INTRODUCTION
Community pharmacists are uniquely positioned to provide patient care because of their accessibility, expertise, and experience, which are contributory to the effective functioning of a healthcare system. In Vietnam, such medical professionals are directly consulted on health problems by over 80% of the population (Chalker et al., 2005). Correspondingly, community pharmacies are evolving into front-line service providers in the primary healthcare systems of the country. The evidence has shown that pharmacists can identify and resolve drug-related problems, empower patients to adopt positive self-management behaviors (Chandra et al., 2003), increase patient satisfaction (Liu et al., 1999), and optimize patient quality of care (Wu et al., 2006) through patient counseling.
To regulate pharmacy practice, therefore, the Vietnamese Drug Administration has issued good pharmacy practice principles and standards for community pharmacies since 2011 (Viet Nam’s Ministry of Health, 2010). The regulations clearly state that medication dispensing and counseling services should be implemented by registered pharmacists. However, few such modules focus on the development of community pharmacist-specific knowledge and skills in undergraduate programs in Vietnam (Vo et al., 2013). In the country, medicines are classified into over-the-counter (OTC) drugs and prescription-only medicines (POMs), but community pharmacies do not always recommend appropriate medications or strictly enforce prescription laws for POMs. These behaviors raise concerns regarding public health issues (Chalker et al., 2005) and highlight the necessity of implementing educational interventions revolving around the pharmaceutical management of common minor diseases. These initiatives are important as they may lead to global improvement in the quality of counseling by pharmacists.
Among typically occurring illnesses is the common cold, which is caused by viruses and cannot be treated through antibiotics. However, community pharmacists in Vietnam often dispense such medications for the condition without a physician’s prescription. As reported in a 2019 meta-analysis, 75.6% of antibiotics were dispensed by Vietnamese community pharmacists to patients who were primarily seeking relief from respiratory symptoms/illnesses with no prescriptions (Nguyen et al., 2019). This situation has triggered increasing apprehension as regards the resistance of common bacteria to frequently used antibiotics, thus driving Vietnam’s Ministry of Health to carry out national strategies for combatting bacterial resistance to medication.
With consideration of the above-mentioned issues, this study evaluated the effectiveness of short-term educational interventions on the knowledge and counseling practice of community pharmacists with respect to common cold management. To this end, pharmacists were administered a survey and involved in a pseudo customer assessment experiment.
MATERIALS AND METHODS
Study design and settings
This pre- and post-intervention study was carried out in Hue City, Thua Thien Hue Province in central Vietnam. The research was implemented in two parts: The first featured educational interventions and assessment via a paper-based test, and the second featured an experiment involving pseudo customer visits. Thirty-eight pharmacists accepted the invitation to participate in the educational interventions. The invitations were coursed through direct and online posters published on a website for pharmacists called nhipcauduoclamsang.com (literal translation: “bridge on clinical pharmacy”). The inclusion criteria were having a diploma in a pharmacy program, being a pharmacist employed in a pharmacy, and having provided informed consent to participate. The exclusion criteria were pharmacists working in hospitals or those employed by the same pharmacy chain.
Educational interventions
Training
Training content for the community pharmacists was developed and presented face to face by an experienced clinical pharmacist, who is also the author of The Pocket Handbook of Counseling for Community Pharmacists-30 Common Minor Symptoms, published officially in Vietnam in 2018 (Vo, 2018). The group-based training session, which was held at Hue University of Medicine and Pharmacy, encompassed five parts: (1) introduction and pre-test; (2) counseling and communication skills; (3) the common cold and its definition, causes and transmission pathways, and symptoms, as well as the differences between the cold and the flu, signs that denote the need for a medical visit, treatment in adults and children, and home care; (4) role play activities; and (5) session summary and post-test. In the role play, two lecturers acted out two scenarios (one involving a child with a common cold and another about an adult afflicted with the same condition) as a model, and then the participants were asked to contribute during the scenario debriefing on counseling skills and treatment ideas.
Educational materials
In addition to The Pocket Handbook, which covers counseling skills, a material on the management of 30 common symptoms and conditions encountered during pharmacy work was given to all the participants. Each section devoted to the management of a set of common symptoms and conditions (including the cold) is presented in the following standard format: (1) introduction, (2) symptoms, (3) differential diagnosis, (4) open-ended questions to be presented to patients for information collection, (5) cases for which a medical visit is needed, (6) treatment, and (7) advice.
Assessment
Paper-based test
A structured questionnaire was used to assess the knowledge of the participants on the management of the common cold before and after the educational interventions. The questionnaire consists of two sections: The first contains (1) general questions related to the demographics of a pharmacy and its staff, including the highest professional education attained, years of work experience, number of employees, and average number of customers entertained per day and (2) specific inquiries into knowledge on the management of the common cold, including its causes, transmission pathways, typical symptoms, and drug-related issues. The second section comprises 11 questions (nine multiple-choice questions and two short open-ended questions). The paper-based test was administered before and after the interventions.
Pseudo customer visits
Pseudo customer visits were conducted to assess the employees’ actual counseling practice a week after the educational interventions were implemented. Intensive training was provided to eight pseudo customers (two males and six females aged 21- to 22-year old and in their third and fourth years of pharmacy study). The training included role play activities, rehearsing the scenarios (Table 1), and practicing how to fill in an assessment checklist (Table 2).
In accordance with the pre-set scenarios, the pseudo customers entered the participating pharmacies and provided information to a pharmacist without showing a prescription. The community pharmacists were unaware that they were being assessed, and only those who attended the training sessions were evaluated. The pseudo customers were instructed to convey their requests at the beginning of the encounter in a standardized manner, providing no further information unless asked. If a participant asks an open-ended question, the pseudo customers were directed to provide all relevant information, but if closed-ended questions were raised, they were to provide only the information pertaining to the questions (most of the time, a “yes” or “no” response). The pseudo customers were instructed to actively ask for advice only if the pharmacist does not offer any additional information on drugs up to the point where payment for the medicine is made. They were then required to ask for directions on the use of the products (i.e., how to take the drugs and what to watch out for). They were also instructed to observe the behaviors of the pharmacy employees, memorize the advice given to them, and buy the medications recommended by the pharmacists. The conversations were recorded using a smartphone. Within 15 minutes after the visits, the pseudo customers were asked to fill an assessment checklist. At the end of the study, both a senior researcher and the pseudo customers listened to the recordings to verify the checklist as a means of ensuring the inter-rater reliability of the evaluations.
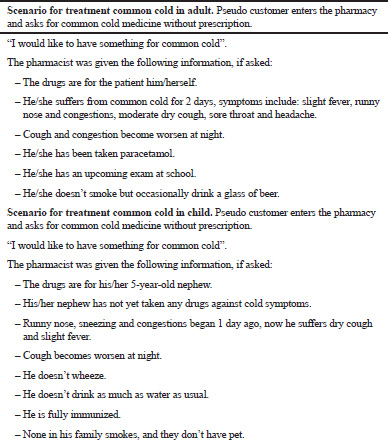 | Table 1. Case scenarios on common cold management. [Click here to view] |
 | Table 2. Checklist for counseling assessment. [Click here to view] |
Assessment checklist
The counseling guidelines of the American Society of Health-System Pharmacists (ASHP, 1997) was used as the primary reference in designing the assessment checklist, which was subsequently converted into an online format for convenient information filling and data collection. Figure 1 illustrates a flow chart that summarizes the study.
Statistical analyses
The data were encoded and analyzed using MedCalc® version 12.3, and chi-square and McNemar tests were employed to compare the proportion of right answers before and after the interventions (pre- and post-tests). A p < 0.05 was considered as statistically significant.
RESULTS AND DISCUSSION
Characteristics of the pharmacists
The intervention courses were attended by 38 community pharmacists, among whom the majority were female (32% or 84.2%), and 20 were younger than 30-year old and had less than 3 years of work experience. Most of them serve less than 50 clients per day (n = 23).
 | Figure 1. Study process. [Click here to view] |
 | Table 3. Proportion of correct answers before and after the interventions. [Click here to view] |
Assessment of knowledge about common cold management
The interventions significantly improved the knowledge of the pharmacists regarding common cold management. For the nine multiple-choice questions in the pre-test, only 37.4% of the participants provided correct answers, but this proportion increased to 83.9% in the post-test (p = 0.001) (Table 3). The most significant improvements were related to the provision of antihistamines as treatment for the common cold (71.0%) and the elaboration of all OTC pain relievers and fever reducers (63.1%).
The two short open-ended questions were intended to ask the participants to list which cases they believe require a visit to a clinic or hospital for additional medical care and which advice should be given when paracetamol is sold to customers. The average number of advice provided under these two situations significantly increased after the educational interventions from 1.89 ± 1.06 to 4.97 ± 2.64 (p = 0.017) and from 1.50 ± 0.89 to 2.08 ± 1.23 (p = 0.057), respectively. Similarly, Pham et al. (2013) found that educational training significantly increased Vietnamese pharmacists’ knowledge about the management of childhood diarrhea. Our study contributes evidence to support effectiveness of educational intervention on improvement of pharmacists’ knowledge.
Assessment of counseling skills
One week after the interventions, the pseudo customers visited 30 out of the 38 participating pharmacies to evaluate the counseling skills of the respondents (Table 4). The remaining eight pharmacies were excluded because they had irregular opening hours. Of the customers, 14 were asked to play out the adult scenario, and 16 were instructed to act out the child-based scenario. The customers were counseled by all the pharmacists, of whom 80% actively asked for further information and gave additional advice. By contrast, the remaining 20% offered information only when pressed by the pseudo customers. This rate of counsel provision is extensively high compared with the findings in our previous study, wherein counseling in community pharmacies in Hue was provided by only 61% of the pharmacists (Vo and Le, 2018). We believe that those pharmacists who participated in educational intervention got more knowledge and skills, then were more willing to provide counseling, which demonstrated by a high rate of counseling in pseudo customer visits. In a study in Germany, 98% of the participants offered advice, among which 36% was given on demand (Berger et al., 2005).
 | Table 4. Assessment of counseling skills. [Click here to view] |
Twenty sessions of counseling (66.7%) lasted for more than 3 minutes, and one-fifth of the session spanned over 5 minutes, which is higher than the result derived in the Korean context (i.e., only 6.8%) (Yang et al., 2016). The improved outcomes in the current work can be attributed to increased counseling awareness and skills among the trained pharmacists, the implementation of the treatment-request scenarios, and active interactions with the pseudo customers.
Community pharmacists should screen patients carefully by assessing the signs and symptoms of the illnesses presented. This would enable such personnel to supply safe and effective medicines for self-treatment (Brata et al., 2013). Our findings demonstrated that the pharmacists focused on acquiring basic information, namely, a patient’s identification (93.3%), age (80.0%), and symptoms (80.0%). They disregarded symptom duration as well as a patient’s medical history and allergies (no more than 20%). The literature on pharmacy performance in Vietnam indicated that pharmacists in the country ask a few and insufficient questions before they dispense medications. A study showed that 52% of pharmacists did not pose inquiries before providing advice and/or medications, but this percentage decreased to 34% after intervention (Pham et al., 2013). Researchers reviewed the information-gathering process for the provision of medicines for self-medication via community pharmacies in developing countries (Brata et al, 2013). They found that the reported rate of information gathering varied from 18% to 97%, depending on the research methods used. Information on signs and symptoms and patient identity is more frequently collected than medication history and medical history, similar to our results.
Pharmacists are in a strategic position to optimize the health of the public by providing appropriate advice to patients who self-medicate (Brata et al., 2015). Our findings showed that all the pharmacists provided instructions regarding drug administration each time, but the number of pharmacists who notified the pseudo customers about contraindications and potential side effects was minimal (6.7%). None of them explained what a patient should do in case of missed doses and how to store drugs, and no one referred the patients to a doctor. Other studies also reported that information on precautions, side effects, interactions, contraindications, and storage is unlikely to be given by pharmacists (Puspitasari et al., 2009). A review of the provision of appropriate advice on self-medication in the developing countries found that the proportion of pharmacy employees who offer suitable recommendations varied widely from 0% to 96% (Brata et al., 2015). Research also revealed that only 35.3% of pharmacists specified instances that warrant a visit to a physician (Pham et al., 2013). Our study registered no such referrals from the participants. Written information is essential as a supplement and reinforcement to verbal information when verbal interaction is insufficient in educating a customer (Hamrosi et al., 2014). We found that 40% of the participating pharmacists used written forms as a means of counseling patients.
None of the pharmacists took the time to verify a patient’s understanding. Only 6.7% summarized important points that a patient needed to remember, and 16.7% checked for additional concerns or questions from the patients. The bulk of interactions revolved around collecting patient information and providing advice rather than verifying understanding.
 | Table 5. Dispensed drugs in the adult and child scenarios. [Click here to view] |
These findings need to be taken into account when conducting new educational intervention for pharmacists. We should design specific education modules on topics which pharmacists are still incompetent, such as medication history interview, management of adverse drug reaction and drug interaction, and referrals to doctors.
Assessment of dispensing practice
For the pseudo customers acting out the adult scenario, the mean number of drugs dispensed was 4.56 ± 0.86 (Table 5). All the customers were given paracetamol (as a single product or as a part of a combination of drug regimens) to reduce fever. The pharmacists also sold them non-sedative (71.4%) and sedative (14.3%) anti-histamines. In particular, the POMs usually dispensed without the pharmacist requiring prescriptions were antibiotics (100%), dextromethorphan (57.1%), oral corticosteroids (14.3%), and chymotrypsin (42.9%). For the pseudo customers playing out the child-based scenario, the number of drugs sold was fewer than those purchased in the adult scenario, with the mean being 3.43 ± 0.98 (Table 3). Nevertheless, many of the dispensing-associated problems encountered in the adult scenario occurred as well in the situation involving children.
Results of the role play sessions reflected a difference between knowledge of dispensing and actual practice—a finding that contrasted with our expectations. The pharmacists dispensed inappropriate medicines, especially antibiotics. In the paper-based test administered after the educational interventions, 97.4% of the pharmacists correctly answered that “antibiotics should not be used to treat the common cold,” but in 100% and 56.3% of the adult and child scenarios, respectively, they recommended antibiotic monotherapy for the condition. Despite the issuance of regulations and guidelines for antibiotic dispensing, the illegal sale of most antibiotics without prescriptions is a common practice in Vietnam (Larsson et al., 2000). According to a community–based study undertaken in the country, 78% of antibiotics were purchased in private pharmacies without the employees asking for prescriptions (Larsson et al., 2000). Antibiotics were also often used for about 3 days or less (Nguyen et al., 2011). The inappropriate use of antibiotics in the country is challenging as it has resulted in high levels of resistance to such medications (National Working Group—The Center for Disease Dynamics, Economics & Policy, 2010). Non-sedative antihistamines accounted for a high proportion of purchased drugs even though our educational interventions highlighted that these drugs are ineffective against common cold symptoms. As recommended by the US Food and Drug Administration, children under 2 years of age should not be given any kind of cough and cold product that contains a decongestant or antihistamine because serious and possibly life-threatening side effects can occur (FDA, 2018). In our study, antihistamines were sold to adults and 5-year-old children (scenarios) 37.5% and 85.7% of the time, respectively. Of these medications, the non-sedative variants made up 71.4% and 12.5% of the total, respectively.
As previously stated, the pharmacists dispensed several POMs, such as dextromethorphan, oral corticosteroids, antibiotics, celecoxib, salbutamol, and chymotrypsin without asking for prescriptions. Vietnamese private pharmacists often ignore the importance of POM legislation (Chalker et al., 2005; Larsson et al., 2000; Nguyen et al., 2011; 2019). A number of studies suggested that to poor case management and counseling at pharmacies are driven primarily by time constraints, lack of knowledge and communication skills, low customer expectations, profit-driven motivations, and the negative effects of dissatisfaction among customers (Brata et al., 2013; 2015). Ensuring sustainable practice necessitates appropriate training. Correspondingly, multi-faceted interventions should be implemented covering issues, such as law enforcement, strict supervision, and building up community networks of pharmacies for training and systematic management by the Vietnamese Ministry of Health (Pham et al., 2013).
Limitations
This study is one of the first to use educational interventions and the pseudo customer method to evaluate the theoretical knowledge and actual practice of community pharmacists with respect to common cold management in Vietnam. Nevertheless, the study’s limitations need to be considered when interpreting the results. First, there were no pseudo customer visits which conduct before educational intervention. Instead, we directly observed counseling in the community pharmacies, for which the results discussed here were reported in another article (Vo and Le, 2018). Second, the sample size was small because of limited resources, but this study still uncovered problematic issues in the counseling practice for common cold management. Third, World Health Organization suggested five patient care indicators (including average consultation time, average dispensing time, percentage of drugs actually dispensed, percentage of drugs adequately labeled, and patients’ knowledge of correct dosage); however, we evaluated only three indicators.
CONCLUSION
The results indicated that educational interventions can be an effective tool for enhancing the knowledge of community pharmacists as regards common cold management. The pseudo customer method enabled the evaluation of actual practice among the respondents. Despite the promising findings, however, a gap still exists between the knowledge and practice of community pharmacists in the investigated context. Further studies with long-term and multi-component interventions should be launched, with focus on the irrational use of antibiotics and inappropriate dispensing of POMs. More rigorous research should also be directed toward carrying out effective interventions designed to elevate the quality of counseling by community pharmacists.
REFERENCES
ASHP. ASHP guidelines on pharmacist-conducted patient education and counseling. Am J Health Syst Pharm, 1997; 54(4):431–4. CrossRef
Berger K, Eickhoff C, Schulz M. Counselling quality in community pharmacies: implementation of the pseudo customer methodology in Germany. J Clin Pharm Ther, 2005; 30(1):45–57. CrossRef
Brata C, Gudka S, Schneider CR, Clifford RM. A review of the provision of appropriate advice by pharmacy staff for self-medication in developing countries. Res Social Adm Pharm, 2015; 11(2):136–53. CrossRef
Brata C, Gudka S, Schneider CR, Everett A, Fisher C, Clifford RM. A review of the information-gathering process for the provision of medicines for self-medication via community pharmacies in developing countries. Res Social Adm Pharm, 2013; 9(4):370–83. CrossRef
Chalker J, Ratanawijitrasin S, Chuc NT, Petzold M, Tomson G. Effectiveness of a multi-component intervention on dispensing practices at private pharmacies in Vietnam and Thailand - a randomized controlled trial. Soc Sci Med, 2005; 60(1):131–41. CrossRef
Chandra A, Malcolm N, Fetters M. Practicing health promotion through pharmacy counseling activities. Health Promot Pract, 2003; 4(1):64–71. CrossRef
FDA. 2018. Use caution when giving cough and cold products to kids. Available via https://www.fda.gov/drugs/resourcesforyou/specialfeatures/ucm263948.htm. (Accessed 28 March 2020).
Hamrosi KK, Raynor DK, Aslani P. Enhancing provision of written medicine information in Australia: pharmacist, general practitioner and consumer perceptions of the barriers and facilitators. BMC Health Serv Res, 2014; 14:183. CrossRef
Larsson M, Kronvall G, Chuc NT, Karlsson I, Lager F, Hanh HD, Tomson G, Falkenberg T. Antibiotic medication and bacterial resistance to antibiotics: a survey of children in a Vietnamese community. Trop Med Int Health, 2000; 5(10):711–21. CrossRef
Liu MY, Jennings JP, Samuelson WM, Sullivan CA, Veltri JC. Asthma patients’ satisfaction with the frequency and content of pharmacist counseling. J Am Pharm Assoc, 1999; 39(4):493–8. CrossRef
National Working Group—The Center for Disease Dynamics, Economics & Policy. 2010. Situation analysis: antibiotic use and resistance in Vietnam—Executive Summary. Available via https://cddep.org/wp-content/uploads/2017/06/vn_summary_web_1_8.pdf. (Accessed 28 March 2020).
Nguyen QH, Nguyen TK, Ho D, Larsson M, Eriksson B, Lundborg CS. Unnecessary antibiotic use for mild acute respiratory infections during 28-day follow-up of 823 children under five in rural Vietnam. Trans R Soc Trop Med Hyg, 2011; 105(11):628–36. CrossRef
Nguyen TPT, Vu DH, Luong TTH, Do XT, Nguyen HA, Nguyen TB. Antibiotics dispensing without prescription in community pharmacies in the world: systematic review and meta-analysis. J Pharmaceut Res Drug Inf, 2019; 10(1):2–11.
Pham DM, Byrkit M, Pham HV, Pham T, Nguyen CT. Improving pharmacy staff knowledge and practice on childhood diarrhea management in Vietnam: are educational interventions effective? PLoS One, 2013; 8(10):e74882. CrossRef
Puspitasari HP, Aslani P, Krass I. A review of counseling practices on prescription medicines in community pharmacies. Res Social Adm Pharm, 2009; 5(3):197–210. CrossRef
Viet Nam’s Ministry of Health. 2010. Circular No. 43/2010/TT—BYT: Regulatory Roadmap Implementation Principles, Standards Of “Good Practice Pharmacy (GPP): Geographical Scope And Activities of Drug Retail Premises”. Available via http://vbpl.vn/boyte/Pages/vbpq-van-ban-goc.aspx?ItemID=26086. (Accessed 28 March 2020).
Vo TH, Bedouch P, Nguyen TH, Nguyen TL, Hoang TKH, Calop J, Allenet B. Pharmacy education in Vietnam. Am J Pharm Educ, 2013; 77(6):114. CrossRef
Vo TH, Le TQ. Direct observation of counseling of OTC drug use in community pharmacies at Hue. J Med Pharm, 2018; 8(4):20–4. (Vietnamese). CrossRef
Vo TH. 2018. The pocket handbook of counseling for community pharmacists – 30 common minor symptoms. Lao Dong Publisher, Hanoi, Vietnam. (Vietnamese).
Wu JY, Leung WY, Chang S, Lee B, Zee B, Tong PC, Chan JCN. (2006). Effectiveness of telephone counselling by a pharmacist in reducing mortality in patients receiving polypharmacy: randomised controlled trial. BMJ, 333(7567): 522. CrossRef
Yang S, Kim D, Choi HJ, Chang MJ. A comparison of patients’ and pharmacists’ satisfaction with medication counseling provided by community pharmacies: a cross-sectional survey. BMC Health Serv Res, 2016; 16:131. CrossRef