INTRODUCTION
Bisphosphonates (BPs) are pyrophosphate analogs that are prescribed as first-line drugs for the prevention and treatment of bone disorders such as Paget’s disease, hypercalcemia of malignancy, osteopenia, and osteoporosis (Drake et al., 2008; Ezra and Golomb, 2000). BPs act by inhibiting the mevalonate pathway in bone resorption, which is a crucial step in the bone remodeling process (Lambrinoudaki et al., 2006; Schenk et al., 1986; Van Beek et al., 2003). The majority of orally administered BPs such as alendronate (ALD) has serious gastrointestinal adverse conditions such as irritation of the mucosal wall of GIT, gastric ulcers, and esophagitis. Moreover, ALD has very low (not more than 2%) bioavailability, and its systemic absorption is further hampered by the presence of food. To avoid all aforementioned side effects, the dose of ALD is advised to be taken empty stomach in the morning in an upright sitting position with a big glass of water. This practice helps in reducing the irritation of mucosal lining but can be hard to comply with by elderly patients (Graham, 2002; Naniwa et al., 2008; Porras et al., 1999). This crisis raises the need for the development of a carrier system and/or a choice of a different route that can efficiently improve the bioavailability of ALD, escaping its oral side effects and keeping its osteogenic activity intact.
Drug molecules currently administered via the transdermal route fall within a narrow range of molecular weight, typically less than 500 g/mol (Benson, 2005; Marwah et al., 2014). Thus, ALD (molecular weight 325 g/mol) can be the potential candidate for transepidermal delivery. Transdermal application has numerous potential benefits over oral delivery such as evading GIT side effects, comfort in an application, and ultimately better patient compliance (Katsuni et al., 2012), especially the elderly patients in this case. The key step in the transdermal application of ALD, a hydrophilic candidate, is delivering it through stratum corneum in an adequately high amount to exert therapeutic effect (Choi et al., 2008; Yano et al., 1986). Many research studies have explored and established microemulsions as an effective carrier to deliver polar drugs across the skin for local and systemic effects (Alkrad et al., 2019; Kaur et al., 2018; Kumbhar et al., 2020; Talhouni et al., 2019). The mounting attention given to microemulsion, as a delivery system, stems from some of their peculiar characteristics such as the larger surface area of the inner dispersed phase which gives better drug release, improved penetration capacity across biological membranes, and high stability (Hashem et al., 2011; Nastiti et al., 2017; Sapra et al., 2014). Besides, the strategic selection of components of the microemulsion can further enhance the penetration of drugs across the skin without causing any skin irritation. In this study, isopropyl myristate (IPM) is selected as an oil phase as its usage in the transdermal system has add-on benefit being biocompatible permeation enhancer (Furuishi et al., 2019; Kantaria et al., 2003; Zidan et al., 2017). Aerosol OT (bis-2-(ethylhexyl) sulfosuccinate, AOT) has been comprehensively used with IPM to formulate transdermal microemulsions due to its non-irritant properties (Anjum et al., 2016; Changez and Varshney, 2000; Dib et al., 2020; Liebig et al., 2018). AOT facilitates solubilization of a sizable extent of water with oil even when the aqueous phase has higher drug loading. Moreover, the synergistic influence on water solubilization ability was observed when AOT was used in combination with a nonionic surfactant like labrasol/tweens (Kantaria et al., 2003; Yanyu et al., 2012).
Taking into account the abovementioned specifics, we conjectured that the encapsulation of ALD in IPM/AOT/labrasol w/o microemulsion may result in enhanced permeation of ALD across the epidermal barrier and can achieve greater bioavailability than oral administration of the same. Furthermore, we hypothesized that ALD microemulsion can demonstrate osteogenic activity on osteoblastic cells.
MATERIALS AND METHODS
Materials
ALD was received as a gift sample from Aurobindo Pharmaceuticals, Hyderabad, India. IPM and dioctyl sulfosuccinate (AOT) were purchased from Sigma Aldrich, Mumbai, India. Labrasol was generously donated by Gattefosse, India. All the solvents used were of high performance lipid chromatography (HPLC) grade, and chemicals were of analytical grade. Freshly collected Milli-Q water (Millipore, Billerica, MA) was used in the preparation of aqueous mobile phase of HPLC analysis.
Construction of pseudo-ternary phase diagrams
To record the concentration range of each microemulsion component, pseudo-ternary phase diagrams were constructed with the titration method. Five phase diagrams, with IPM as oil, were studied with 1:1, 2:1, 3:1, 4:1, and 5:1 weight ratios of AOT (surfactant) to labrasol (co-surfactant). The ratio of surfactant mixture (AOT + labrasol) to oil was varied at 1:9, 2:8, 3:7, 4:6, 5:5, 6:4, 7:3, 8:2, and 9:1 for each phase diagram. An aqueous solution of the drug was added in a dropwise manner to the surfactants and oil mixture under moderate magnetic stirring, and a solution turning slight turbid is considered as an endpoint (Yanyu et al., 2012).
Preparation of microemulsion
The compositions of microemulsion with varying concentrations of components were selected from the phase diagram. The microemulsion was prepared by gradually titrating a weighed amount of oily mixture of IPM, AOT, and labrasol with an aqueous solution of ALD (Sintov and Botner, 2006). The microemulsion was formed spontaneously at room temperature as a clear monophasic liquid.
Physical appearance
The prepared microemulsion (blank and drug-loaded) was scrutinized through visual inspection of their homogeneity, phase separation (if any), and consistency.
Globule size
The microemulsion was characterized for average globule size with Malvern Zetasizer 7.12 (Malvern Instruments Ltd., Malvern, UK).
Transmission electron microscopy (TEM)
The morphology of microemulsion was observed by TEM (TEM JEM-2010-Japan Electron Optics Laboratory Company, Tokyo, Japan). A single drop of optimized formulation was put on a copper grid and then dried at room temperature. Pictures were recorded by TEM with suitable magnification.
Drug content
The drug content in microemulsion was determined by the following previously reported multistep derivatization process for ALD and analyzing a sample by high-performance liquid chromatography (Meng et al., 2010).
Refractive index
The refractive indices for both blank and ALD microemulsion were determined using a refractometer (Fisher Scientific, Japan) in triplicates.
Viscosity
The viscosities of blank and drug-loaded microemulsions were measured with a Brookfield cone and plate rheometer (Brookfield Engineering, Middleborough, MA) with a No. 1 rotor set at 60 rpm. The temperature was controlled at 25°C.
Density
The density of blank and ALD added microemulsion was measured using a pycnometer. Precisely measured 10 ml of sample microemulsion was taken in a container and accurately weighed, and the density was calculated. The experiment was carried out in triplicates for each sample.
Electrical conductivity
The electrical conductivity of the microemulsion samples was measured by Riac CM/100 conductivity meter (Yellow Springs Instruments, Yellow Springs, OH). The tests were performed in triplicates at room temperature.
DSC
DSC analysis was performed (STARe, Mettler Toledo GmbH Analytical, Giessen, Germany) to examine the thermal behavior of water in the microemulsion. The samples of blank and ALD loaded microemulsions were accurately weighed (5–10 mg) into 40-0 μl aluminum pans, and the pans were sealed, kept under sub-zero temperature (−70ºC) overnight, and scanned between −40°C and 150°C, at a heating rate of 1°C/minute. A blank sealed aluminum pan was used as a reference.
Thermodynamic stability studies
Heating cooling cycle
Blank and ALD microemulsions went through 6 cycles, where they were kept at 40 ± 2ºC and then at 4 ± 2ºC for at least 48 hours (Hamed et al., 2019).
Centrifugation test
Microemulsions underwent centrifugation at 3,500 rpm for 30 minutes and were scrutinized for any drug precipitation or phase separation or any color/consistency changes (Hamed et al., 2019).
Freeze-thaw cycles
Formulations were stored between −25 ± 2oC and 25 ± 2ºC at least for 48 hours and were examined for any drug precipitation or phase separation or any color/consistency changes (Hamed et al., 2019).
Stability studies
The physical and chemical stability of ALD-loaded microemulsion was studied by keeping samples at 25 ± 2oC, relative humidity 60 ± 5% for 3 months. The samples were withdrawn at selected time intervals and were tested visually for globule size. Drug content was assessed by HPLC (Pakpayat et al., 2009).
In vitro permeation
In vitro permeation profiles were evaluated through excised rat skin, mounted on Franz diffusion cells (area 0.95 cm²) with stratum corneum area facing toward donor chamber. Accurately 3–4 ml of phosphate buffer solution (phosphate buffer saline (PBS) pH 7.4) was filled in the receiver section of diffusion cells maintained at 32 ± 0.5°C and was stirred magnetically at 300 rpm. Precisely measured samples of microemulsion (dose: 0.1, 0.5, or 1 mg of ALD) were placed in the donor compartment above the stratum corneum side of rat skin. The permeation profiles of microemulsions were compared with an aqueous solution of ALD (dose: 1 mg) placed in a separate diffusion cell. The aliquots of acceptor media (500 μl) were collected at regular intervals, and each aliquot was substituted with an equal volume of fresh pre-heated PBS. An ALD concentration was determined using the reverse phase HPLC method, and the quantity of ALD permeated was determined (Meng et al., 2010).
In vivo pharmacokinetic studies
Animals were divided into five groups (n = 6). Hairs were removed from the skin (about 10 cm²) of three groups of rats. These groups received ALD microemulsion transdermally at a dose of 30, 25, or 20 mg/kg. The fourth group of rats received an ALD solution orally at a dose of 30 mg/kg. Alendronate solution (1 mg/kg) was administered intravenously to rats in the fifth group. At pre-determined time intervals, the blood samples were collected, and plasma was isolated instantly by centrifugation at 3,000 rpm for 15 minutes. Alendronate plasma concentrations were measured by HPLC (Meng et al., 2010). Pharmacokinetic parameters were calculated for each individual set of data by noncompartmental analysis using WinNonLin version 4 (Pharsight, Mountain View, CA). The absolute bioavailability was evaluated for transdermal as well as oral delivery of ALD.
MTT assay
The influence of ALD (pure drug and microemulsion) on cellular viability was studied with MG-63 osteoblast-like cells (NCCS, Pune, India) by culturing them as defined earlier (Kim et al., 2012). Cells were collected after reaching confluency and plated in 96-well plates. Cells were incubated at 37ºC in the incubator with 5% CO2 and were washed with PBS. 3-(4,5-dimethylthiazol-2-yl)-2,5-diphenyl tetrazolium bromide (MTT) assay was performed by placing cells into each well of 96-well plate, incubating them overnight, adding 0.5 mg/ml of MTT into each well, and further incubating them for 4 hours at 37 ± 0.5ºC. The culture medium was then aspirated, and the produced formazan crystals were dissolved by adding 150 μl of dimethyl sulfoxide (DMSO) (Ha et al., 2003). The supernatant was collected, and the colorimetric changes were measured at 490 nm in a microplate reader. MTT assay was carried out with four groups: control, ALD solution, blank microemulsion, and ALD microemulsion. The results are represented as the percentage optical density of samples considering the control group as 100%.
Alkaline phosphatase (ALP) activity
ALP activity was analyzed in four different groups: control, ALD solution, blank microemulsion, and ALD microemulsion. The MG-63 cells were plated in well plates at a density of 1 × 105 cells. After overnight incubation, ALD microemulsion/ ALD pure solution/ blank microemulsion was added, and the cultures were continued for 3, 7 and, 10 days. Cells were lysed after completion of the study, cell lysates were then centrifuged for 3 minutes (15,000 rpm, 4 ± 0.5ºC), and the supernatants were separated. 1N NaOH was added after 30 minutes of incubation of supernatant with p-nitrophenyl phosphate (30 minutes, 37 ± 0.5ºC). ALP activity was determined by measuring the conversion of p-nitrophenyl phosphate to p-nitrophenol. An optical density was determined at a wavelength of 405 nm.
Mineralization
Mineralization study was carried out in four different groups: control, ALD solution, blank microemulsion, and ALD microemulsion. The MG-63 cells were plated in 24-well tissue culture plates (density 1 × 105 cells). After overnight incubation, blank microemulsion/ALD microemulsion/ALD pure solution was added, and the plates were kept for incubation for either 14 or 21 days separately at 37 ± 0.5ºC. On completion, 0.5N HCl was added to the cells, cell lysates were centrifuged (3 minutes, 15,000 rpm, 4 ºC), and the supernatant was used for the measurement of calcium deposition using QuantiChromTM Calcium Assay Kit (DICA-500, BioAssay Systems, Hayward, CA). The protocol provided by the manufacturer was followed. An optical density was determined at a wavelength of 612 nm.
RESULTS AND DISCUSSION
Pseudo-ternary phase diagrams and preparation of microemulsion
It is easier to get an idea of a concentration range of different components required for a monophasic microemulsion through ternary phase studies. Figure 1 shows the results of phase studies performed with IPM, AOT, and labrasol. Oil, water, and surfactant mixture were denoted as oil, water, and Smix in the phase diagram, respectively. Each diagram describes the isotropic microemulsion region for individual ternary mixture denoted by the shaded region. The sizeable monophasic region was obtained in each plot, and it was majorly confined to the oil Smix axis, which indicates formation w/o microemulsion. An ample amount of water was solubilized with the help of the chosen surfactant mixture without resulting in phase separation. Mitra and Paul have previously reported an improvement in water solubilization ability in w/o microemulsion with a mixture of surfactants comprising of AOT and non-ionic surfactants (Mitra and Paul, 2005). The addition of non-ionic surfactant labrasol to AOT played a major role in increasing solubilization of a high amount of water and hence resulted in a wide microemulsion region. We observed that with an increase in the ratio of AOT:labrasol up to a certain extent (from 1:1 to 4:1), the monophasic microemulsion region grows in the area, beyond which microemulsion domain (at 5:1) reduced a little. This behavior is explained by few studies which clarify that the expansion of the microemulsion region depends on the certain mole fraction of a non-ionic surfactant and can increase or decrease beyond it (Kantaria et al., 2003; Mitra and Paul, 2005). On the other hand, Kantaria found no clear indication between this particular pattern with hydrophilic-lipopholic balance (HLB) of surfactants and recommended to perform ternary studies with multiple ratios of surfactant mixture, similar to we did here, to get an exact idea, which surfactant ratio would be the best to use for the formation of w/o microemulsion.
The inspection of phase diagrams concludes that, at AOT/labrasol ratio of 4:1, the maximum water solubilization was possible. A higher percentage of water in stable microemulsion can prove beneficial in incorporating water-soluble drugs such as ALD. The final formulation was prepared by keeping the surfactant weight ratio at 4:1. The composition of ALD microemulsion is shown in Table 1. The final drug concentration in microemulsion was around 0.2%w/w.
 | Table 1. Percentage composition of blank microemulsion [Click here to view] |
 | Figure 1. Ternary phase diagrams for water–AOT/labrasol–IPM combination with varying ratios of AOT:labrasol (a) 1:1, (b) 2:1, (c) 3:1, (d) 4:1, (e) 5:1. [Click here to view] |
Physical appearance
Microemulsions appeared as clear and transparent homogenous liquid with no turbidity or phase separation. There was no visible drug precipitation in ALD microemulsion. These results impart that the prepared microemulsion was a stable monophasic liquid.
Globule size
Globule size analysis exhibited a mean globule size of microemulsion in nanosize range with a mean diameter of 93.21 ± 5.95 nm. The polydispersity index was observed to be on a lower side (<0.3) which indicates uniform globule sizes within the formulation.
Transmission electron microscopy
TEM result for the ALD microemulsion is shown in Figure 2. It displayed spherical-shaped droplets of microemulsion with the size range around 100 nm similar to indicated by globule size studies.
Drug content
The drug content of the microemulsion was found to be 89.56 ± 4.2%w/w.
Refractive Index (RI)
The refractive index of drug-loaded microemulsion stayed unchanged as that of blank microemulsion (Table 2). The refractive indices of o/w microemulsion are usually slightly lower than w/o microemulsion due to the lower refractive index of aqueous external phase (RI = 1.33) than most of the pharmaceutically used oils (Junyaprasert, 2008). The refractive indices of prepared formulations in this study are notably similar to the refractive index of IPM (RI = 1.44), which is an external phase and addition of water (as internal phase), and surfactants did not show a major influence on RI.
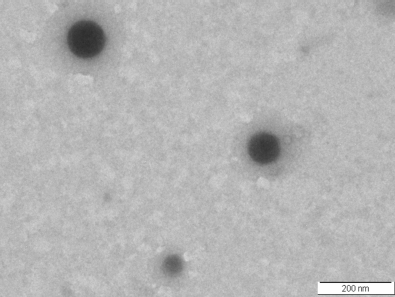 | Figure 2. TEM image of alendronate microemulsion. [Click here to view] |
 | Table 2. Characterization of blank microemulsion as compared to alendronate microemulsion. [Click here to view] |
Viscosity
The blank and ALD-loaded microemulsion displayed low viscosity (Table 2) which is the characteristic of microemulsion (Junyaprasert, 2008).
Density
The density of blank and ALD microemulsion remains unchanged as a small amount of the drug did not have any significant effect (p > 0.05) on the density of microemulsion (Table 2).
Electrical conductivity
Low electrical conductivity is a typical property of w/o microemulsion due to the presence of a non-aqueous outer phase. As electrical conductive component in a microemulsion is water, it is present as the inner phase, and the low electrical conductivity is observed when w/o microemulsions are concerned (Cao et al., 2019; Kantaria et al., 2003). The conductivity of both, blank and drug-containing w/o microemulsion, was found to be quite low (Table 2).
Differential scanning colorimetry
The samples of pure IPM, blank, and ALD-loaded microemulsion were compared for a cooling–heating cycle with the help of DSC. Some important characteristics of thermogram related to the melting or freezing of oil/water points were observed. In o/w microemulsion, water is present as the continuous phase, weakly bound to surfactant, termed as free water, and freezes at the temperatures close to 0°C, whereas the water existing as the dispersed phase in w/o microemulsion is strongly bound to the surfactant at the interface and is termed as bound water. Such water freezes at the temperature below 0°C. Hence, studying the thermal pattern of bound water as the dispersed system is a simple, easy, and supplemental tool to learn about the microstructures of microemulsions (Liu et al., 2009). In Figure 3, endothermic peak appearing above zero temperature (5.4°C) represented the melting of the oil, and this peak is prominent in all three DSC curves. A very weak endothermic peak below zero temperature (−5.5°C) was attributed to the melting of bound water in the dispersed phase. This weak endothermic peak was absent from the thermogram of pure IPM. The DSC curves of blank microemulsion and their drug-loaded counterpart were generally similar; however, slight shifts in the thermal events were observed. This may be because the drug has a certain effect on a surfactant film or the interaction between surfactant and water molecules (Boonme, 2007; Podlogar, 2004). The results of DSC studies are in agreement with observations from conductivity and RI and confirm the type of prepared microemulsion as w/o.
Thermodynamic stability studies
The prepared microemulsion could survive a thermodynamic stability test without any drug precipitation and phase separation. Low interfacial tension due to surfactant blend and smaller globule size could be vital reasons for the stability of microemulsion against extreme conditions (Russell-Jones and Himes, 2011; Yanyu et al., 2012).
Stability study
As stability study is a crucial parameter for the evaluation of microemulsion, it was performed effectively for 3 months, and the satisfactory results were obtained with globule size and drug content (Table 3). No drug precipitation or visual aggregation was reported as well. Hence, it is suggested that the prepared w/o microemulsion is stable at least for 3 months.
In vitro permeation
Alendronate microemulsion in varying doses of 0.1, 0.5, and 1 mg was applied to rat skin, and the permeation behavior of these test samples was compared with an aqueous solution (dose: 1 mg) of ALD. The lowest amount of ALD, i.e., only 17 ± 5.45 μg/cm2 was permeated through rat skin with ALD microemulsion having a dose of 0.1 mg (Fig. 4a), in 24 hours. Similarly, with a medium dose of ALD microemulsion (dose 0.5 mg), a significantly lower amount of drug was permeated (121± 9.01 μg/cm2) when compared to microemulsion with a 1 mg dose of ALD (350 ± 42.69 μg/cm2, p < 0.05), in 24 hours. Earlier research work, performed by Russell Jones and Himes, has stated that concentration gradient acts as a key factor in the absorption of hydrophilic drugs across the skin, and passive diffusion is the principal mechanism in the process (Russell-Jones and Himes, 2011). Hence, a higher drug permeation through w/o microemulsion was observed with a larger dose of ALD. In the case of ALD solution (dose 1 mg), a significantly low amount of ALD got permeated at the end of 24 hours (102 ± 35.4 μg/cm2, p < 0.05) when compared to ALD microemulsion (dose 1 mg). Alendronate microemulsion with medium dose (0.5 mg) achieved q little higher permeation than ALD solution but lacked significance (p > 0.05). These better permeation profiles of ALD through w/o microemulsion can be attributed to the different components of microemulsion which can act as permeation enhancers. The inclusion of IPM in the microemulsion can considerably boost the permeation of drugs across the skin than many other commonly used pharmaceutically accepted oils (Zhang et al., 2011) by modulating the lipid barrier of the skin (Suh and Jun, 1996). Besides, several studies advocate the use of AOT in w/o microemulsion to augment the permeation of drugs through the rat skin (Gupta et al., 2005). The lipophilic portion of the AOT works together with keratinous proteins of the skin causing the softening of the stratum corneum which eases the permeation process (Changez and Varshney, 2000). Non-ionic surfactants too, labrasol in this study, contribute to permeation enhancement, by increasing the fluidity of stratum corneum (Nokhodchi et al., 2003). Moreover, the nanosize of the microemulsion droplets increases the chances of their adherence to the skin which eventually can result in better permeation (Yanyu et al., 2012; Kogan and Garti, 2006). This confirms that the submicron globule size of microemulsion along with the use of optimal excipients, which acted as permeation enhancers, improved the permeation of ALD along rat skin than a solution of ALD. We hypothesized that, noteworthy, improvement in skin permeation with w/o microemulsion would favorably increase the bioavailability of ALD when applied transdermally.
 | Table 3. Stability studies of ALD microemulsion: analysis of globule size and drug content for period of three months. [Click here to view] |
 | Figure 3. DSC thermograph of IPM (a) compared with blank microemulsion (b) and alendronate microemulsion (c). [Click here to view] |
In vivo pharmacokinetic study
A pharmacokinetic study was performed to support in vitro data and to investigate if dose reduction of ALD could be possible with improvement in bioavailability on transdermal delivery of w/o microemulsion. Plasma concentration–time profiles and post-administration of ALD in rats via various administration routes are shown in Figure 4b, and the standard pharmacokinetic parameters are shown in Table 4. The pharmacokinetic profiles of transdermal ALD microemulsion at three different doses (at a dose of 20, 25, and 30 mg/kg) were compared with intravenous (dose 1 mg/kg) and oral (dose 30 mg/kg) administration of ALD. On the transdermal application of microemulsion, the plasma concentrations of ALD gradually increased for the first 3 hours and were at an almost constant level up to 12 hours. This might be due to the continuous and controlled delivery of ALD from the w/o microemulsion (Zhao et al., 2006). This observation was unchanged for all transdermal microemulsion groups with different doses of ALD. An intravenous administration of ALD demonstrated a quick and steep rise in plasma concentration and subsequent disappearance from the bloodstream. The oral administration of ALD solution (30 mg/kg) followed a similar pattern as that of intravenous administration with quickly attending Cmax (285 ± 89.41 ng/ml at Tmax 1 hour) than transdermal microemulsion (Tmax 3 hours) and fading afterward from the bloodstream. This difference in the Tmax could be due to the delay in the permeation of ALD due to multiple layers of the skin (Gannu et al., 2010). It was noted that the AUC(0–24) of ALD increased with ascending order of the dose of ALD microemulsion (20 < 25 < 30 mg/kg). Dosing ALD microemulsion (30 mg/kg) via transdermal route led to around 2-fold higher AUC(0–24) than ALD oral solution (30 mg/kg, p < 0.05). Furthermore, ALD transdermal microemulsion at dose of 25 mg/kg resulted in higher AUC(0–24) even with a lower dose than that of the ALD oral solution (30 mg/kg) but failed to report any significance (p > 0.05). A higher bioavailability was achieved with ALD w/o microemulsion (dose 20/g/kg; 2.3%, and 30 mg/kg; 3.58%) when compared with ALD oral solution (dose 30 mg/kg; 1.85%).
 | Figure 4. (a). In vitro drug permeation-time profile of alendronate solution-ALD sol 1 mg (-♦-); alendronate microemulsion-ALD ME 1 mg (-â– -); alendronate microemulsion-ALD ME 0.5 mg (-â–²-); alendronate microemulsion-ALD ME 0.1 mg (-×-) using rat skin by Franz diffusion cells (mean ± S.D, n = 3). (b) Plasma concentration vs. time profile for alendronate solution intravenous-ALD IV 1 mg/kg (-♦-); alendronate solution oral-ALD oral 30 mg/kg (-â– -); alendronate microemulsion transdermal-ALDME TD 20 mg/kg (-â–²-); alendronate microemulsion-ALDME TD 25 mg/kg (-×-); alendronate microemulsion-ALDME TD 30 mg/kg (---). (mean ± S.D, n = 3). [Click here to view] |
Based on the results of the pharmacokinetic study, the w/o microemulsion proved to be an effective carrier system to deliver ALD across the skin. Oil from a continuous phase of w/o microemulsion is compatible with sebum from hair follicles. It is reported that, for hydrophilic drugs such as ALD, hair follicular route is the main path for permeation through the skin (Teichmann et al., 2006). The globule size of the microemulsion carrier is generally smaller than the size of the opening of a hair follicle and, hence, can help the penetration of drugs. The hair follicle provides a larger surface area with compromised stratum corneum (Abd et al., 2018; Blume-Peytavi and Vogt, 2011), and a thick network of blood capillaries around the follicle enhances the systemic absorption of the drug (Lademann et al., 2009). Furthermore, using permeation enhancers in the microemulsion, in the form of oil and surfactants, can contribute to the increased permeation of drugs on transdermal application (Gannu et al., 2010; Setya et al., 2017). These individual microemulsion components, when taken together as a chemical mixture, can act synergistically for the enhancement of transdermal drug delivery (Karande and Mitragotri, 2009). Based on pharmacokinetic profiles of ALD given by different routes, we observed that reduction in the dose of ALD transdermal microemulsion (dose 25 mg/kg) gave an insignificantly different plasma profile than ALD oral solution (dose 30 mg/kg, p > 0.05). On the other hand, ALD transdermal microemulsion with the same dose (30 mg/kg) as that of the oral solution (dose 30 mg/kg, p > 0.05) resulted in a significant increase in exposure (AUC(0–24) ) and the bioavailability (p< 0.01). Comparing the results of a pharmacokinetic study with that of skin permeation studies, a similar trend is observed and confirmed the selection of particular microemulsion excipients assisted in improving the permeation of ALD with microemulsion. This research work states that the use of a lipid carrier for improving the transepidermal permeation can be a sound method for the proficient delivery of hydrophilic drugs such as ALD across the skin and can probably be used to avoid toxicity related to its oral administration.
 | Table 4. Pharmacokinetic parameters upon single-dose administration of ALD. [Click here to view] |
 | Figure 5. Proliferation of osteoblast-like cells (MG-63 cells) treated with blank microemulsion (ME), pure drug alendronate (ALD), and alendronate microemulsion (ALD ME) for 48 and 72 hours, expressed as a percentage of optical density relative to control (medium only) of 100%, using MTT assay (mean ± S.D, n = 3, *p < 0.05 compared with the control group). [Click here to view] |
MTT assay
Cultured cell lines are generally utilized to scrutinize the vital aspects of drug metabolism linked to toxicity. We used MG-63 cells in this study as they are immature osteoblastic cells, which enables studying the effect of ALD on the initial developmental stages of cells (Xiong et al., 2009). MTT assay as a cell viability study was conducted to estimate the effect of ALD and ALD microemulsion on MG-63 osteoblast-like cells (Fig. 5). We represented the data relative to the optical density of the control group as 100%. Treatment with ALD was successful in promoting cell proliferation, indicating that the test samples were not cytotoxic. In ALD-treated groups (ALD solution and microemulsion), cell number was greater at 48 hours and significantly higher at 72 hours of treatment (p < 0.05) than in the untreated groups (control and blank microemulsion). The increase in cell number was the greatest for ALD microemulsion after 72 hours (13% increase above control cells). When compared with ALD solution, the viability of cells cultured with ALD microemulsion was higher but lacked significance (p > 0.05). Similar effects of ALD formulations against osteoblastic cells are reported in earlier works highlighting its osteogenic ability (Ezzati et al., 2014; Im et al., 2004; Kim et al., 2012). Im et al. described the proliferative and maturation inducing effects of ALD and risedronate on MG-63 osteoblast-like cells (Im et al., 2004). Ezzati et al. reported that the nanoformulation of ALD was not only cytocompatible but also increased viability of cultured cells than ALD pure drug (Ezzati et al., 2014). Kim et al. exhibited similar activity of ALD with no cytotoxicity (Kim et al., 2012). Although the primary mechanism involved in bisphosphonate-induced cell proliferation is unknown, few researchers considered that extracellular signal-regulated kinases can play a key role in the same (Mathov et al., 2001). Few studies observed inhibitory or no effects of bisphosphonates on the viability of human osteoblastic cells (Garcia-Moreno et al., 1998; Reinholz et al., 2000). The explanations for these contradictory observations might be related to the bisphosphonate analog and its concentration range used in the study. The overall time of treatment and type of cells could also be responsible for the differing effects.
 | Figure 6. (a). ALP activity of osteoblast-like cells (MG-63 cells) treated with medium only (control) blank microemulsion (ME), pure drug alendronate (ALD), and alendronate microemulsion (ALDME) after 3, 7, and 10 days of incubation (mean ± S.D, n = 3, * p < 0.05 compared with control and ME group, ap < 0.01 compared with control and ME group). (b) Calcium deposition of osteoblast-like cells (MG-63 cells) treated with medium only (control) blank microemulsion (ME), pure drug alendronate (ALD), and alendronate microemulsion (ALDME) after 14 and 21 days of incubation (mean ± S.D, n = 3, * p < 0.05 compared with control and ME group, ap < 0.01 compared with control and ME group). [Click here to view] |
From the results of the MTT assay, we speculated that, along with proliferation, ALD microemulsion can induce maturation and osteogenic activity in MG 63 osteoblastic cells.
ALP activity and mineralization
ALP is a definite index for the estimation of osteogenic activity and tissue differentiation. We evaluated the influence of ALD on the initial differentiation of osteoblasts through ALP activity at 3, 7, and 10 days (Fig. 6a). We noted an increase in the ALP activities of MG-63 cells of all substrates for 10 days of the incubation period. At 3 days of incubation, the ALP levels of cells cultured without the drug (i.e., control or blank microemulsion) did not differ significantly from cells cultured with ALD microemulsion/solution (Fig. 6a, p > 0.05). On the contrary, MG-63 cells cultivated with ALD microemulsion or solution showed a significant increase in ALP activity at day 7 (p < 0.05) and day 10 (p < 0.01) of incubation than that of untreated cells. The maximum levels of ALP were noted with the cells cultured with ALD microemulsion at 10 days of incubation (Fig. 6a). In an earlier study by Kim et al., the ALP levels of osteoblast-like cells treated with ALD were found to be significantly higher in comparison to the control group (Kim et al., 2012). Xiong et al. positively correlated the osteogenic activity of ALD with ALP activities of osteoblastic cells. They have shown that ALD upregulated ALP levels in cells along with the increased expressions of genes of bone turnover markers such as osteocalcin, bone morphogenetic protein and collagen (Xiong et al., 2009). Wang et al. observed that ALD is capable of increasing ALP activity in osteoblastic cells other than MG-63 (Wang et al., 2010). Here, we have shown that ALD enhances differentiation and bone formation by increasing ALP activity in osteoblastic cells, which is also supported by the previous research works (Kim et al., 2010; Moon et al., 2011; Shi et al., 2009).
A late differentiation of osteoblasts was studied by determining the calcium deposition by MG-63 cells on culturing with ALD solution and microemulsion for 14 and 21 days (Fig. 6b). Alendronate significantly raised calcium deposition in both substrates (ALD solution and microemulsion) after treatment for 14 and 21 days when compared with cells cultured without the drug (control and blank microemulsion, p < 0.05). Results confirmed that ALD microemulsion encourages the maximum deposition of a mineral matrix in cultured osteoblast-like cells (Fig. 6b). BPs are known to promote the mineralization of cell culture through various cellular pathways including inhibition of mevalonate, protein tyrosine phosphatase pathway, or acceleration of non-RAS-MEK-ERK ½ cbfa 1 pathway (Fujita et al., 2001; Itoh et al., 2003; Reinholz et al., 2002). These results are in agreement with those of Xiong et al. study which indicates that ALD augments the development of MG-63 cells to the mineralization stage (Xiong et al., 2009).
Results from mineralization study support the outcomes of MTT and ALP studies. Taken together, these findings recommend that ALD microemulsion can promote cellular functions of osteoblast-like cells and can prompt their differentiation and maturation. The results in this study support the theory that ALD has anabolic and osteogenic effects on osteoblasts.
CONCLUSION
The present study successfully confirmed that the transdermal w/o microemulsion system can present a real interest in the systemic delivery of a hydrophilic drug, such as ALD. The transdermal application of microemulsion provided a better pharmacokinetic profile than oral ALD which may prove beneficial in anti-osteoporotic treatment. The results indicate that the encapsulation of ALD, a bisphosphonate, in a microemulsion can retain its osteogenic and anabolic effects. Hence, it is anticipated that the use of microemulsion as a transepidermal carrier system can possibly improve the therapeutic efficacy of a bisphosphonate and can increase a patient compliance by evading severe gastrointestinal adverse effects.
ACKNOWLEDGMENTS
The authors are thankful to the University Grant Commission—Basic Science Research (UGC-BSR) for grants.
CONFLICT OF INTEREST
The authors declare that they have no conflict of interest.
STATEMENT OF HUMAN AND ANIMAL RIGHTS
The protocols for animal experiments (25/1617) were approved by the Animal Experimentation Committee of the National Toxicology Centre, Pune.
REFERENCES
Abd E, Benson HAE, Roberts MS, Grice JE. Minoxidil skin delivery from nanoemulsion formulations containing eucalyptol or oleic acid: enhanced diffusivity and follicular targeting. Pharmaceutics, 2018; 10(1):19; doi: 10.3390/pharmaceutics10010019 CrossRef
Alkrad JA, Al-doori SM, AlGhatm H. Using inverted microemulsions for transdermal application of folic acid. Asian J Pharm Sci, 2019; 13(2):134–40.
Anjum S, Gupta A, Sharma D, Dalal P, Gupta B. Skin compatibility and antimicrobial studies on biofunctionalized polypropylene fabric. Mater Sci Eng C, 2016; 69:1043–50. CrossRef
Benson HAE. Transdermal drug selivery: penetration enhancement techniques. Cur Drug Deliv, 2005; 2:23–33. CrossRef
Blume-Peytavi U, Vogt A. Human hair follicle: reservoir function and selective targeting. Br J Dermatol, 2011; 165:13–7. CrossRef
Boonme P. Applications of microemulsions in cosmetics. J Cosmet Dermat, 2007; 6:223–8. CrossRef
Cao Y, Gao H, Xia H, Zhu X, Li B, Zhou X, Jin Y. Development and evaluation of a water-in-oil microemulsion formulation for the transdermal drug delivery of teriflunomide (A771726). Chem Pharm Bull, 2019; 67:786–94. CrossRef
Changez M, Varshney M. Aerosol-OT microemulsions as transdermal carriers of tetracaine hydrochloride. Drug Dev Ind Pharm, 2000; 26(5):507–12. CrossRef
Choi A, Gang H, Chun I, Gwak H. The effects of fatty acids in propylene glycol on the percutaneous absorption of alendronate across the excised hairless mouse skin. Int J Pharm, 2008; 357:126–31. CrossRef
Dib N, Falcone RD, Acuna A, Garcia-Rio L. The ionic liquid-surfactant bmim-AOT and nontoxic lipophilic solvents as components of reverse micelles alternative to the traditional systems. A study by 1H NMR spectroscopy. J Mol Liq, 2020; 304: 112762; doi:10.1016/j.molliq.2020.112762 CrossRef
Drake MT, Clarke BL, Khosla S. Bisphosphonates: mechanism of action and role in clinical practice. Mayo Clin Proc, 2008; 83(9):1032–45. CrossRef
Ezra A, Golomb G. Administration routes and delivery systems of bisphosphonates for the treatment of bone resorption. Adv Drug Deliv Rev, 2000; 42:175–95. CrossRef
Ezzati J, Dolatabadi N, Hamishehkar H, Eskandani M, Valizadeh H. Formulation, characterization and cytotoxicity studies of alendronate sodium-loaded solid lipid nanoparticles. Colloids Surf B: Biointerfaces, 2014; 117:21–8. CrossRef
Fujita T, Izumo N, Fukuyama R, Meguro T, Yasutomi C, Nakamuta H, Koida M. Incadronate and etidronate accelerate phosphate-primed mineralization of MC4 cells via ERK1/2-Cbfa1 signaling pathway in a rasindependent manner: further involvement of mevalonate-pathway blockade for incadronate. Jpn J Pharmacol, 2001; 86:86–96. CrossRef
Furuishi T, Kunimasu K, Fukushima K, Ogino T, Okamato K, Yonemochi E, Tomono K, Suzuki T. Formulation design and evaluation of a transdermal drug delivery system containing a novel eptazocine salt with the Eudragit® E adhesive. J Drug Deliv Sci Technol, 2019: 54:101289; doi:10.1016/j.jddst.2019.101289 CrossRef
Gannu R, Palem CR, Yamsani VV, Yamsani SK, Yamsani MR. Enhanced bioavailability of lacidipine via microemulsion based transdermal gels: formulation optimization, ex vivo and in vivo characterization. Int J Pharm, 2010; 388:231–41. CrossRef
Garcia-Moreno C, Serrano S, Nacher M, Farré M, Díez A, Mariñoso ML, Carbonell J, Mellibovsky L, Nogués X, Ballester J, Aubía J. Effect of alendronate on cultured normal human osteoblasts. Bone, 1998; 22:233–9. CrossRef
Graham DY. What the gastroenterologist should know about the gastrointestinal safety profiles of bisphosphonates. Dig Dis Sci, 2002; 47:1665–78. CrossRef
Gupta RR, Jain SK, Varshney M. AOT w/o microemulsions as penetration enhancer in transdermal drug delivery of 5-fluorouracil. Colloids Surf B: Biointerfaces, 2005; 41:25–32. CrossRef
Ha H, Ho J, Shin S, Kim H, Koo S, Kim IH, Kim C. Effects of eucommiae cortex on osteoblast-like cell proliferation and osteoclast inhibition. Arch Pharm Res, 2003; 26(11):929–36. CrossRef
Hamed R, Farhan A, Abu-Hawaij R, Mahamoud NN, Kamal A. Lidocaine microemulsion-laden organogels as lipid-based systems for topical delivery. J Pharm Innov, 2019; doi:10.1007/s12247-019-09399-zc CrossRef
Hashem FM, Shaker DS, Ghorab MK, Nasr M, Ismail A. Formulation, characterization and clinical evaluation of microemulsion containing clotrimazole for topical delivery. AAPS PharmSciTech, 2011; 12:879–86. CrossRef
Im GI, Qureshi SA, Kenney J, Rubash HE, Shanbhag AS. Osteoblast proliferation andmaturation by bisphosphonates. Biomaterials, 2004; 25:4105–15. CrossRef
Itoh F, Aoyagi S, Furihata-Komatsu H, Aoki M, Kusama H, Kojima M, Kogo H. Clodronate stimulates osteoblast differentiation in ST2 and MC3T3-E1 cells and rat organ cultures. Eur J Pharmacol, 2003; 477:9–16. CrossRef
Junyaprasert VB, Boonme P, Wurster DE, Rades T. Aerosol ot microemulsions as carriers for transdermal delivery of hydrophobic and hydrophilic local anesthetics. Drug Deliv, 2008; 15:323–30. CrossRef
Kantaria S, Rees GD, Lawrence MJ. Formulation of electrically conducting microemulsion-based Organogels. Int J Pharm, 2003; 250:65–83. CrossRef
Karande P, Mitragotri S. Enhancement of transdermal drug delivery via synergistic action of chemicals. Biochimica et Biophysica Acta, 2009; 1788(11): 2362–73. CrossRef
Katsuni H, Liu S, Tanaka Y, Hitomi K, Hayashi R, Hirai Y, Kusamori K, Quan YS, Kamiyama F, Sakane T, Yamamoto A. Development of a novel self-dissolving microneedle array of alendronate, a nitrogen-containing bisphosphonate: evaluation of transdermal absorption, safety, and pharmacological effects after application in rats. J Pharm Sci, 2012; 1:3230–8. CrossRef
Kaur A, Sharma G, Gupta V, Ratho RK, Katare OP. Enhanced acyclovir delivery using w/o type microemulsion: preclinical assessment of antiviral activity using a murine model of zosteriform cutaneous HSV-1 infection. Artif Cells Nanomed Biotechnol, 2018; 46:346–54. CrossRef
Kim CW, Yun YP, Lee HJ, Hwang YS, Kwon IK, Lee SC. In situ fabrication of alendronate-loaded calcium phosphate microspheres: controlled release for inhibition of osteoclastogenesis. J Control Rel, 2010; 147(1):45–53. CrossRef
Kim SE, Suh DH, Yun YP, Lee JY, Park K, Chung JY, Lee DW. Local delivery of alendronate eluting chitosan scaffold can effectively increase osteoblast functions and inhibit osteoclast differentiation. J Mater Sci Mater Med, 2012; 23:2739–49. CrossRef
Kogan A, Garti N. Microemulsions as transdermal drug delivery vehicles. Adv Colloid Interface Sci, 2006; 123:369–85. CrossRef
Kumbhar MD, Karpe MS, Kadam VJ. Development and characterization of water-in-oil microemulsion for transdermal delivery of Eperisone hydrochloride. Appl Clin Res Clin Trials Regul Aff, 2020; 7(1):45–64. CrossRef
Lademann J, Patzelt A, Richter H, Schanzer S, Sterry W, Filbry A, Bohnsack K, Rippke F, Meinke M. Comparison of two in vitro models for the analysis of follicular penetration and its prevention by barrier emulsions. Eur J Pharm Biopharm, 2009; 72:600–4. CrossRef
Lambrinoudaki I, Christodoulakos G, Botsis D. Bisphosphonates. Ann N Y Acad Sci, 2006; 1092:397–402. CrossRef
Liebig F, Moreno S, Thunemann AF, Temme A, Appelhans D, Koetz J. Toxicological investigations of “naked” and polymer-entrapped AOT-based gold nanotriangles. Colloids Surf B Biointerfaces, 2018; 167:560–7. CrossRef
Liu H, Wang Y, Lang Y, Yao H, Dong Y, Li S. Bicontinuous cyclosporine-A loaded water-Aot/tween 85-isopropylmyristate microemulsion: structural characterization and dermal pharmacokinetics in vivo. J Pharm Sci, 2009; 98(3):1167–76. CrossRef
Marwah H, Garg T, Goyal AK, Rath G, Permeation enhancer strategies in transdermal drug delivery. Drug Deliv, 2014; 23(2):564–78. CrossRef
Mathov I, Plotkin LI, Sgarlata CL, Leoni J, Bellido T. Extracellular signal-regulated kinases and calcium channels are involved in the proliferative effect of bisphosphonates on osteoblastic cells in vitro. J Bone Miner Res, 2001; 16:2050–6. CrossRef
Meng J, Meng Q, Zheng L. A simple and rapid high-performance liquid chromatography method for determination of alendronate sodium in beagle dog plasma with application to preclinical pharmacokinetic study. Biomed Chromatogr, 2010; 24:169–73. CrossRef
Mitra RK, Paul BK. Effect of NaCl and temperature on the water solubilization behavior of AOT/nonionic mixed reverse micellar systems stabilized in IPM oil. Colloid Surf A: Physicochem Eng Aspects, 2005; 255:165–80. CrossRef
Moon HJ, Yun YP, Han CW, Kim MS, Kim SE, Bae MS, Kim GT, Choi YS, Hwang EH, Lee JW, Lee JM, Lee CH, Kim DS, Kwon IK. Effect of heparin and alendronate coating on titanium surfaces on inhibition of osteoclast and enhancement of osteoblast function. Biochem Biophys Res Commun, 2011; 413(2):194–200. CrossRef
Naniwa T, Maeda T, Mizoshita T, Hayami Y, Watanabe M, Banno S, Ito R. Alendronate induced esophagitis: possible pathogenic role of hypersensitivity to alendronate. Intern Med, 2008; 47:2083–5. CrossRef
Nastiti C, Ponto T, Abd E, Grice JE, Benson HAE, Roberts MS. Topical nano and microemulsions for skin delivery. Pharmaceutics, 2017; 9:37–62. CrossRef
Nokhodchi A, Shokri J, Dashbolaghi A, Hassan-Zadeh D, Ghafourian T, Barzegar-Jalali M. The enhancement effect of surfactants on the penetration of lorazepam through rat skin. Int J Pharm, 2003; 250:359–69. CrossRef
Pakpayat N, Nielloud F, Fortune R, Tourne-Peteilh C, Villarreal A, Grillo I, Bataille B. Formulation of ascorbic acid microemulsions with alkyl polyglycosides. Eur J Pharm Biopharm, 2009; 72: 444–52. CrossRef
Podlogar F, Gasperlin M, Tomsic M, Jamnik, A, Rogac, M.B. Structural characterization of water-tween 40/imwitor 308-isopropyl myristate microemulsions using different experimental methods. Int J Pharm, 2004; 276:115–28. CrossRef
Porras AG, Holland SD, Gertz BJ. Pharmacokinetics of alendronate. Clin Pharmacokinet, 1999; 36:315–28. CrossRef
Reinholz GG, Getz B, Pederson L, Sanders ES, Subramaniam M, Ingle JN, Spelsberg TC. Bisphosphonates directly regulate cell proliferation, differentiation, and gene expression in human osteoblasts. Cancer Res, 2000; 60:6001–7.
Reinholz GG, Getz B, Sanders ES, Karpeisky MY, Padyukova NS, Mikhailov SN, Ingle JN, Spelsberg TC. Distinct mechanisms of bisphosphonate action between osteoblasts and breast cancer cells: identity of a potent new bisphosphonate analogue. Breast Cancer Res Treat, 2002; 71:257–68. CrossRef
Russell-Jones G, Himes R . Water-in-oil microemulsions for effective transdermal delivery of proteins. Expert Opin Drug Deliv, 2011; 8:537-546. CrossRef
Sapra B, Thatai P, Bhandari S, Sood J, Jindal M, Tiwary AK. A critical appraisal of microemulsions for drug delivery: part II. Ther Deliv, 2014; 5:83–94. CrossRef
Schenk R, Eggli P, Fleisch H, Rosini S. Quantitative morphometric evaluation of the inhibitory activity of new aminobisphosphonates on bone resorption in the rat. Calcif Tissue Int, 1986; 38:342–9. CrossRef
Setya S, Madaan T, Tariq M, Razdan BK, Talegaonkar S. Appraisal of transdermal water-in-oil nanoemulgel of selegiline HCl for the effective management of Parkinson’s disease: pharmacodynamic, pharmacokinetic and biochemical investigations. AAPS PharmSciTech, 2017; 19(2):573–89. CrossRef
Shi X, Wang Y, Ren L, Gong Y, Wang DA, Enhancing alendronate release from a novel PLGA/hydroxyapatite microspheric system for bone repairing applications. Pharm Res, 2009; 26(2):422–30. CrossRef
Sintov AC, Botner S. Transdermal drug delivery using microemulsion and aqueous systems: influence of skin storage conditions on the in vitro permeability of diclofenac from aqueous vehicle systems. Int J Pharm, 2006; 311:55–62. CrossRef
Suh H, Jun HW. Effectiveness and mode of action of isopropyl myristate as a permeation enhancer for naproxen through shed snake skin. J Pharm Pharmacol, 1996; 48(8):812–6. CrossRef
Talhouni AA, Alkrad JA, Al-Dabbagh MM, Abazid H, Hussein-Al-Ali SH. Transdermal of atenolol via microemulsions. Int J App Pharm, 2019; 11(2):164–71. CrossRef
Teichmann A, Otberg N, Jacobi U, Sterry W, Lademann J. Follicular penetration: development of a method to block the follicles selectively against the penetration of topically applied substances. Skin Pharmacol Physiol, 2006; 19:216–23. CrossRef
Van Beek ER, Cohen LH, Leroy IM, Ebetino FH, Löwik CW, Papapoulos SE. Differentiating the mechanisms of antiresorptive action of nitrogen-containing bisphosphonates. Bone, 2003; 33:805–11. CrossRef
Wang Y, Shi X, Ren L, Yao Y, Wang DA. In vitro osteogenesis of synovium mesenchymal cells induced by controlled release of alendronate and dexamethasone from a sintered microspherical scaffold. J Biomater Sci Polym Ed, 2010; 21(8–9):1227–38. CrossRef
Xiong Y, Yang HJ, Feng J, Shi ZL, Wu LD. Effects of alendronate on the proliferation and osteogenic differentiation of MG-63 cells. J Int Medical Res, 2009; 37:407–416. CrossRef
Yano T, Nakagawa A, Tsuji M, Noda K. Skin permeability of various nonsteroidal anti-inflammatory drugs in man. Life Sci, 1986; 39:1043–50. CrossRef
Yanyu X, Fang L, Qineng P, Hao C. The influence of the structure and the composition of water/AOT tween 85/IPM microemulsion system on transdermal delivery of 5-fluorouracil. Drug Dev Ind Pharm, 2012; 38:1521–9. CrossRef
Zhang J, Michniak-Kohn B. Investigation of microemulsion microstructures and their relationship to transdermal permeation of model drugs: ketoprofen, lidocaine, and caffeine. Int J Pharm, 2011; 421:34–44. CrossRef
Zhao H, Liu JP, Zhang X, Li Y. Enhancement of transdermal delivery of theophylline using microemulsion vehicle. Int J Pharm, 2006; 327:58–64. CrossRef
Zidan AS, Kamal N, Alayoubi A, Seggel M, Ibrahim S, Rahman Z, Cruz CN, Ashraf M. Effect of isopropyl myristate on transdermal permeation of testosterone from carbopol gel. J Pharm Sci, 2017; 106(7): 1805–3. CrossRef