2007) and suburban areas (Ching et al., 2013). Nearly 20% of the respondents in the present study did not receive formal education and approximately half of them have a household income lower than RM 830 per month and this was classified as a poor family according to the definition by the Malaysian government (Ministry of Health, Labor and Welfare, 2011).
Although this study specifically involved patients with chronic illnesses, the prevalence of HSP utilization was lower as compared to other studies which focused on specific disease groups, such as type II diabetes mellitus (58.5%), hypertension (62.6%), and Parkinson’s disease (83.4%) (Baharom et al., 2016; Ching et al., 2013; Ferguson et al., 2019). The low prevalence in this study could be explained by the intension of the use of the products (Abdullah et al., 2018). Approximately 40% of the HSPs were intended for general health maintenance or as energy booster rather than for disease adjunctive treatment. Additionally, the low household income among the respondents might be another reason for the low prevalence in this study. A study in Iran revealed a similar finding that dietary supplement consumption increases when there is an increment in the family income level (Mohammadbeigi et al., 2020). In the present study, only 29.8% of active HSP users were patients from low-income group. This finding might reflect the fact that the high expenditure on HSPs was a burden to chronic disease patients with a low household income. A study by Austin et al. (2017) also found that the cost of HSPs might place the low household income families at a higher risk of financial burden. Interestingly, household income was the only determining factor for the use of HSPs in the present study. This finding is in contrast with other studies where income is not the sole determining factor but multiple factors such as gender, age, body mass index, and education status were also influencing the use of HSPs (Aziz and Tey, 2009; O’Brien et al., 2017).
This study raised a concern on the concomitant use of supplement products with prescribed medicines. A high proportion of active HSP users were not consulting and disclosing such information to their healthcare providers. These findings are consistent with a recent meta-analysis which found that the patients’ rate of disclosure of such information to their healthcare providers was low (Foley et al., 2019). The major contributing factors to this problem might be that the patients were afraid of critics and lack of discussion between the healthcare providers and patients on the use of HSPs (Abdullah et al., 2018; Foley et al., 2019). This issue needs to be addressed as there are potential interactions between HSPs and prescribed medicines and which subsequently might cause unwanted effects or therapeutic failure (Tachjian et al., 2010).
The Malaysian Medicines Policy was endorsed in 2006 for which the quality use of medicines is one of the essential components (Pharmaceutical Services Division, 2013). Subsequently, the national “Know Your Medicines” campaign which aimed to improve the quality use of medicines among Malaysians was lunched (Ting et al., 2019). Various activities were conducted through this campaign which involves workshop exhibition and talks, promoting rational use of medicines through the mass media, and reviewing consumer perception and knowledge toward medicines (Ting et al., 2019). Besides, the Malaysian government requires compulsory labeling for registered HSPs with security label and registration number on the outer packaging (National Pharmaceutical Regulatory Division, 2020; Ting et al., 2018b). The consumers could verify the products’ authenticity by either vetting the security label MeditagTM Hologram (Pharmaceutical Services Division, 2015) or searching for the product registration number through the online product registration search database named “QUEST 3+ Product Search” (National Pharmaceutical Regulatory Agency, 2020). These steps are essential in avoiding consuming any unregistered or counterfeited products. However, a worrying practice was found in this study that more than 60% of the respondents did not check product registration status before consuming any HSP. This could be due to the lack of awareness about product registration (Ting et al., 2019). Surprisingly, around 40% of the respondents perceived that not all the HSPs marketed in Sarawak are safe and registered. These findings reflected that the rural population might have a lack of accessibility to the government health promotion campaign. Information on the precaution of concomitant use of HSPs with prescribed medicines, potential drug-HSP interaction, and HSP registration status is lacking among the rural population. This warranted a review of the current health promotion material and the necessity in creating better understanding of these topics. Crucial steps are needed to create better health promotion strategies in creating awareness among the patients on the safe use of HSPs. More health promotion campaigns should be organized by the Ministry of Health to highlight the potential risk of HSP adulteration and interactions with prescribed medicines and encourage patients to discuss the use of HSP with healthcare providers. This is an important step as this information is lacking in the currently available health promotion materials. Besides, more local representatives from the rural areas should be invited to be involved in the educational program, along with well-designed local native language health promotion materials to create awareness on the safe use of HSPs.
Adherence to prescribed medicines is crucial for chronic disease control (Ting et al., 2018a). Nevertheless, approximately, quarter of the patients in this study have a tendency to change the regime of the prescribed medication after the use of HSPs. This finding indicates that some patients from rural areas have not complied with the instruction of healthcare providers. In order to address this problem, the healthcare provider could take the initiative to explore more by asking patients about their use of HSPs with open-ended questions. Patients would be willing to disclose more about their use of supplement products if the healthcare provider showed interest in knowing the information (Foley et al., 2019). Additionally, all information about HSPs should be recorded in the patient record book and treated the same as other prescribed medicines. Documentation of patient’s HSP usage could alert the healthcare provider on the potential adverse effects and interaction between supplements and prescribed medicines (Ben-Sasson et al., 2020).
LIMITATIONS
There might have been a selection bias in this study due to the convenience sampling. To overcome this problem, the data were collected from multicenter facilities and with a bigger sample size. Additionally, the results were solely based on the self-reporting of the patients’ consumption of HSP, which might have introduced recall bias. However, efforts were made to avoid recall bias, whereby the patients were asked to bring along the HSPs for review in case they could not recall their HSP name. However, there was a possibility of response bias (socially desirable answers) as the interviewers were the pharmacist working in the district hospital.
CONCLUSION
The concomitant use of HSPs with prescribed medicines was prevalent among patients with chronic diseases in rural areas of Sarawak. This practice was seldom being disclosed by the patients to the healthcare providers. Educational interventions and tenacious efforts are required to instill better practice on the safe use of HSPs among patients.
ACKNOWLEDGMENTS
The authors would like to thank the Director General of Health Malaysia for the permission to publish this article.
FINANCIAL SUPPORT
This study was supported by the Bridging-Incentive Grant, Universiti Sains Malaysia [grant numbers: 304.PFARMASI.6316547].
CONFLICT OF INTEREST
The authors have no conflicts of interest in connection with this paper.
REFERENCES
Abdulla NM, Adam B, Blair I, Oulhaj A. Heavy metal content of herbal health supplement products in Dubai—UAE: a cross-sectional study. BMC Complement Altern Med, 2019; 19(1): 276; doi:10.1186/s12906-019-2693-3 CrossRef
Abdullah N, Borhanuddin B, Patah AEA, Abdullah MS, Dauni A, Kamaruddin MA, Shah SA, Jamal R. Utilization of complementary and alternative medicine in multiethnic population: the Malaysian Cohort Study. J Evid Based Integr Med, 2018; 23:1–9. CrossRef
Austin SB, Yu K, Liu SH, Dong F, Tefft N. Household expenditures on dietary supplements sold for weight loss, muscle building, and sexual function: disproportionate burden by gender and income. Prev Med Rep, 2017; 6:236–41. CrossRef
Aziz Z, Tey NP. Herbal medicines: prevalence and predictors of use among Malaysian adults. Complement Ther Med, 2009; 17(1):44–50. CrossRef
Baharom N, Shamsul Azhar S, Rotina AB. Prevalence of complementary alternative medicine use among patients with type II diabetes in Negeri Sembilan, Malaysia. Med Health, 2016; 11(2):257–66. CrossRef
Bailey RL, Gahche JJ, Lentino CV, Dwyer JT, Engel JS, Thomas PR, Betz JM, Sempos CT, Picciano MF. Dietary supplement use in the United States, 2003-2006. J Nutr, 2010; 141(2):261–6. CrossRef
Baltazar-Martins G, Brito de Souza D, Aguilar-Navarro M, Muñoz-Guerra J, Plata MDM, Del Coso J. Prevalence and patterns of dietary supplement use in elite Spanish athletes. J Int Soc Sports Nutr, 2019; 16(1):30; doi:10.1186/s12970-019-0296-5 CrossRef
Ben-Sasson M, Levy I, Ben-Arye E, Attias S, Schiff E. Dietary and herbal supplements use among patients hospitalized in internal medicine departments. Complement Ther Med, 2020; 50:102345; doi:10.1016/j.ctim.2020.102345 CrossRef
Ching SM, Vasudevan R, Zakaria ZA, Paimin F. Frequency of complementary and alternative medicine usage among Malaysian hypertensive subjects. Life Sci J, 2013; 10(4):2526–31.
Ferguson CC, Knol LL, Halli-Tierney A, Ellis AC. Dietary supplement use is high among individuals with parkinson disease. South Med J, 2019; 112(12):621–5. CrossRef
Foley H, Steel A, Cramer H, Wardle J, Adams J. Disclosure of complementary medicine use to medical providers: a systematic review and meta-analysis. Sci Rep, 2019; 9(1):1573; doi:10.1038/s41598-018-38279-8 CrossRef
Gardiner P, Graham RE, Legedza AT, Eisenberg DM, Phillips RS. Factors associated with dietary supplement use among prescription medication users. Arch Intern Med, 2006; 166(18):1968–74. CrossRef
Gardiner P, Phillips RS, Shaughnessy AF. Herbal and dietary supplement-drug interactions in patients with chronic illnesses. Am Fam Physician, 2008; 77(1):73–8.
Institute for Public Health. National Health and Morbidity Survey 2014: Malaysian Adult Nutrition Survey (MANS) Vol. II: survey findings. Ministry of Health Malaysia, Kuala Lumpur, Malaysia, 2014.
Lee PY, Taha ABA, Lin K, Ghazali SR, Almashoor SHSA. Usage of complementary and alternative medicine among primary attendees, Kuching, Sarawah, Malaysia, January-April 2004. Asia Pac Fam Med, 2007; 6(1):1–10. Available via http://www.apfmj-archive.com/afm6_1/afm52.htm (Accessed 6 September 2020).
Lim A. Cultural backgrounds influence herbal supplement purchases & two more health supplement trends in Malaysia. Joint ASEAN NETWORK 10, Singapore, 2020. Available via https://janio.asia/id/articles/malaysia-health-supplements-ecommerce-trends/ (Accessed 6 September 2020).
Liu H, Zhang S, Zou H, Pan Y, Yang Q, Ouyang Y, Luo J, Lin Q. Dietary supplement use among chinese primary school students: a cross-sectional study in Hunan province. Int J Environ Res Public Health, 2019; 16(3):374; doi:10.3390/ijerph16030374 CrossRef
Ministry of Health, Labour and Welfare. Country report: Malaysia. The 9th ASEAN & Japan High Level Officials Meeting on Caring Societies, 25 – 28 October 2011. Ministry of Health, Labour and Welfare, Tokyo, Japan, 2011. Available via https://www.mhlw.go.jp/bunya/kokusaigyomu/asean/2011/dl/Malaysia_CountryReport.pdf (Accessed 6 September 2020).
Mohammadbeigi A, Mohammadsalehi N, Moshiri E, Asgarian A, Afrashteh S, Khazaei S, Ansari H. Pattern of dietary supplement consumption among Iranian high school girls and related factors. Sri Lanka J Child Health, 2020; 49(1):41–7. CrossRef
Namazi N, Kelishadi R, Heshmat R, Motlagh ME, Sanaei M, Shafiee G, Ziaodini H, Beshtar S, Taheri M, Aminaee T, Qorbani M, Shahrzad, MK. Determinants of taking dietary supplements in Iranian children and adolescents: the CASPIAN-V study. J Diabetes Metab Disord, 2019; 18(2):409–17. CrossRef
National Pharmaceutical Regulatory Agency. QUEST3+ Products Search. Ministry of Health Malaysia, Kuala Lumpur, Malaysia, 2020. Available via https://npra.gov.my/index.php/en/consumers/information/products-search.html (Accessed 4 September 2020).
National Pharmaceutical Regulatory Division. Drug registration guidance document. Second edition - September 2016, July 2020 Revision. Ministry of Health Malaysia, Petaling Jaya, Malaysia, 2020.
Nelson J, Muhammed N, Rashid RA. Native customary rights: does it hold the future of Sarawak’s natives? J For Environ Sci, 2016; 32(1):82–93. CrossRef
O’Brien SK, Malacova E, Sherriff JL, Black LJ. The prevalence and predictors of dietary supplement use in the Australian population. Nutrients, 2017; 9(10):1154. CrossRef
Pharmaceutical Services Division. Malaysian National Medicines Policy (MNMP): First Term Performance Report (2007-2011). Ministry of Health Malaysia, Petaling Jaya, Malaysia, 2013.
Pharmaceutical Services Division. New hologram Meditag. Ministry of Health Malaysia, Petaling Jaya, Malaysia, 2015. Available via https://www.pharmacy.gov.my/v2/en/content/new-hologram-meditag.html (Accessed 4 September 2020).
Sarawak Pharmacy Enforcement Branch. Sarawak Pharmacy Enforcement Sampling Report (2015-2017). Pharmacy Enforcement Branch, State Health Department, Kuching, Malaysia, 2018.
Sien YP, Sahril N, Abdul Mutalip MH, Zaki NA, Abdul Ghaffar S. Determinants of dietary supplements use among adolescents in Malaysia. Asia Pac J Public Health, 2014; 26(5 Suppl):36S–43S. CrossRef
Siti ZM, Tahir A, Farah AI, Fazlin SM, Sondi S, Azman AH, Maimunah AH, Haniza MA, Siti Haslinda MD, Zulkarnain AK, Zakiah I, Zaleha WC. Use of traditional and complementary medicine in Malaysia: a baseline study. Complement Ther Med, 2009; 17(5–6):292–9. CrossRef
Tachjian A, Maria V, Jahangir A. Use of herbal products and potential interactions in patients with cardiovascular diseases. J Am Coll Cardiol, 2010; 55(6):515–25. CrossRef
Tengku Mohamad TAS, Islahudin F, Jasamai M, Jamal JA. Preference, perception and predictors of herbal medicine use among Malay women in Malaysia. Patient Prefer Adherence, 2019; 13:1829–37. CrossRef
Ting CY, Ahmad Zaidi Adruce S, Hassali MA, Ting H, Lim CJ, Ting RS, Abd Jabar AHA, Osman NA, Shuib IS, Loo SC, Sim ST, Lim SE, Morisky DE. Effectiveness and sustainability of a structured group-based educational program (MEDIHEALTH) in improving medication adherence among Malay patients with underlying type 2 diabetes mellitus in Sarawak State of Malaysia: study protocol of a randomized controlled trial. Trials, 2018a; 19(1):310; doi:10.1186/s13063-018-2649-9 CrossRef
Ting CY, Ang WC, Ahmad K, Loo SC, Hassali MA, Alshaari AH, Jabar A. Awareness on know your medicine campaign and the appropriate use of medicines among Sarawak consumers. J Pharm Health Serv Res, 2019; 10(3):381–4. CrossRef
Ting CY, Loo SC, Sim ST, Tee EC, Hassali MA, Abd Jabar AHA, Adruce SAZ, Talin BA. Unregistered medical products detected by Malaysia’s Pharmacy Enforcement Division during routine inspection: a cross-sectional study among selected mainstream medicines’ retailers in the State of Sarawak. Pharm Med, 2018b; 32(2):143–8. CrossRef
Zubrova J, Pokladnikova J, Draessler J. The use of dietary supplements by patients in the pre-operative period in the Czech Republic. Int J Clin Pharm, 2020; 42(5):1304–10; doi:10.1007/s11096-020-01080-7 CrossRef