INTRODUCTION
Recently, there is a growing global trend for consumers to practice self-care and self-medicate for common minor ailments by using non-prescription medicines (Benrimoj et al., 2007b). The role of community pharmacists as educators and prescribers on the non-prescription medicines became crucial as they are the healthcare professionals most readily accessible to the public to ensure the appropriate use of medicines (Chua et al., 2006). Worldwide, there are countries adopting the component of achieving quality use of medicine under the national medicine policy with the aim to provide better health outcomes (Benrimoj et al., 2008; Ministry of Health Malaysia, 2007). The quality use of medicines should include the use of non-prescription medicines for minor illnesses management. Indeed, there is a new model of healthcare which is classified as “pharmacist-assisted self-care” whereby substantial business and professional opportunities are created for community pharmacists, and at the same time providing a higher level of healthcare value for consumers (Covington, 2006). Community pharmacists will assess the suitability of self-care treatment, recommend the best choices of treatment by using non-prescription medicines, and provide counseling on the use of medicines.
In Malaysia, the absence of dispensing separation between private doctor clinics and pharmacies is the main challenge of the community pharmacists. Additionally, the lack of government medicine prices control policy in private health sectors has further enhanced medicine prices competition between pharmacies (Sivanandam et al., 2018). Consequently, the community pharmacists tend to reduce the profit margins for prescription medicines and revitalize the non-prescription medicines sales and services, including Class C Poison and over-the-counter medicines, for minor ailments treatment. Although there is no clear definition of a minor ailment, symptoms which are associated with a short term, trivial, and self-limiting illness are considered as a minor ailment (Lo, 2006).
Currently, there is no local guideline and model of practice available in Malaysia to guide the community pharmacists’ practices of minor ailments management. Therefore, the Malaysian government could consider adopting policy used by the neighboring developed countries. For instance, Australian community pharmacists have standards of practice developed by the pharmacy profession to guide the provision of non-prescription medicines using a consumer-focused and risk management approach (Benrimoj et al., 2007b). Consumer-focused is an approach that concentrates on the consumers’ health outcomes rather than the sales of products. The risk management approach will guide the pharmacy assistants to perform screening and refer at-risk consumers to the pharmacists when necessary (Benrimoj and Wilson, 2006). The standards of practice for the provision of non-prescription medicines require a constant monitoring by professional bodies to ensure the responsibilities of community pharmacists are met (Benrimoj et al., 2007a).
Malaysia has a unique medicine classification as compared to other countries. According to the Malaysian Poison Act 1952, all Class C Poison can be dispensed by a registered pharmacist in a licensed pharmacy premise without a prescription (Pharmaceuticals Services Division, 2019). Class C Poisons consist of medicines such as antihistamines, nonsteroidal anti-inflammatory drugs (NSAIDs), topical corticosteroids, and topical antibiotics that cover minor ailments (Legal Research Board of Malaysia, 2006). For instance, naproxen and topical betamethasone (corticosteroid) which are classified as Class C Poisons in Malaysia regardless of the dose and packing can be used for pain management and dermatitis, respectively, by the community pharmacists without the need of prescriptions (Pharmaceuticals Services Division, 2019), whereas in the developed country like Australia, naproxen that exceeds 250 mg per dosage unit in packs more than 30 and topical betamethasone are classified as prescription-only medicines (Therapeutic Goods Administration, 2019). The wide range of Class C Poisons in Malaysia allows the community pharmacists to play a distinctive role in minor ailments management.
A previous study in Malaysia found that approximately 42% of the Malaysian consumers purchased their medications from community pharmacies (Babar and Ibrahim, 2003). This provides a greater opportunity for pharmacists to serve better pharmaceutical care to the public through pharmacist guided self-medications (Chong et al., 2011). Unassisted non-prescription medicines use may lead to adverse therapeutic consequences for the consumers. Hence, there is a need for community pharmacists to prevent harm through interventions during the provision of minor ailments consultation (Covington, 2006). In fact, a study revealed that 20.9% of the community pharmacists’ interventions on non-prescription medicines use were potentially lifesaving (William et al., 2011).
To date, there is limited data on Malaysian community pharmacists’ usage of non-prescription medicines in the management of minor ailments. A baseline data should be provided to develop guidelines and models of practice for community pharmacists in minor ailments management. This study, therefore, aims to evaluate the use of non-prescription medicines (Class C Poison and over-the-counter medicinal products) in the management of minor ailments by the Malaysian community pharmacists. The total charges imposed on the consumers (medication prices, consultation fee, or any additional service charges) and consumers’ follow-up were also assessed.
METHODS
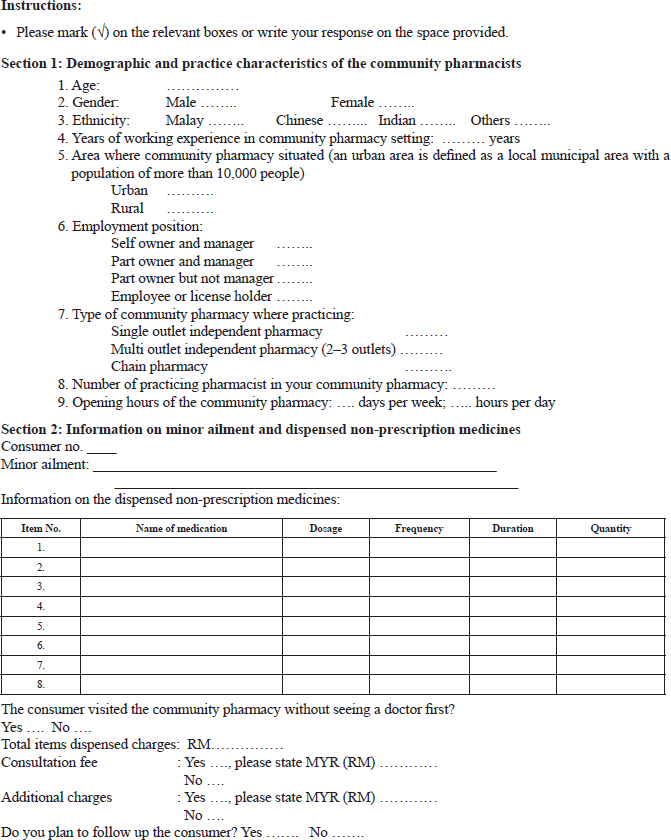
This was a descriptive cross-sectional survey using a self-completed anonymous data collection form to be filled in by the community pharmacists. The data collection form was tested for face and content validity by two experts and five registered pharmacists. It was further adjusted after pilot testing with five community pharmacists. The data collection form consists of sections on demographic and practice characteristics of the community pharmacists, minor ailments managed by the community pharmacists, medications dispensed, and the total charges imposed on the consumers. Besides, there was a question to assess whether the consumer visited the community pharmacy without seeing a doctor first for the minor ailment treatment. A question to assess whether the pharmacist planned to follow-up the consumer was also included in the data collection form. This study has obtained ethics approval from the Joint Ethics Committee of School of Pharmaceutical Sciences, Universiti Sains Malaysia-Hospital Lam Wah Ee on Clinical Studies [approval number: USM—HLWE/IEC/2012(0001)].
All the 2,730 community pharmacists practicing in Malaysia as listed in the Division of Pharmacy Service, State Government of all the states in Malaysia were invited for participation in this study. The inclusion criteria were the community pharmacists who received at least 10 consumers' requests for minor ailment treatment per day. Data were collected across the first 10 requests for minor ailments management for adult consumers encountered by the community pharmacists in one working day upon receiving the invitation to participate in this research. The data collection included only the request from the consumers who walk in without a prescription and seek for community pharmacist’s help in minor ailments treatment. The pharmacists were requested to provide the information on the non-prescription medicines dispensed for the minor ailments. Additionally, the pharmacists were required to assess whether the consumer visited the community pharmacy for the minor ailment treatment without seeing a doctor first. The pharmacists were also requested to provide information on whether they planned to follow-up the consumer. This study excluded the requests for minor ailments management in children. The community pharmacists received the data collection forms through a personal approach (for the pharmacists in the state of Penang) and mail (for other states throughout Malaysia). Two invitation letters and two follow-up letters were used to increase the response rate. Written informed consent was obtained from all the responding pharmacists and no personal data of the participants were recorded. Data were collected from 4th December 2013 to 24th April 2016.
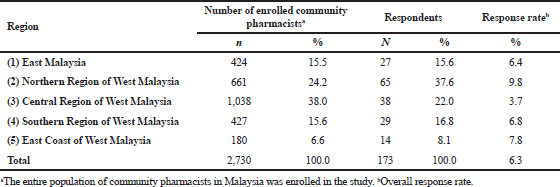 | Table 1. Total number of community pharmacists, response rate and distribution of respondents according to region in Malaysia. [Click here to view] |
Data analysis was performed by using IBM SPSS® Statistics Version 24. Frequency and cross-tabulation were used for descriptive analysis. All the data were initially tested for normality distribution. As the data were not normally distributed, the average value of the data was presented as median and inter-quartile range (IQR). Non-parametric test including Chi-square, Mann–Whitney U, and Kruskal–Wallis test were used to evaluate the differences in the practices of the pharmacists. A p-value of less than 0.05 was set to determine statistical significance.
RESULTS
Demographic and practice characteristics of community pharmacists
A total of 173 community pharmacists were participated in this study for a response rate of 6.3% with the highest response rate of 9.8% originating from the Northern Region of West Malaysia (Table 1). The majority of the community pharmacists were female (67.1%) and aged between 31 and 40 years (38.2%). Considering the ethnicity, most of the pharmacists were Chinese (74.6%). The pharmacists mostly (34.1%) have five years or less of working experience in a community pharmacy setting. Most of the community pharmacists were practicing in the urban area (79.2%). Approximately, half (53.2%) of the pharmacists were employees or license holders of the pharmacies. The pharmacists mostly (48.0%) practiced at single outlet independent pharmacies and the majority (60.7%) responded that there was only one pharmacist in the respective pharmacies. Almost half (49.7%) of the pharmacists had their pharmacies operating for 7 full days per week (Table 2).
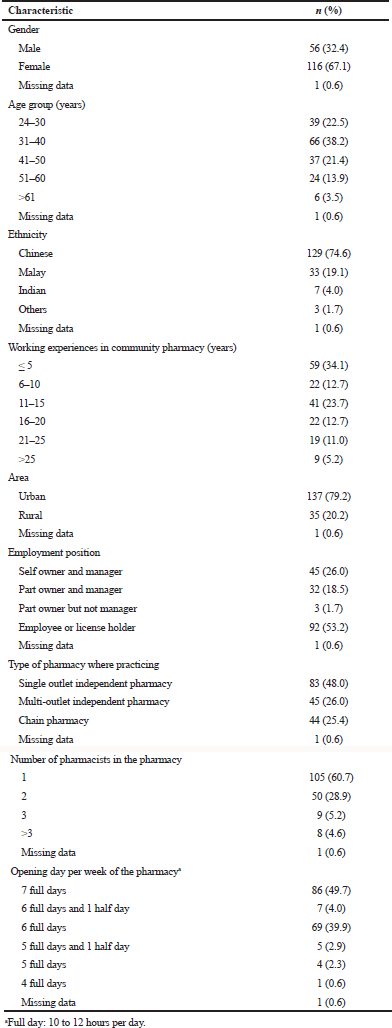 | Table 2. Demographics and practice characteristics of community pharmacists. [Click here to view] |
Number of minor ailments and medicines dispensed
A total of 1,704 consumers with minor ailments visited community pharmacies to seek treatment and the total number of minor ailments were 2,149. From the 1,704 consumers, 78.3% (n = 1,335) had one ailment, whereas 17.5% (n = 298) of consumers came in with two ailments, while the remaining 4.2% (n = 71) were with three ailments. The majority (84.1%; n = 1,433) of the consumers received either one or two medicines for their minor ailments. Only 15.9% (n = 271) of consumers received more than three items for their treatment. The median number of medicines dispensed per consumer was 2.00 (IQR: 1.00–2.00). Besides, consumers with acute minor ailments received significantly (Mann–Whitney U test: Z = −8.809; p < 0.001) higher number of medicines (median = 2.00; IQR: 1.00–2.00) than those with chronic minor ailments (median = 1.00; IQR: 1.00–2.00).
Type of minor ailments managed, and non-prescription medicines dispensed by community pharmacists
Most consumers (92.3%) sought help from community pharmacists for their acute minor ailments which required within seven days of treatment duration. Meanwhile, only 7.7% of the consumers have chronic conditions which required more than seven days of treatment. The minor ailments were mostly classified as respiratory (29.1%), oral and gastrointestinal (19.9%), and dermatologic (19.6%) conditions. The most common ailments were productive cough (7.3%), fever (6.3%), and dermatitis (6.1%). Among these ailments, dermatitis was the chronic condition which required a longer treatment period (Table 3). The management of these minor ailments mostly involved the anatomical therapeutic chemical therapeutic classes of NSAIDs (14.3%), cough & cold preparations (13.6%), and antihistamines & antiallergics (11.4%). The top three most commonly dispensed medicines were cetirizine tablet (5.9%), paracetamol tablet (4.7%), and diclofenac tablet (4.2%). The majority of community pharmacists (64.8%) used Class C poisons while some (33.2%) chose to use non-scheduled poisons (over-the-counter products) for the management of minor ailments when looking specifically at the medicine classification according to the Malaysian Poison Act 1952 (Table 4).
Duration of treatment and choice of treatment
Majority of consumers (n = 1,074; 63.0%) had their treatment duration between 1 and 5 days, while 385 (22.6%) consumers had between 6 and 10 days of treatment duration. Only a small portion of consumers (n = 242; 14.2%) required a treatment duration of more than 11 days. The duration of treatment for chronic conditions was significantly longer (Mann–Whitney U test: Z = −13.543; p < 0.001) than acute conditions (median 21.00 days; IQR: 10.00–30.00 vs. median 5.00 days; IQR: 3.00–7.00). Considering the choice of treatment, most of the consumers (75.5%, n = 1286) sought help from community pharmacists first to manage their minor ailments without seeing the doctors. Only 19.4% of consumers (n = 331) consulted the doctors for treatment before seeking help from community pharmacists.
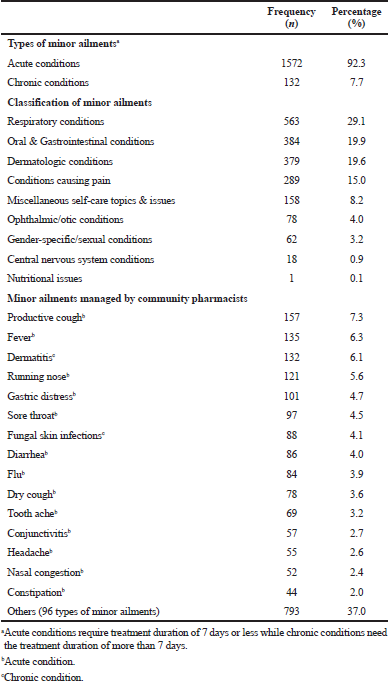 | Table 3. Minor ailments managed by community pharmacists. [Click here to view] |
Follow-up and treatment cost
In this study, the community pharmacists planned to follow-up on only 16.4% of the consumers for further monitoring and adjustment in treatment (Table 5). Nevertheless, the follow-up rate for chronic conditions (40.9%) was 4.23 times (odds ratio) significantly higher than acute conditions (14.3%). None of the community pharmacists charged any consultation fee or any additional charge to the consumers. All the treatments provided merely involved the medicine costs. The median cost of treatment per consumer according to the number of minor ailments was RM 13.40. The cost of treatment for consumers with three ailments (median = RM 19.90) was significantly higher than those with two ailments (median = RM 14.20) and one ailment (median = RM 12.50), respectively. By looking at the type of minor ailments, the average cost per consumer for chronic conditions (median = RM 27.78) was significantly greater than the acute conditions (median = RM 12.90) (Table 6).
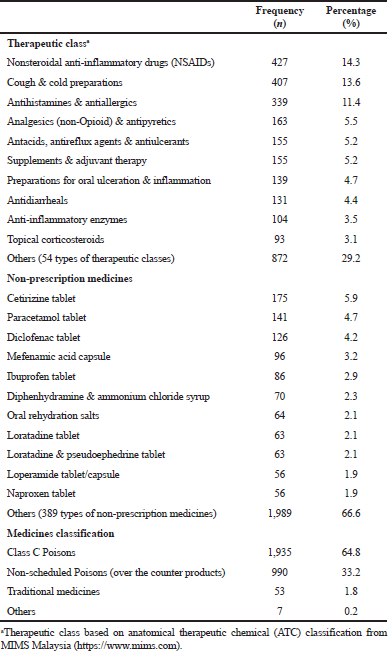 | Table 4. Non-prescription medicines dispensed by community pharmacists for the management of minor ailments. [Click here to view] |
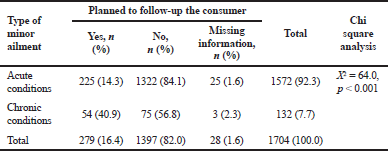 | Table 5. Community pharmacist planned to follow-up the consumer according to type of minor ailment. [Click here to view] |
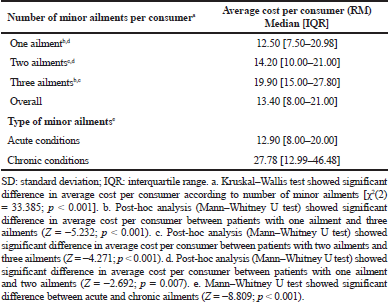 | Table 6. Community pharmacist planned to follow-up the consumer according to type of minor ailment. [Click here to view] |
DISCUSSION
The absence of dispensing separation policy in the Malaysian private healthcare sector has driven the community pharmacists to focus more on the non-prescription medicines use for minor illnesses rather than the dispensing of prescription medicines. Nevertheless, in countries with dispensing separation, the provision of prescription medicines is the core component of the community pharmacists’ practice (Mackridge et al., 2017; Merks et al., 2016). For instance, in North West England, three quarters (76%) of the interactions between consumers and pharmacy staff were linked with prescription medicines supply while only a minority of consumers were accessed to community pharmacists for consultation and services (Mackridge et al., 2017). Besides, a study conducted in the rural area of the United Kingdom found similar trend that the primary tasks of the community pharmacists were medicines dispensing and only 23.3% of the respondents consulted the community pharmacists for their minor ailments, such as bacterial/viral infections, minor injuries, stomach problems, and allergies (Merks et al., 2016).
The types of minor ailments and the medicines dispensed by the community pharmacists in this study were unique as compared to findings from other countries. The most common minor ailments found in this study were productive cough, fever, and runny nose and these ailments were mostly managed by diphenhydramine & ammonium chloride syrup, paracetamol tablet, and cetirizine tablet, respectively. Conversely, in Canada with seasonal changes, the common minor ailments encountered by community pharmacists were cold sores (34.4%), followed by insect bites (20%) and seasonal allergies (19.2%) (Mansell et al., 2015). Besides, a study in Jordan showed another trend with headache as the common minor ailment and it was mainly managed by paracetamol combined with caffeine (Hammad et al., 2018). Meanwhile, the community pharmacists in Baghdad were most likely to recommend diphenoxylate and loperamide as first-line treatment for acute diarrhea (Ibrahim et al., 2018). In Ethiopia, a study found that oral rehydration salt and zinc (33.3%), followed by mebendazole (23.9%) were frequently used by the community pharmacists for acute diarrhea treatment (Ayele et al., 2018). The irrational use of mebendazole for acute diarrhea treatment was due to the lack of access to clinical training among the Ethiopian community pharmacists and poor community awareness (Ayele et al., 2018).
In this study, the majority of the consumers with minor illnesses sought help first from the community pharmacists without consulting the physicians. This finding reflects the essential role of the Malaysian community pharmacists in the quality use of non-prescription medicines for minor ailment management. In fact, studies from overseas found a similar trend of community pharmacists’ role in minor ailment management. For instance, a study conducted among Canadian consumers showed most chose pharmacists over physicians because they trusted pharmacists as well equipped to handle minor ailments and the convenience of accessing the community pharmacies (Mansell et al., 2015). Only 27.2% would consult the physicians if the minor ailment services were not available (Mansell et al., 2015). Besides, the changes of national policy in the United Kingdom which allows pharmacists’ prescribing of a wide range of medicines had made consumers opt to visit community pharmacy for minor ailments treatment (Bojke et al., 2004; Mansell et al., 2015). In Malaysia, the National Medicine Policy emphasizes the models of best practice development and implementation to ensure the quality use of medicines (Ministry of Health Malaysia, 2007). However, currently, there are no local guidelines being developed to guide the community pharmacists in the provision of minor ailment treatment using non-prescription medicines. Hence, the Malaysian professional pharmacy bodies should cooperate with the Ministry of Health to establish guidelines or models of practice for minor ailments management by community pharmacists.
A lack of follow-up to the consumers by the community pharmacists for further treatment monitoring and adjustment was observed in this study. Insufficient patient medication record keeping and follow-up for consumers by the community pharmacists were similarly found in a previous study in Malaysia (Chong et al., 2011). The community pharmacists need to be enhanced in their patient follow-up practice. Follow-up is essential particularly for chronic minor skin problems as found in this study, such as dermatitis and fungal skin infections, which require long-term treatment and prevention. The low following-up and record-keeping practices might be due to the lack of local guideline and module of practice. Additionally, the absence of monitoring or audit system for community pharmacists’ performance evaluation is also a barrier for enhancing the minor ailments practices (Benrimoj et al., 2008). For instance, in Australia, a monitoring system was developed from the establishment of the Quality Care Pharmacy Support Centre to improve the standards for the non-prescription medicines provision by the community pharmacists (Benrimoj et al., 2008). Hence, the Malaysian community pharmacists should move toward establishing guidelines and a performance monitoring system for minor illnesses treatment.
Medicine affordability is one of the key components emphasized in the Malaysian National Medicine Policy (Ministry of Health Malaysia, 2007). This study revealed that the treatment costs charged by the community pharmacists were only involved medicine costs without any extra consultation fee. This could be due to the absence of a government policy that allows the community pharmacists to charge any consultation fee for every visit by the consumers. Therefore, the expenses for receiving treatment from community pharmacists for minor ailments are lower than from the private clinic doctors. The consumers generally need to pay a consultation fee (approximately RM 30) plus the medicines cost if they seek for private clinic doctors’ treatment (Ismail, 2018). However, this study found an affordable cost of treatment (median RM 13.40) for minor ailments management in community pharmacies. A study in North East Scotland and East Anglia showed a similar trend whereby the mean overall cost per consultation was significantly lower for community pharmacies (£29.30) than general practitioner (£82.34) (Watson et al., 2015).
LIMITATIONS
The clinical outcomes of the consumers who received treatment for minor ailments were not assessed in this study. Besides, this study was conducted under a condition whereby there were no local guidelines to assist the community pharmacists in the management of minor ailment. Therefore, future study should focus on establishing and implementing guidelines or modules of practice for the minor ailments management in the Malaysian community pharmacy setting and evaluating the clinical outcomes of the treatment. Additionally, this study did not assess whether counseling was provided to the consumers for the minor ailment treatment. The provision of counseling during minor ailment needs to be evaluated in future study as well.
CONCLUSION
The community pharmacists actively managed the minor ailments by using a wide range of non-prescription medicines with affordable cost of treatment. Nevertheless, there was a lack of follow-up for the consumers who received the treatment. Therefore, guidelines, module of practices, and an audit system should be established to further improve the minor ailments management practices by the community pharmacists.
ACKNOWLEDGEMENT
The authors would like to thank all the participants for their willingness to participate in this study.
FINANCIAL SUPPORT
This work was supported by the Short-term Grant, Universiti Sains Malaysia (grant numbers 304/PFARMASI/6313014, 2013).
CONFLICTS OF INTEREST
The authors declared that they have no conflict of interest.
REFERENCES
Ayele AA, Mekuria AB, Tegegn HG, Gebresillassie BM, Mekonnen AB, Erku DA. Management of minor ailments in a community pharmacy setting: findings from simulated visits and qualitative study in Gondar town, Ethiopia. PLoS One, 2018; 13(1):e0190583. CrossRef
Babar ZUD, Ibrahim MIM. Affordability of medicines in Malaysia—consumer perceptions. Essent Drugs Monit, 2003; 33:18–9.
Benrimoj SC, Gilbert A, Quintrell N, Neto AC. Non-prescription medicines: a process for standards development and testing in community pharmacy. Pharm World Sci, 2007b; 29(4):386–94. CrossRef
Benrimoj SI, Wilson F. Standards for the provision of pharmacy medicines and pharmacist only medicines in community pharmacy. Pharmaceutical Society of Australia, Canberra, Australia, 2006 [Online]. Available via http://pharm-assist.com.au/wp-content/uploads/2017/05/PSA-s2s3-standards.pdf (Accessed 23 July 2019).
Benrimoj SI, Werner JB, Raffaele C, Roberts AS. A system for monitoring quality standards in the provision of non-prescription medicines from Australian community pharmacies. Pharm World Sci, 2008; 30(2):147–53. CrossRef
Benrimoj SI, Werner JB, Raffaele C, Roberts AS, Costa FA. Monitoring quality standards in the provision of non-prescription medicines from Australian Community Pharmacies: results of a national programme. Qual Safe Health Care, 2007a; 16(5):354–8. CrossRef
Bojke C, Gravelle H, Hassell K, Whittington Z. Increasing patient choice in primary care: the management of minor ailments. Health Econ, 2004; 13(1):73–86. CrossRef
Chong CP, Hassali MA, Bahari MB, Shafie AA. Generic medicines substitution practices among community pharmacists: a nationwide study from Malaysia. J Public Health, 2011; 19(1):81–90. CrossRef
Chua SS, Ramachandran CD, Paraidathathu TT. Response of community pharmacists to the presentation of back pain: a simulated patient study. Int J Pharm Pract, 2006; 14(3):171–8. CrossRef
Covington TR. Nonprescription drug therapy: issues and opportunities. Am J Pharm Educ, 2006; 70(6):137.
Hammad EA, Elayeh E, Tubelleh R, Watson M, Wazalty M. A simulated patient study assessing over the counter supply and counseling in Jordan: responding to headache complaints. Int J Clin Pharm, 2018; 40(5):982–6. CrossRef
Ibrahim IR, Palaian S, Ibrahim MI. Assessment of diarrhea treatment and counseling in community pharmacies in Baghdad, Iraq: a simulated patient study. Pharm Pract, 2018; 16(4):1313. CrossRef
Ismail IS. Proposal to raise private doctors' fees by RM30 to RM125. New Straits Times, 2018 [Online]. Available via https://www.nst.com.my/news/nation/2018/08/405344/proposal-raise-private-doctors-fees-rm30-rm125 (Accessed 23 July 2019).
Legal Research Board of Malaysia. Malaysian laws on poison and sales of drugs. International Law Books Services, Kuala Lumpur, Malaysia, 2006.
Lo YN. Consumers’ expectations of over the counter (OTC) medicines: location of sale. University of Saskatchewan, College of Graduate Studies and Research, Saskatoon, Canada, 2006.
Mackridge AJ, Stokes EC, Gray NJ. The use of community pharmacies in North West England: an observational study. Int J Pharm Pract, 2017; 25(2):172–5. CrossRef
Mansell K, Bootsman N, Kuntz A, Taylor J. Evaluating pharmacist prescribing for minor ailments. Int J Pharm Pract, 2015; 23(2):95–101. CrossRef
Merks P, Åšwieczkowski D, Jaguszewski MJ. Patients’ perception of pharmaceutical services available in a community pharmacy among patients living in a rural area of the United Kingdom. Pharm Pract, 2016; 14(3):774. CrossRef
Ministry of Health Malaysia. National Medicines Policy of Malaysia. Ministry of Health Malaysia, Kuala Lumpur, Malaysia, 2007.
Pharmaceuticals Services Division. First Schedule Poisons List [Section 2]. Ministry of Health Malaysia, Petaling Jaya, Malaysia, 2019 [Online]. Available via https://www.pharmacy.gov.my/v2/sites/default/files/document-upload/poisons-list-25.07.2019_1.pdf (Accessed 11 August 2019).
Sivanandam H, Carvalho M, Rahim R. Proposed medicine price control mechanism now in early stages, says Health Ministry. The Star Online, 2018 [Online]. Available via https://www.thestar.com.my/news/nation/2018/11/14/proposed-medicine-price-controlmechanism-now-in-early-stages-says-health-ministry/ (Accessed 23 July 2019).
Therapeutic Goods Administration. Australian Product Information. Betnovate (betamethasone valerate) cream, ointment & scalp application. Australian Government Department of Health, Canberra, Australia, 2019 [Online]. Available via https://www.ebs.tga.gov.au/ebs/picmi/picmirepository.nsf/pdf?OpenAgent&id=CP-2009-PI-00866-3&d=201907151016933 (Accessed 23 July 2019).
Watson MC, Ferguson J, Barton GR, Maskrey V, Blyth A, Paudyal V, Bond CM, Holland R, Porteous T, Sach TH, Wright D, Fielding S. A cohort study of influences, health outcomes and costs of patients' health-seeking behavior for minor ailments from primary and emergency care settings. BMJ Open, 2015; 5(2):e006261. CrossRef
William KA, Emmerton LM, Taylor R, Werner J, Benrimoj SI. Non-prescription medicines and Australian community pharmacy interventions: rates and clinical significance. Int J Pharm Pract, 2011; 19(3):156–65. CrossRef