INTRODUCTION
Schizophrenia is one of the serious psychiatric disorders with heterogeneous symptoms profile characterized by the presence of positive and negative symptoms, such as agitation, hallucinations, delusions, and lack of emotion. Antipsychotic medication is a key component to treat schizophrenia either to treat acute relapses of symptoms or to maintain therapy for relapse prevention, but the clinical use of these medicines differs in the management of first-episode schizophrenia in comparison to a relapse or recurrence of an established illness (Owen et al., 2016).
Pharmacotherapy with antipsychotic agents, in combination with adequate psychotherapy, is the key to effective schizophrenia treatment, according to the international guidelines such as the National Institute for Health and Care Excellence (NICE), the British Association for Psychopharmacology, or The Schizophrenia Patient Outcomes Research Team (PORT) (Gaebel et al., 2011).
However, the antipsychotic prescribing pattern for inpatients and outpatients varies widely in the daily practice. In many parts of the world, the second-generation antipsychotics (SGAs) are more frequently prescribed (Banergee et al., 2013; Park et al., 2014), while in other countries, first-generation antipsychotics (FGAs) are more frequently prescribed (Famuyiwa et al., 1983; Igbinomwanhia et al., 2017). There are no published data on the pattern of antipsychotic agents in Indonesia, particularly related to the rational use of antipsychotics. Inappropriate drug use will affect the effectiveness of the drug. It can increase the incidence of side effects and drug interactions as well as increases relapse rate and reduces recovery rate.
This study was aimed to discuss the treatment patterns of antipsychotics and clinical features of inpatients with schizophrenia. To our knowledge, this is the first report to discuss the treatment patterns of antipsychotics and clinical features of inpatients with schizophrenia at a tertiary hospital in Jakarta, Indonesia. The appropriateness of drug including appropriate indication, drug, patients, drug dose, and drug frequency are also analyzed and described.
METHODS
Study design and duration
This was a retrospective study and carried out in schizophrenic patients who were hospitalized at the Department of Psychiatry, Cipto Mangunkusumo Hospital, a tertiary teaching hospital located in Jakarta, in the period between July 2014 untill June 2015. We used data from the medical records.
Inclusion and exclusion criteria
The inclusion criteria for eligible inpatients were: diagnosed with psychotic disorders coded as F20–F29 based on the International Classification of Diseases 10th revision and aged between 16 and 65 years who had received antipsychotics therapy; while the exclusion criteria were patients with diagnosis of schizophrenia who were hospitalized ≤3 days and who were referred back to the unit or if their medical records were unreadable, incomplete data and unable to be traced. The study has been approved by the Faculty of Medicine, Universitas Indonesia Ethics Committee (No. 974/UN2.F1/ETIK/2015). All data were made anonymous for the research team with no possibility to identify any individual patient.
Sampling technique and sample size
In this study, we used consecutive sampling to recruit the study population. Therefore, all the patients who were hospitalized during those above periods and eligible according to inclusion criteria were included in this study. For calculating the sample size, we used the following formula:
n = Z2pq/e2
where n is the sample size, Z2 is the abscissa of the normal curve that cuts off an area α at the tails (95%), e is the desired level of precision (0.1), p is the estimated proportion of an attribute that is present in the population (50%), and q is 1 − p. From those above formula, the resulting sample size for our study is 97.
Data collection and instrument
We used data from medical records. The documented inpatient’s characteristics were sex, age, marital status, occupation, health insurance, diagnoses, length of hospitalization and suffering from schizophrenia, clinical outcome while the patients were discharged, and duration of hospitalization. All prescriptions were documented in the physiatric’s ward. The data were documented by using specific forms for the sake of this study.
Evaluation of rational use of antipsychotics
The evaluation of rational use of antipsychotics involved assessment of the appropriateness on the pattern of antipsychotic treatment including appropriate indication, drug, patient, drug dose, and drug frequency in schizophrenic patients according to the medical service standards at the Department of Psychiatry in Cipto Mangunkusumo Hospital or in line with the guidelines/consensus (Medical Guideline on The Management of Schizophrenia, Department of Psychiatry, Cipto Mangunkusumo Hospital (2015), (2nd Revised Edition) ; National Guideline on Psychiatry Services (2012); The Schizophrenia PORT: Updated Treatment Recommendations 2009 (Kreyenbuhl et al., 2010); and Guideline for Schizophrenia Treatment by NICE (2014) (NICE guideline for mental health and behavioral condition) .
Appropriate indication was defined as the accuracy of drug selection according to clinical signs and symptoms. Appropriate drug was defined as the accuracy to choose monotherapy or antipsychotic combination, accuracy to select the route of administration, no drug interaction, free of over-treatment or under-treatment and polypharmacy. Appropriate patient was defined as no contraindication and no history of allergy of certain antipsychotic. Appropriate drug dose defined as the drugs were given in the acceptable range dose. Finally, the appropriate drug dosing regimen was defined as the accuracy of drug dosing interval administered based on its half-life.
The assessment using Positive and Negative Syndrome Scale (PANSS) as an indicator of antipsychotic treatment outcome in schizophrenic patients was carried out at the beginning and at the end of hospitalization. The clinical condition of the patients at the end of hospitalization was considered as “stable/controlled” when the total score of PANSS assessment was ≤50%, in which the total score of PANSS was ±40.
Data analysis
The latest version of SPSS software was used to do the statistical analysis. Descriptive statistics were used to present the collected data.
RESULTS
A total of 113 inpatient’s medical records were collected. The average age was 43 years old (range: 16–63 years old). Sixty-two percent of the inpatients (N = 70) were male, 60% were single, and the majority of these patients (77%) were covered by the national health insurance scheme. Although more than 55% of the patients graduated from high school or university, majority of them (72%) were unemployed.
Ninety-nine percents of subjects (inpatients) were diagnosed with one of the following types of schizophrenia: paranoid schizophrenia (F20.0) (N = 101, 89%), hebephrenic schizophrenia (4.4%), and catatonic schizophrenia (1%).
There were 230 hospitalizations during 12-month period (from July 1, 2014 to June 30, 2015). In the above period, 26% of the inpatients were hospitalized twice, 23% hospitalized for the first time, while 51% of the inpatients were hospitalized three times or more (two patients were hospitalized for nine times). In average, inpatients hospitalized at the ward for 15 days (minimum 2 days and maximum 40 days). Most schizophrenic inpatients in Cipto Mangunkusumo hospital had clinical outcome of “stable/controlled” (66%) with a total PANSS score of ≤50%, in which total PANSS score was ±40 or the score of PANSS EC assessment of <4 for each item.
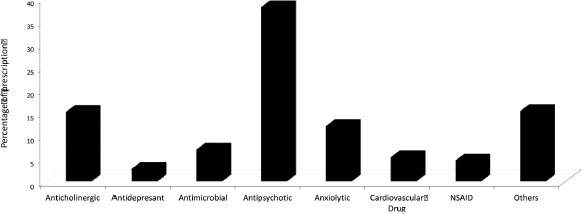 | Figure 1. Summary of drugs prescription (drugs prescribed pro re nata are not count). [Click here to view] |
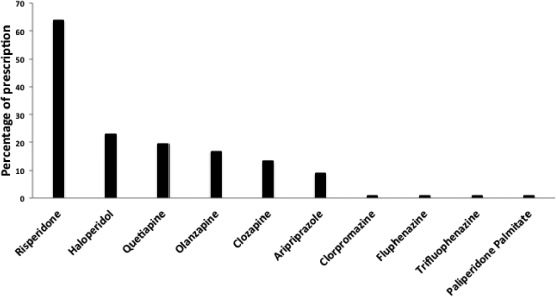 | Figure 2. The frequency of antipsychotics in prescription. [Click here to view] |
According to the Anatomical Therapeutic Chemical Classification index, a total of 350 medication prescriptions were analyzed. The frequently prescribed drugs were antipsychotics, antiparkinson, antianxiety agents, antidepressants, bipolar disorder agents, and cardiovascular agents (Fig. 1).
Among antipsychotics, the most frequently prescribed were risperidone (63.7%) followed by haloperidol (23%), quetiapine (19.5%), and olanzapine (16.8%). Most of the antipsychotic doses were in the suggested maintenance ranges (Fig. 2).
Side effects were recorded in 61 patients. This included extrapyramidal symptoms (N = 48; 78%), followed by weight gain (N = 6; 8%) and lipid abnormality (N = 5; 7%). All of those side effects were categorized as mild to moderate and healed spontaneously. Table 1 showed the profile of side effect of antipsychotic in all subjects. The most symptom of extra pyramidal reaction was tremor and mostly located in the extremities.
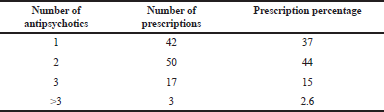
Sixty-two percent patients were given only one antipsychotic (monotherapy) and remaining were treated with at least two antipsychotics. Tables 2 and 3 describe the frequencies for the main combinations of antipsychotics and sum of antipsychotic in prescription. The most commonly used antipsychotics in combination with others were risperidone and haloperidol.
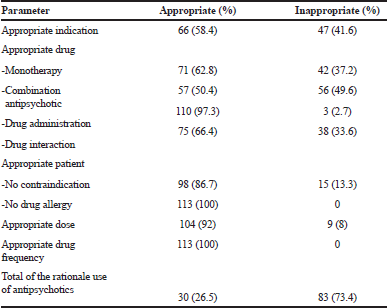
The rational use of antipsychotics consisted of appropriate indication, appropriate drug, appropriate patient, appropriate dose, and appropriate drug frequency of the study subjects is presented in the Table 4. Majority of inappropriateness caused by inaccuracy to choose an appropriate antipsychotic for combination or too early to combine the antipsychotics.
DISCUSSION
We describe and analyze the patterns of antipsychotics prescribed and clinical features in patients with schizophrenia who hospitalized in a teaching hospital in Jakarta, Indonesia. The evaluation of the appropriateness of antipsychotic treatment includes appropriate indication, appropriate drug, appropriate patient, appropriate drug dose, and appropriate drug frequency.
The frequency of male patients was higher than that of female patients (61.9% vs. 38.1%) in the population of the study observed, which is consistent with several previous studies. According to Lehman et al. (2004), the prognosis and course of illness in male patients are more severe compared to female patients; therefore, the symptoms appear faster and there are cultural factors affecting the great number of male patients as men are the breadwinner for their families resulting in greater burden for them compared to women.
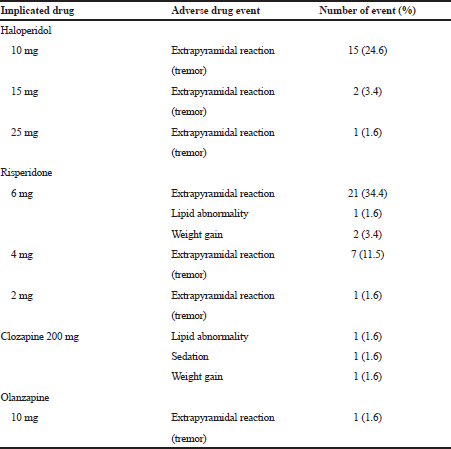 | Table 1. The common adverse drug events and implicated drug. [Click here to view] |
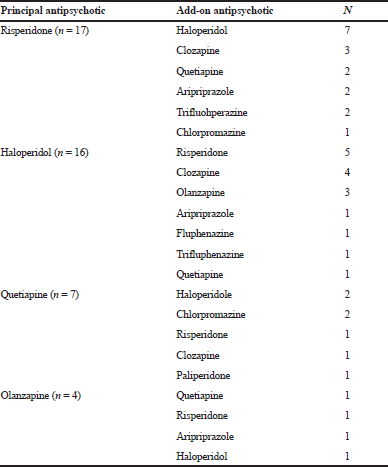 | Table 2. Polypharmacy for the four most common principal antipsychotic treatments. [Click here to view] |
Similar to other studies, we also found that inpatient schizophrenia mostly occurred at the aged of 26–45 years (58.4%). Since they were at reproductive and productive ages, it was likely to increase life burden as to fulfill their own needs and their family needs.
In this study period, the greatest number of patients were those who had paranoid schizophrenia (89.4%) with permanent paranoid delusion along with auditory hallucination that occurred in many patients, that is similar to the one reported by Ministry of Health, Republic of Indonesia, paranoid schizophrenia (F20.0.) is the most common diagnosis in the outpatient unit and ward in Indonesia (Riskesdas 2013). In addition, the length of hospital stay showing that the longest stay in schizophrenic patients was 15–21, which is consistent with the clinical pathway of schizophrenia at Cipto Mangunkusumo Hospital, that was stated the effective management of schizophrenia care is 21 days of hospitalization with a target of calmed patients and total score of PANSS of ≤50%, in which the total PANSS is ±40 or the score of PANSS EC assessment of <4 for each item. Moreover, according to patient’s clinical outcome the frequency distribution of the “calmed” was 66.4%, the “unstable/uncontrolled” clinical outcome was 27.4%, and discharge upon patient’s request was 6.2%. Most schizophrenic patients who were hospitalized in Cipto Mangunkusumo hospital had clinical outcome of “stable/controlled” with a total PANSS score of ≤50%, in which total PANSS score was ±40 or the score of PANSS EC assessment of <4 for each item (Cipto Mangunkusumo Clinical Pathway, 2015). For all hospital care, it is expected that the clinical outcome is “stable/controlled” as there are multiple factors causing “unstable/uncontrolled” clinical outcome; particularly the irrational use of drug treatment.
 | Table 3. Number of antipsychotics in prescription. [Click here to view] |
 | Table 4. The frequency of rationale use of antipsychotic. [Click here to view] |
According to this study result, the most commonly prescribed antipsychotics used was risperidone, since the hospitalized patients mostly had insurance and risperidone was the most common drug used in patients with insurance, particularly the Indonesia’s National Healthcare Insurance Program. Regarding the cost, risperidone is the cheapest SGA of benzioxazole class with the least extra-pyramidal side effects compared to other typical antipsychotics (Borison et al., 1992). Haloperidol decanoate (FGA long acting) was also frequently used since most patients had low compliance in taking medicine, therefore the long-term antipsychotic was given to achieve effective treatment (Nielsen et al., 2015). In addition, haloperidol injection was also frequently used to overcome acute symptoms such as irritability and restlessness using PANSS EC assessment as the indicator of acute treatment progress in schizophrenic patients (Huang et al., 2015).
Surprisingly, more than 40% of antipsychotic prescriptions were given to the patient without appropriate indication (41.6%). For appropriate indication, an evaluation should be performed when selecting antipsychotic treatment so that it is appropriate with the symptoms and consistent with the patient’s condition. According to the analysis of the study, inappropriate indication was mostly found in patients with an indication for clozapine treatment including symptoms of suicidal idea or behavior along with high score evaluation on suicidal risk, but the drug was not given (Pompili et al., 2016).
Contrary to the recommendations in the literature and Cipto Mangunkusomo hospital clinical pathway, the prescription frequency for antipsychotic monotherapy was low (37%), with most of the patients treated with antipsychotic combination and/or other adjunct psychiatric drugs.
Based on the schizophrenia clinical pathway in Cipto Mangunkusumo Hospital, monotherapy treatment should be given to all schizophrenic patients, either those who received treatment at the outpatient unit or those who were hospitalized in Cipto Mangunkusumo Hospital. Based on the European College of Neuropsychopharmacology guidelines on combination antipsychotics treatment and the frequent use of other psychiatric medications as described in Figure 1, might be interpreted by these argumentations (Goodwin et al., 2009): monotherapy partial response, the existence of concomitant symptoms other than those of the primary disorder, the combination therapy might increase tolerability by minimizing the adverse reactions of higher dose or there might be possible advantages from a de novo combination.
Combining antipsychotics with strong and weak D2 receptor binding properties with antipsychotics might result an optimal 70%–80% receptor occupancy, hypothetically (Seeman et al., 1998). In our study population, one of the examples of that type of combination was the common use of haloperidol with risperidone. In addition, high prevalence of affective and anxiety symptoms in patient with schizophrenia is shown in this study, so patients might get advantages from antidepressant and antianxiety agents treatment. Antipsychotic adverse effects such as symptoms of extrapyramidal might need anticholinergics treatment (Kopala, 1996). In our study, the use of co-treatment of antianxiety agent, antidepressants, and anticholinergic was common, that might be the reason for giving the combined treatment.
As the consequences of combined treatment in our study population, it was found the potential development of drug interaction in 22% subjects (data not shown). Most interaction occurred due to the administration of haloperidol and risperidone, which increased the risk of extrapyramidal disorder. Drug interaction in this study could also occur when the antipsychotics are given simultaneously with simvastatin as well as between azithromycin and some antipsychotics, in which theoretically it can inhibit the metabolism of antipsychotics resulting in increased effectiveness as well as the side effects of antipsychotics. It is expected that no drug interaction was found in antipsychotic treatment for all schizophrenic patients as it would affect drug effectiveness; therefore, an evaluation is necessary on antipsychotics that are more likely to have drug interaction with other drugs.
As shown in Table 1, the most common side effect due to antipsychotic treatment during hospitalization was extrapyramidal symptom, i.e., 77% of a total 61 adverse events. Extrapyramidal symptom (EPS) was the most common side effect found due to the use of risperidone at dose of 6 mg (34.4%) and due to the use of 10 mg of haloperidol (24.6%). Extrapyramidal symptoms occur with antipsychotics that block dopamine receptor in the post-synapse receptors of neurons in the brain, particularly in the limbic system and extrapyramidal system (Dopamine D2 receptor antagonists). It commonly occurs in typical antipsychotics, especially haloperidol compared to atypical antipsychotics except risperidone as it has stronger antagonist effect on dopamine receptor than other atypical antipsychotics (Meyer, 2011). In addition to EPS, other side effects found were lipid abnormality, obesity, abnormality and disorders of glucose, and sedation. These are consistent with the study conducted at Psychiatric Hospital in Slovenia which found extrapyramidal as the most common side effects (16%) of a total 100 patients, mostly caused by haloperidol, risperidone, or fluphenazine; followed by sedation and weight gain. Those adverse reactions of antipsychotics in that study were the main cause of switching antipsychotics (Bole et al., 2017). In this study, we collected data for adverse event from medical records. Since the adverse event’s data from medical record did not represent the real symptom of adverse events, the data from questionnaire are better. These issues were considered as a limitation of this study.
Crucial information which was shown in Table 3 described the sum of prescribed antipsychotics in each inpatient. We observed that our subjects were treated with one antipsychotic in 37% of prescriptions, two antipsychotics in 44% while three antipsychotics in 15% prescriptions were concomitantly prescribed. Surprisingly, more than three antipsychotics were prescribed concomitantly in 4% of prescriptions. This is not recommended based on guidelines from the British Association for Psychopharmacology, which pointed out that antipsychotics combination should be avoided unless in the case of replacing (Barnes, 2011). A recent study from Gaviria et al. showed that 70% patients were on antipsychotic combination, and 81.4% were on psychiatric treatments other than antipsychotics.
CONCLUSIONS
We present comprehensive prescribing patterns and clinical features for inpatients with schizophrenic disorder. We conclude that the medication in Cipto Mangunkusumo Hospital is not excellent for the following reasons: (1) combination treatment that induced high risk of clinically relevant drug interaction especially with psychotropic drugs; (2) more than 40% of antipsychotic prescriptions were administered without appropriate indication and mostly found in patients with an indication for clozapine treatment including symptoms of suicidal idea or behavior along with high score evaluation on suicidal risk, but the drug was not given; (3) more than 50% of inpatients received two or more antipsychotics concomitantly.
Psychiatrics are expected to be insightful of psychotropic drug interaction, adverse reactions, dosage, and mode of drug administration and the contribution of clinical pharmacology services to the psychiatrics could improve medication of inpatients with psychotic disorders, significantly.
ACKNOWLEDGMENTS
The authors would like to thank Melva Louisa for her encouragement, Fittria Pudjianty for her help with data collection, and the study participants for their assistance. The authors also thank all the clinicians for their contribution to this study.
CONFLICT OF INTEREST
No conflict of interest was declared.
ROLE OF FUNDING SOURCE
This study was funded by the research grant from Directorate of Research and Community Engagements Universitas Indonesia, Depok, Indonesia. The funding source did not play any role in the study design; the collection, analysis, and interpretation of data; or in the writing of the manuscript.
REFERENCES
Banerjee I, Roy B, Sathian B, Banerjee I, Chakraborty PK, Saha A. Socio demographic profile and utilization pattern of antipsychotic drugs among schizophrenic inpatients: a cross sectional study from western region of Nepal. BMC Psychiatry, 2013; 13:96. CrossRef
Barnes, TR, Paton C. Antipsychotic polypharmacy in schizophrenia: benefits and risks. CNS Drugs, 2011; 25:383–99. CrossRef
Bole CB, Pišlar M, šen M, TavÄar R, Mrhar A. Switching antipsychotics: results of 16-month non-interventional, prospective, observational clinical research of inpatients with schizophrenia spectrum disorders. Acta Pharm, 2017; 6:99–112. CrossRef
Borison RL, Pathiraja AP, Diamond BI, Meibach RC. Risperidone: clinical safety and efficacy in schizophrenia. Psychopharmacol Bull, 1992; 28:213–8.
Department of Psychiatry, Cipto Mangunkusumo Hospital, Guideline on “The Management of Schizophrenia,” 2015 (2nd Revised Edition). CrossRef
Famuyiwa OO. Psychotropic drug prescription in Nigeria. Acta Psychiatr Scand, 1983; 68:73–81. CrossRef
Gaebel W, Riesbeck M, Wobrock T. Schizophrenia guidelines across the world: a selective review and comparison. Int Rev Psychiatry, 2011; 23:379–87. CrossRef
Hálfdánarson Ó, Zoëga H, Aagaard L, Bernardo M, Brandt L, Fusté AC, et al. International trends in antipsychotic use: a study in 16 countries, 2005-2014. Eur Neuropsychopharmacol, 2017; 27:1064–76. CrossRef
Huang CL, Hwang TJ, Chen YH, Huang GH, Hsieh MH, Chen HH, et al. Intramuscular olanzapine versus intramuscular haloperidol plus lorazepam for the treatment of acute schizophrenia with agitation: an open-label, randomized controlled trial. J Formos Med Assoc, 2015; 114:438–45. CrossRef
Igbinomwanhia NG, Olotu SO, James BO. Prevalence and correlates of antipsychotic polypharmacy among outpatients with schizophrenia attending a tertiary psychiatric facility in Nigeria. Ther Adv Psychopharmacol, 2017; 7:3–10. CrossRef
Kopala LC. Spontaneous and drug-induced movement disorders in schizophrenia. Acta Psychiatr Scand Suppl, 1996; 389:12–7. CrossRef
Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB. Schizophrenia Patient Outcomes Research Team (PORT). The Schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2009. Schizophr Bull, 2010; 36:94–103. CrossRef
Lehman AF, Kreyenbuhl J, Buchanan RW, Dickerson FB, Dixon LB, Goldberg R, et al. The schizophrenia Patient Outcomes Research Team (PORT): updated treatment recommendations 2003. Schizophr Bull, 2004; 30:193–217. CrossRef
Meyer JM. Pharmacotherapy of psychosis and mania. In: Goodman, Gilman (eds.). The pharmacological basis of therapeutics. 2nd edition, McGraw-Hill, New York, NY, pp 409–39, 2011.
Nielsen J, Jensen, SO, Friis RB, Valentin JB. Correll CU. Comparative effectiveness of risperidone long-acting injectable vs first-generation antipsychotic long-acting injectables in schizophrenia: results from a nationwide, retrospective inception cohort study. Schizophr Bull, 2015; 41:627–36. CrossRef
National Guideline on Psychiatry Services. Indonesian Psychiatric Association, 2012.
NICE. Psychosis and schizophrenia in adults: treatment and management. Available via http://www.nice.org.uk/Guidance/CG178 (Accessed 29 September 2017).
Owen MJ, Sawa A, Mortensen PB. Schizophrenia. Lancet, 2016; 388:86–97. CrossRef
Park SC, Lee MS, Kang SG Lee SH. Patterns of antipsychotics prescription to patients with schizophrenia in Korea: results from the health insurance review & assessment service-national patient sample. J Korean Med Sci, 2014; 29:719–28. CrossRef
Pompili M, Baldessarini RJ, Forte A, Erbuto D, Serafini G, Fiorillo A, et al. Do atypical antipsychotics have antisuicidal effects? A hypothesis-generating overview. Int J Mol Sci, 2016; 17. CrossRef
Seeman P, Tallerico T. Antipsychotic drugs which elicit little or no parkinsonism bind more loosely than dopamine to brain D2 receptors, yet occupy high levels of these receptors. Mol Psychiatry, 1998; 3:123–34. CrossRef