INTRODUCTION
The global prevalence of cirrhosis from autopsy studies ranges from 4.5% to 9.5% of the general population (Graudal et al., 1991; Lim and Kim, 2008; Melato et al., 1993; Sarin and Maiwali, 2019). Liver Cirrhosis, if left neglected, can result in the death of the patient. The severity of the liver disease will give an idea about the chances of prognosis of the patient. It also allows us to choose the therapeutic strategies to follow and lifestyle modifications that are to be necessarily adopted into the daily routine. However, the awareness of the prognosis of the disease to the patient is a double-edged sword. The patient may perceive the information positively or negatively. In this context, we should assess the patient’s mental status before providing information. The Child-Pugh score, often-cited tool in the literature, predicts the severity of the liver disease, namely, liver abnormalities like portosystemic shunt surgery, liver cirrhosis. This score quantifies the patient’s disease severity with respect to serum albumin, bilirubin, International Normalised Ratio (INR), ascites, and grades of encephalopathy.
Most of the patients admitted in the hospital were unaware of their severity and finds difficulty to quit the alcohol. Confused about how the patient will receive the information, most of the physicians will reveal the information to the patient caregivers. There is a need to explain the severity of the disease, lifestyle factors that are to be adopted, dietary changes to promote recovery of the disease. Unfortunately, the physicians may not find enough time to do all this because of their work schedule and the low doctor to patient ratio. Therefore, we decided to assess the severity of the disease and the depression status of the patients. Based on the depression status of the patient’s, detailed counseling about the prognosis of the disease, lifestyle modifications, and precautions to be followed will be given to the patient and/or patient caregiver. The present study aimed to bring an awareness of the prognosis of the liver disease to the patient and/or patient caregiver based on the patient’s depression status and offer patient counseling for anxiety and depressed patients. Also, deaddiction centers will be suggested to help coping with the deaddiction of alcohol.
MATERIALS AND METHODS
Study design, study site, and duration
A cross-sectional study was carried out on 100 inpatients, in the Department of General Medicine, Tertiary Care Hospital, Kakinada, for 8 months. Simple random sampling was used to select the patients. The study was approved by the Institutional Ethics Committee (RC No./Clinicals/Pharm.D/N2/13/2018).
Sampling technique
Simple Random Sampling technique was employed for selecting the subjects. Sampling frame with subjects with chronic liver disease patients was prepared. From that framework, subjects were chosen randomly using a random number generator method.
Sample size
The margin of error was 5%, with a 95% confidence level, 120 as population size, and 50% as response distribution; the sample size obtained was 92. We collected an extra eight cases to make it to 100 patients.
Participants
Inclusion criteria
Patients of both sexes, meeting clinical features of a diagnosis, such as jaundice, nodular liver, splenomegaly, ascites, weight loss, and encephalopathy. Abnormal bilirubin, albumin, prothrombin time, Alanine Aminotransferase and Aspartate Aminotransferase values, and liver biopsy were included in the study.
Exclusion criteria
Critically ill patients, who underwent recent surgery related to liver, patients who are not willing to participate, and patients with other co-morbidities were excluded from the study.
Study instruments
Child-Turcotte-Pugh score
The Child-Pugh score was mostly cited tool in the literature for predicting the severity of the liver disease, namely, liver abnormalities, such as portosystemic shunt surgery and liver cirrhosis. This score quantifies the patient’s disease severity with respect to serum albumin, bilirubin, INR, ascites, and grades of encephalopathy. It categorizes the severity as class A (5–6 points, least severe, 1-year survival 100%), class B (7–9 points, moderately severe, 1-year survival 80%), class C (10–15 points, most severe, 1-year survival 45%). Child-Pugh Score, part of hepatocellular carcinoma (HCC), helps in therapeutic decision making.
Hospital anxiety and depression scale
Hospital Anxiety and Depression Scale was used to measure the anxiety and depression of the patients. It was a 14-item scale, of which seven items relate to anxiety and seven items relate to depression. A score of 0–7 was normal, 8–10 borderline abnormal, and 11–21 are considered as abnormal.
Data collection
Direct counseling was provided to the patient with scores up to 10, whereas for abnormal patients, counseling was provided to patient caregivers. The counseling session contains three parts. The first part deals with a brief introduction about the chief complaints of the disease with respect to the etiology and pathophysiology of the disease in simple terms. The second part contains counseling on discharge medications and precautions to be followed. The final part deals with the important lifestyle modifications and dietary conditions to be adopted in the daily routine, along with the information of deaddiction centers.
The aim and objectives of the study were clearly explained to the patients and obtained written informed consent from patients who are willing to participate in the study. A semi-structured data collection form was designed. The data collection contained two phases. In the first phase, demographic details were obtained. In the second phase, subjective data and objective data related to the disease were collected from the patient and case sheet/ lab reports, respectively. The Child-Pugh Score was then calculated individually for each patient. This data was tabulated and analyzed.
Data analysis
Grubbs test was used to find out the outliers in the data. Shapiro–Wilk test was used to test the normality of the data. Mean and the standard deviation were calculated for quantitative data with normality and without outliers. Median and interquartile range was calculated for the quantitative data without normality and with outliers. The association between the objective data with the severity of the disease and prognosis of the liver disease was calculated using the Chi-Square test. The level of significance was considered at p < 0.05, whereas p < 0.01 was considered as statistically highly significant.
RESULTS AND DISCUSSION
The mean age of the patients was 47.29 ± 13.17 years. Males are predominantly high than in females. Alcoholic liver disease often observed the etiology of liver disease in our study. Rural people, uneducated, employed, and married are high in number than their counterparts. Among the demographics, occupation, substance abuse and marital status are statistically associated with the severity of the disease (Table 1). Table 2 presents the descriptive statistics of the quantitative data.
The three common clinical manifestations of the liver disease were a pain in the abdomen, edema, and ascites (Table 3). Borderline abnormal anxiety and depression was high in the patients (Table 4). Except for Alkaline Phosphatase (ALP), remaining liver function tests were having a statistically significant association with the severity of the disease (Table 5). Except for Serum Glutamic Oxaloacetic Transaminase (SGOT) and ALP, remaining liver function tests were having a statistically significant association with prognosis of the liver disease (Table 6).
The mean age group of patients was 47.29 ± 13.17 years. Mukherjee et al. (2017) in his multicentric study reported a similar mean age group of patients in south patients. Bhattacharya et al. (2016) reported a mean age group of 45.8 ± 10.45 years in liver cirrhosis patients. Shalimar et al. (2016) reported a mean age group of 42.68 ± 11.84 years in non-survivors, whereas in survivors the mean age group was 42.47 ± 11.97 years.
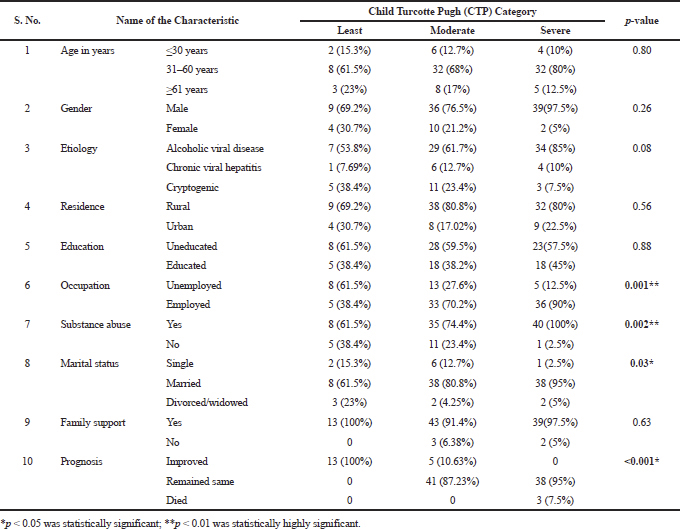 | Table 1. Relationship between socio-demographic factors & Severity of disease (n = 100). [Click here to view] |
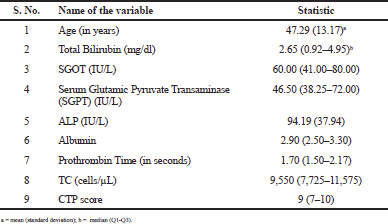 | Table 2. Descriptive statistics of quantitative variables. [Click here to view] |
We observed a high number of male patients than female patients. Similar results were reported in some studies (Mukherjee et al., 2017; Shalimar et al., 2016). Alcohol-induced liver disease cases are often observed in our study (70%). Similarly, Shalimar et al. (2016) reported a high prevalence of alcohol- induced liver disease cases. However, Mukherjee et al. (2017) reported only 12% of alcohol-induced liver disease cases in the south region. Sedentary lifestyle habits like alcohol drinking, in males, are usually higher than females. This predisposes them to chronic liver disease. Impulsive behaviors, such as drinking and smoking were also considerably high in males than in females.
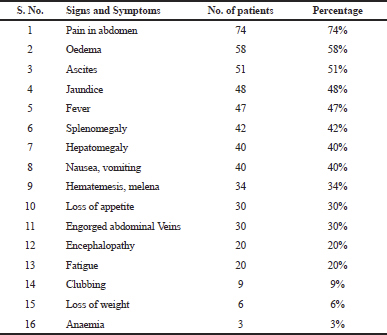 | Table 3. Presenting signs and symptoms of the patients. [Click here to view] |
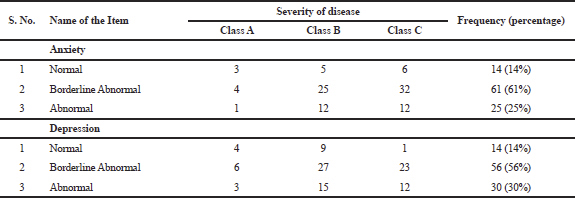 | Table 4. Anxiety and depression of the patients. [Click here to view] |
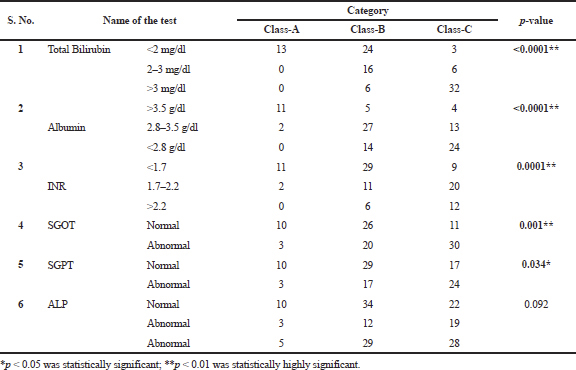 | Table 5. Association of Liver function tests and Severity of disease. [Click here to view] |
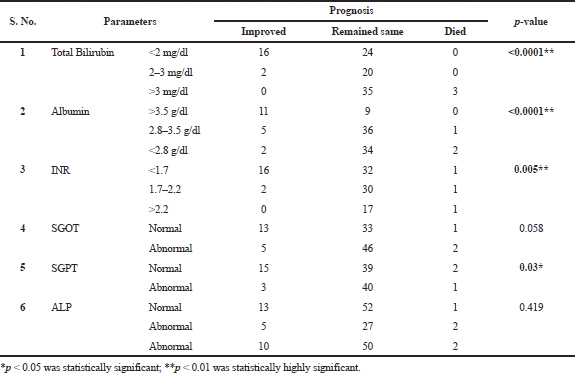 | Table 6. Association of liver function tests and prognosis of patients. [Click here to view] |
The three most presenting clinical signs and symptoms according to their occurrence were abdominal pain (74%), edema (58%), and ascites (51%). Kumar et al. (2016) reported ascites (87.1%), jaundice (69.4%), Gastro Intestinal (GI) bleeding, and decreased appetite (48.4%) as the three most common clinical signs and symptoms of chronic liver disease. Bhattacharya et al. (2016) reported leg swelling (80.5%), abdominal swelling (74.3%), and GI bleeding (43.4%) as the three most common presenting clinical signs and symptoms of chronic liver disease.
Child-Pugh Score was well known prognostic indicator for a number of liver diseases (Benhar and Kumar, 2017; Peng et al., 2015; 2016). The median CTP score was nine, corresponds to class B. Nearly scores corresponding to class B were reported in some studies (Peng et al., 2015; Zippirich et al., 2012). We observed a highly significant association between prognosis and severity of the disease (p < 0.001). Benhar and Kumar (2017) reported a significant association between CTP score and mortality. Except for ALP, we observed a statistically significant association between liver function tests and Child-Pugh scores. Of them, we found highly significant association (p < 0.01) between total bilirubin (p < 0.0001), albumin (p < 0.0001), and severity and prognosis of the disease. Zhu et al. (2016) reported that albumin-bilirubin score predicted postoperative liver failure and overall death in patients with HCC undergoing liver resection more accurately than the CTP score.
We observed a higher percentage of patients with borderline abnormal anxiety (61%) and depression (51%) in our study. Alcoholic liver disease and depression are interlinked with each other. Alcohol increases the risk of depression apart from liver disease and depression increases the risk of alcohol consumption (Carguilo, 2007; Crum et al., 2005; Gilman and Abraham, 2001). However, several studies have identified a high prevalence of depression even in patients with non-alcoholic fatty liver disease. Weinstein et al. (2011) observed a high prevalence of depression in patients with non-alcoholic fatty liver disease and hepatitis-c; excessive alcohol consumption is consistently related to depression. Youssef et al. (2013) observed the association of psychiatric disorders and histological severity of liver disease on 527 cohorts and reported subclinical and clinical depression in 53% and 14% of non-alcoholic fatty liver disease patients, respectively. These results are strengthened by another study (Tomeno et al., 2015).
Silva et al. (2015) also reported that depression rather than grade of liver fibrosis was strongly associated with the impairment in the quality of life of patients with hepatitis C. Zhu et al. (2016) also reported a link between depression rates of chronic hepatitis B infected patients with liver cirrhosis and the severity of the liver cirrhosis. We explained the prognosis of the disease for class B and class C patients very clearly. We offered patient counseling for patients with borderline abnormal and abnormal anxiety and depression, class B and class C severity of the disease. We also provided the list of deaddiction centers for alcoholics, both governments aided and private centers.
CONCLUSION
Borderline abnormal anxiety and depression, class B and class C severity of the disease were high in the patients. High-risk patients came to know the severity of the disease and consequences thereafter (to avoid neglecting their health at least hereafter), with patient counseling along with a list of deaddiction centers. Integrating a psychologist can benefit patients struggling with deaddiction to alcohol.
CONFLICTS OF INTEREST
The authors declare that there is no conflicts of interest.
FUNDING
None.
AUTHOR CONTRIBUTION
Vinodkumar Mugada—design, analysis and interpretation of data, manuscript editing, and proof reading.
Keerthi Chandana Veera—data collection, literature search, and data analysis.
Jaya Divya Paravada—data collection, literature search, and data analysis.
REFERENCES
Benhar NVA, Kumar HV. Epidemiology and clinical profile of hepatic encephalopathy in tertiary care hospital, GGH, Kakinada. J Evid Based Med Healthc, 2017; 4(24):1379–88. CrossRef
Bhattacharya M, Narendra Nath B, Bhabadev G. Clinical profile of cirrhosis of liver in a tertiary care hospital of Assam, North East India. IOSR J Dental Med Sci, 2016; 15(1):21–7.
Carguilo T. Understanding the health impact of alcohol dependence. Am J Health Syst Pharmacists, 2007; 64:S5–11. CrossRef
Crum RM, Storr CL, Chan YF. Depression syndromes with risk of alcohol dependence in adulthood: a latent class analysis. Drug Alcohol Depen, 2005; 79:71–81. CrossRef
Gilman SE, Abraham HD. A longitudinal study of the order of onset of alcohol dependence and major depression. Drug Alcohol, 2001; 63:277–86. CrossRef
Graudal N, Leth P, Marbjerg L, Galloe AM. Characteristics of cirrhosis undiagnosed during life: a comparative analysis of 73 undiagnosed cases and 149 diagnosed cases of cirrhosis, detected in 4929 consecutive autopsies. J Intern Med 1991; 230:165–71. CrossRef
Kumar PC, Shiv Nath S, Anil Kumar P. Study of clinic-etiological profile and the complication pattern in patients with chronic liver disease at tertiary care centre. Int J Contemp Med Res 2016; 3(6):1668–70.
Lim YS, Kim WR. The global impact of hepatic fibrosis and end stage-stage liver disease. Clin Liver Dis, 2008; 12:733–46. CrossRef
Melato M, Sasso F, Zanconati F. Liver cirrhosis and liver cancer. A study of their relationship in 2563 autopsies. Zentralbl Pathol, 1993; 139:25–30.
Mukherjee PS, Vishnubhatla S, Amarapurkar DN, Das K, Sood A, Chawla YK, Eapen CE, Boddu P, Thomas V, Varshney S, Hidangmayum DS, Bhaumik P, Thakur B, Acharya SK, Chowdhury A. Etiology and mode of presentation of chronic liver diseases in India: a multi centric study. PLoS One, 2017; 12(10):e0187033. CrossRef
Peng Y, Qi X, Dai J, Li H, Guo X. Child-Pugh Score versus MELD score for predicting the in-hospital mortality of acute upper gastrointestinal bleeding in liver cirrhosis. Int J Clin Exp Med, 2015; 8(1):751–57.
Peng Y, Qi X, Guo X. Child-Pugh versus MELD score for the assessment of prognosis in Liver Cirrhosis: a systematic review and metanalysis of observational studies. Medicine (Baltimore), 2016; 95(8):e2877. CrossRef
Sarin SK, Maiwali R. Global burden of liver disease: a true burden on health sciences and economies, 2019. [Internet]. http://www.worldgastroenterology.org. Available via http://www.worldgastroenterology.org/publications/e-wgn/e-wgn-expert-point-of-view-articles-collection/global-burden-of-liver-disease-a-true-burden-on-health-sciences-and-economies (Accessed 2 April 2019)
Shalimar, Vivek S, Shivaram P S, Ajay D, Akash S, Chundamannil EE, Dharmendra K, Gaurav P, Jayanti V, Pankaj P, Krishnaswamy N, Radha KD, Sandeep T, Sandeep N, Shobna B, Uday Z, Ujjwal S, Thomas V, Subrat KA. Acute on Chronic liver failure in India: the Indian National Association for study of the Liver consortium experience. J Gastroenterol Hepatol 2016; 31:1742–49. CrossRef
Silva LD, Cunha CC, Cunha LR, Araujo RE, Barcelos VM, Menta PL, Neves FS, Teixeira R, Rocha GA, Gontijo ED. Depression rather than liver impairment reduces quality of life in patients with hepatitis C. Braz J Psychiatry 2015; 37(1):21–30. CrossRef
Tomeno W, Kawashima K, Yoneda M, Saito S, Ogawa Y, Honda Y, Kessoku T, Imajo K, Mawalari H, Fujita K, Saito S, Hirayasu Y, Nakajima A. Non-alcoholic fatty liver disease comorbid with major depressive disorder: the pathological features and poor therapeutic efficacy. J Gastroenterol Hepatol 2015; 30:1009–14. CrossRef
Weinstein AA, Kallman Price J, Stepanova M, Poms LW, Fang Y, Moon J, Nader F, Younossi ZM. Depression in patients with non-alcoholic fatty liver disease and chronic viral hepatitis B and C. Psychosomatics 2011; 52:127–32. CrossRef
Youssef NA, Abdelmalek MF, Binks M, Guy CD, Omenetti A, Smith AD, Diehl AM, Suzuki A. Associations of depression, anxiety and antidepressants with histological severity of non-alcoholic fatty liver disease. Liver Int 2013; 33:1062–70. CrossRef
Zhu HP, Gu YR, Zhang GL, Su YJ, Wang KE, Zheng YB, Gao ZL. Depression in patients with chronic hepatitis B and cirrhosis is closely associated with the severity of liver cirrhosis. Exp Ther Med 2016; 12(1):405–09. CrossRef
Zippirich A, Garcia-Tsao G, Rogowski S, Fleig WE, Seufferlein T, Dollinger MM. Prognostic indicators of survival in patients with compensated and decompensated cirrhosis. Liver Int 2012; 32(9):1407–14. CrossRef